Published online Jul 9, 2022. doi: 10.5409/wjcp.v11.i4.375
Peer-review started: July 29, 2021
First decision: November 11, 2021
Revised: December 17, 2021
Accepted: May 26, 2022
Article in press: May 26, 2022
Published online: July 9, 2022
Processing time: 341 Days and 19.1 Hours
Cardiovascular diseases have a high prevalence in adults and their development begins in the first decades of life. On the other hand, sports participation in childhood and adolescence provides benefits which can delay the onset of these diseases.
To synthesize the available literature on the impact of sports participation on cardiovascular outcomes in children and adolescents.
This systematic review was conducted on studies of children and adolescents (aged 8-18 years) who regularly practiced a sport and had reported cardiovascular outcomes (blood pressure and intima-media thickness) recorded. The Medline/PubMed, SciELO, Reference Citation Analysis (https://www.referencecitationanalysis.com/) and Bireme databases were searched.
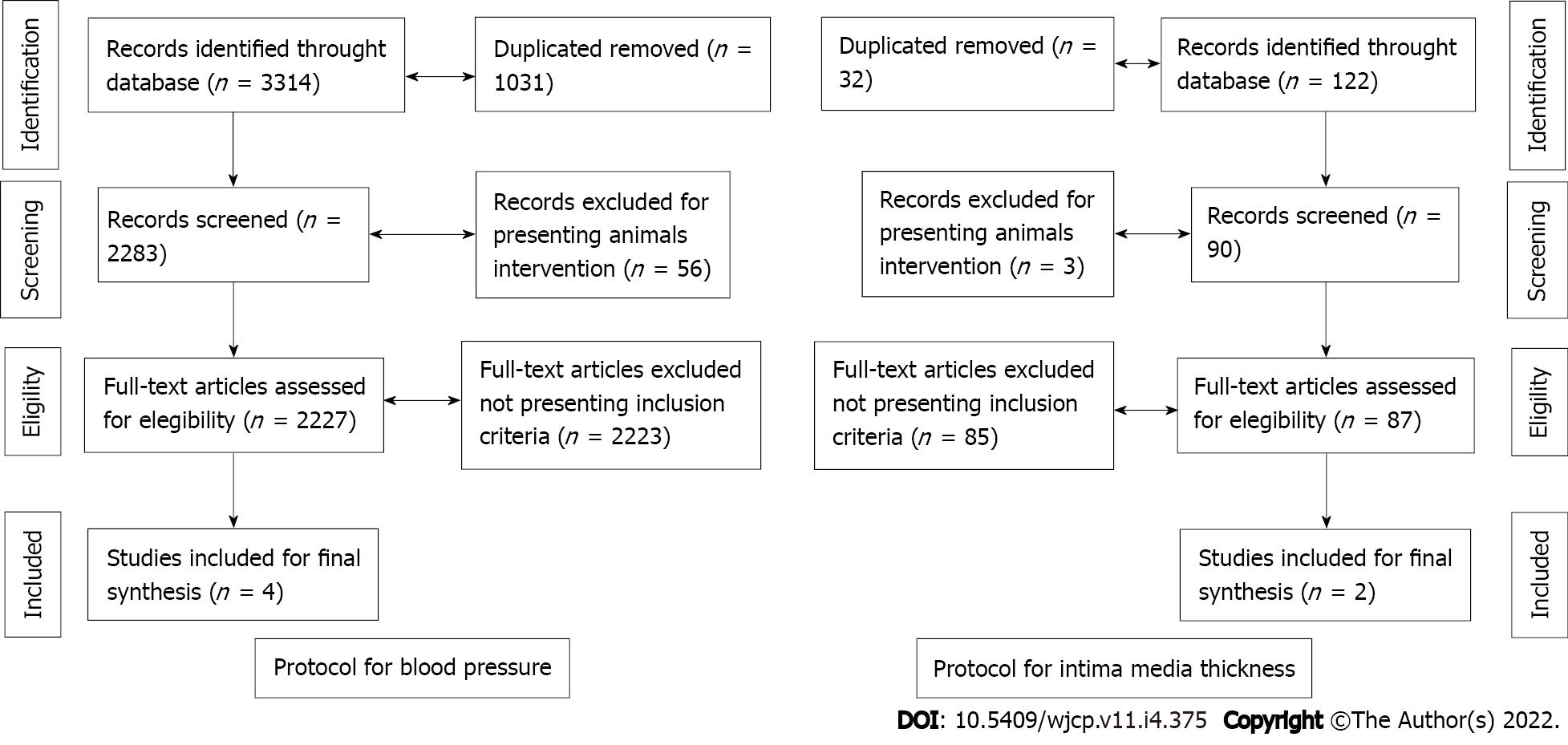
In total, 3314 publications for blood pressure and 122 publications for intima-media thickness were identified in the databases. After exclusions (e.g., duplicate articles, animal studies and those that did not meet the inclusion criteria), four publications for blood pressure (449 adolescents) and two publications for intima-media thickness were included (402 adolescents). For blood pressure, all publications were longitudinal in design (follow-up ranging from 12 wk to 12 mo) and involved adolescents aged from 8 years to 18 years of age. For intima-media thickness, both publications were longitudinal in design and involved adolescents aged from 11 years to 18 years of age.
Sports participation seems to promote benefits to cardiovascular structure and function in adolescents. However, studies with adolescents are scarce and further research is needed to understand this phenomenon.
Core Tip: Obesity, poor diet and a sedentary lifestyle increases the risk for cardiovascular disease in adulthood. On the other hand, sports participation reduces blood pressure and children and adolescents engaged in sports tend to present better arterial thickness values. In this way, those who practice sports regularly may present better cardiovascular health. In this review we seek to characterize the results of sports practice in adolescence on aspects related to cardiovascular health.
- Citation: Torres W, Maillane-Vanegas S, Urban JB, Fernandes RA. Impact of sports participation on cardiovascular health markers of children and adolescents: Systematic review and meta-analysis. World J Clin Pediatr 2022; 11(4): 375-384
- URL: https://www.wjgnet.com/2219-2808/full/v11/i4/375.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v11.i4.375
Cardiovascular diseases are the main cause of death among adults[1,2] with arterial hypertension being the most prevalent[3]. Although arterial hypertension is frequently observed in adults, high blood pressure is its manifestation in children and adolescents. In fact, the prevalence of high blood pressure in early life has increased in recent years[4,5] which is concerning for health professionals as it predicts mortality related to cardiovascular diseases in adulthood[6,7].
Blood pressure monitoring is a simple and useful way to screen cardiovascular problems in clinical practice. In addition, measures of intima-media thickness (IMT) also constitute a relevant marker of cardiovascular health, being a non-invasive method used to screen atherosclerosis[8,9].
Although the occurrence of cardiovascular diseases in children and adolescents is low, habits assumed in early life are able to affect health outcomes later in life[8,10]. Increased time spent in sedentary behavior[11] and insufficient physical activity[12] are behaviors that contribute to the development of cardiovascular diseases including arterial thickening[13].
Physical activity is a relevant behavior with huge potential to affect pediatric health. In terms of cardiovascular health, regular engagement in physical exercise helps to prevent a large variety of cardiovascular diseases in adulthood[14-18], but the effects in children and adolescents are still under investigation. Similarly, the pathways by which routines of physical exercise are able to promote cardiovascular health have been widely investigated in pediatric and adult groups[19], however, relevant questions still remain, mainly in pediatric groups.
For example, there are limited data about the impact of sports participation on cardiovascular health during adolescence. This question is relevant because in the real world (different from exercise protocols performed in the laboratory), sports participation is the main manifestation of physical exercise in adolescence helping adolescents to reach moderate-to-vigorous physical activity recommendations[20-23].
However, in the literature it is unclear whether engagement in sports is beneficial to the cardiovascular system in apparently healthy adolescents. Most publications involving physical exercise and cardiovascular aspects in adolescents are focused on obese groups and the exercise protocols rarely consider sports participation[24]. Thus, the objective of this review is to synthesize the available literature on the impact of sports participation on cardiovascular outcomes (blood pressure and IMT) in children and adolescents.
The present systematic review was conducted according to the Preferred reporting Items for Systematic Review and Meta-Analyses recommendations. The Problem was “sports participation and cardio
The main outcome of this review was to identify changes in systolic blood pressure (SBP) and diastolic blood pressure (DBP) (mmHg) and femoral and carotid IMT (mm) attributed to sports participation in children and adolescents. Due to the limited number of publications, there was no stratification according to sports.
Two authors independently performed the literature search from March to July 2021 and studies published until June 2021 were accessed. The search was restricted to publications in the following electronic databases: Medline/PubMed (National Library of Medicine), SciELO, Reference Citation Analysis (https://www.referencecitationanalysis.com/) and BIREME (Latin American and Caribbean Center on Health Sciences information). The search strategy considered the combination of nine keywords (DeCS): Children, adolescents, youth, teenagers, pediatrics, sports, sports participation, organized sports, blood pressure, intima-media thickness and vessel thickness, as follows.
Blood pressure: ((((((Children) OR (Adolescents)) OR (Youth)) OR (Teenagers)) OR (Pediatrics)) AND (((Sports) OR (Sports participation)) OR (Organized sport))) AND (Blood pressure).
Intima-media thickness: ((((((Children) OR (Adolescents)) OR (Youth)) OR (Teenagers)) OR (Pediatrics)) AND (((Sports) OR (Sports participation)) OR (Organized sport))) AND ((Intima-Media Thickness) OR (Vessel Thickness)).
In terms of language, only publications in English were considered. Data from reviews, expert opinions, case reports, editorials, rodent studies and computational studies were excluded. Cross-sectional studies were also excluded because the aim was to consider longitudinal studies that identified changes in blood pressure and IMT in adolescents engaged in sports. Finally, longitudinal studies that investigated adolescents (girls and boys) aged between 8 years and 18 years who were regularly engaged in any sport were considered eligible.
A standardized Cochrane Consumers and Communication Review Groups data extraction method was used, whereby the age of the participants, sample size, sex, sports participation definition and cardiovascular health marker outcomes (systolic blood pressure, diastolic blood pressure, carotid intima media thickness and femoral intima media thickness) were collated from each study.
Initially, two independent researchers (SMV and JBU) identified potential studies eligible for this review by screening titles and abstracts. Subsequently, the same reviewers observed the inclusion and exclusion criteria, assessed the full texts and extracted data from the included studies using a standardized extraction form. In case of discrepancy, another reviewer (WT) was available throughout the screening process to verify and resolve any issue.
The Newcastle-Ottawa quality assessment scale was used, which adopts a star system to assess the quality of eight items in three different domains (selection, comparability and exposure). Each item can receive one star, except for the comparability domain (two stars). The total score of the instrument ranges from 0 to 9[25].
In cases where standard error of the mean (SEM) and mean values for the intervention or control group were available, the SD was calculated using the following formula: SD = SEM × √n.
In cases where 95% confidence intervals (95%CI) were provided for the intervention or control group, the SD was calculated as follows: SD = √n × (upper limit - lower limit)/t statistic).
The meta-analysis was performed using Review Manager software (Version 5, Cochrane Collaboration). Differences in means and 95%CI were calculated using a continuous random-effect model to incorporate heterogeneity among studies. If the number of available studies was small (n ≤ 3), a fixed effect model was applied to estimate the between study heterogeneity.
Heterogeneity between studies was assessed using the chi square test expressed by means of inconsistency indices (I2) (0%–25%: None, 26%–50%: Low, 51%–75%: Moderate, and 76%–100%: High). Statistical significance was set at P < 0.05.
The research team searched for publications considering two outcomes, the impact of sports participation on blood pressure and IMT.
A total of 3436 relevant studies were identified in the databases. The majority of the studies assessed blood pressure [n = 3314 (96.4%)], while 122 (3.6%) assessed intima media thickness. After removal of duplicates and screening of study titles and abstracts, 2307 studies remained. Following the final full-text screening process, 4 studies for systolic and diastolic blood pressure (n = 326) and 2 studies for intima media thickness (n = 273) were included in the meta-analysis. The study selection process is presented in Figure 1.
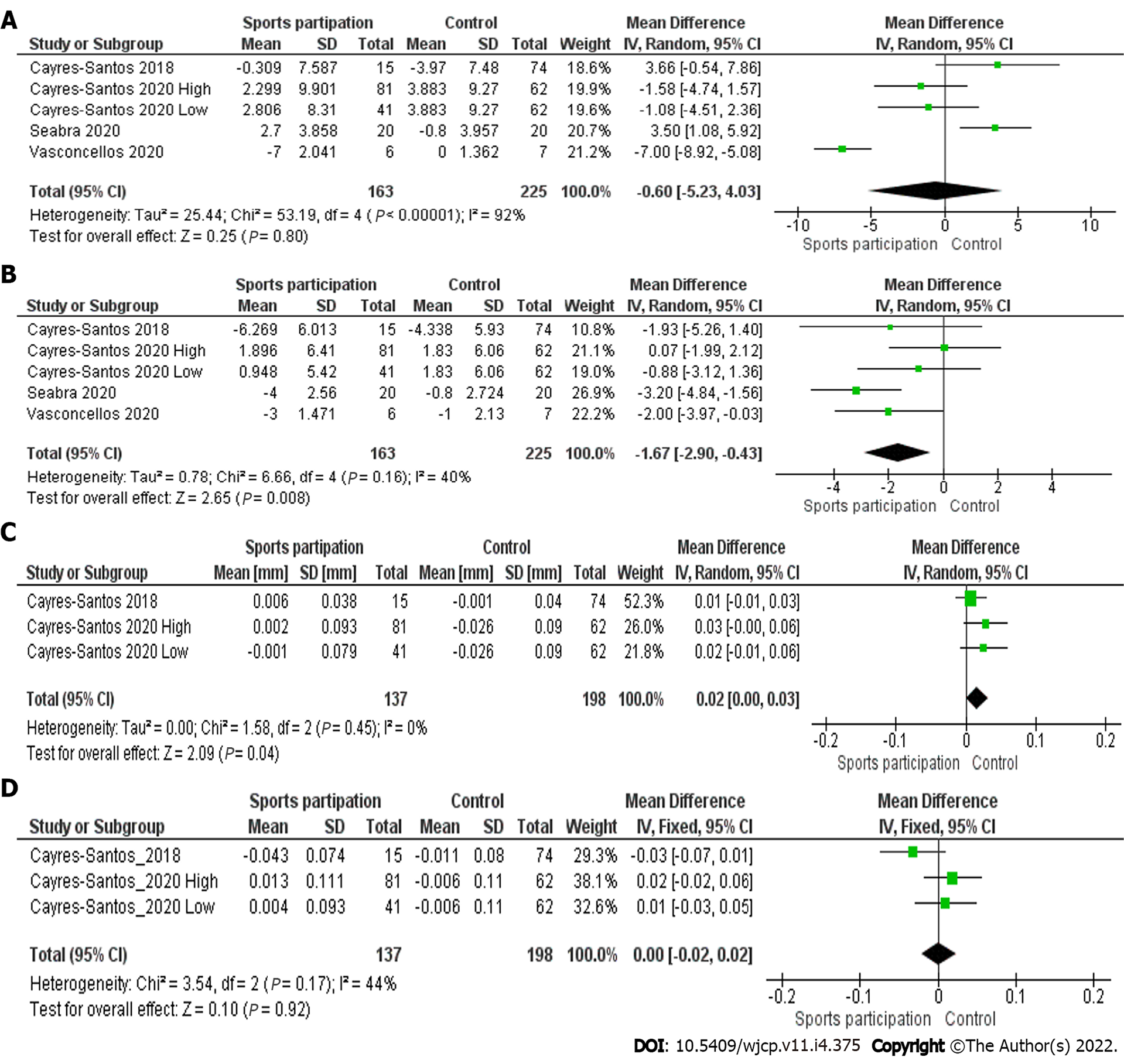
The characteristics of participants included in each study are presented in Table 1 for blood pressure and Table 2 for intima media thickness issues. Comparisons between the two groups (sports participation and control groups) are shown in Figure 2.
| Ref. | Title of paper | Aim/purpose | Total sample, n = 326 | Sample age | Follow-up time | Sports | Main results | Quality assessment1 |
| Cayres-Santos et al[29], 2020 | Sports participation improves metabolic profile in adolescents: ABCD growth study | To analyze the impact of participation in sports with different CRF demands on changes in metabolic and cardiovascular markers in adolescents | 184 adolescents (n = 122 engaged in sports and n = 62 not engaged in sports) | Between 11-18 | 12 mo | High CRF: Basketball, swimming, tennis, and track and field. Low CRF: Baseball, gymnastics, judo, karate, and kung fu | SBP increased in both sports with high [2.299 mmHg (95%CI: 0.142-4.456)) and low CRF [2.806 mmHg (95%CI: 0.261-5.351)]. DBP increased in sports with high [1.896 mmHg (95%CI: 0.499-3.293)], but not in sports with low CRF [0.948 mmHg (95%CI: -0.271 to 4.562)] | 7 |
| Cayres et al[30], 2018 | Sport-based physical activity recommendations and modifications in C-reactive protein and arterial thickness | We analyzed the effects of 1 yr of engagement in ≥ 300 min/wk of organized sports on inflammatory levels and vascular structure in adolescents | 89 adolescents (n = 15 sport practice and n = 74 non-sport practice) | Between 11-14 | 12 mo | Soccer, swimming, and others not shown | SBP did not change in the sports participation group [-0.309 mmHg (95%CI: -4.149 to 3.532)], but DBP did [-6.269 mmHg (95%CI: -9.313 to -3.224)] | 7 |
| Seabra et al[31], 2020 | School-based soccer practice is an effective strategy to improve cardiovascular and metabolic risk factors in overweight children | We examined the effects of a 6-mo school-based soccer program on CV and metabolic risk factors in overweight children | 40 overweight boys aged 8 to 12 yr (n = 20 soccer group and n = 20 control group) | Between 8–12 | 6 mo | Soccer | SBP did not change in the soccer group (2.7 mmHg), but DBP did (-4.0 mmHg) | 9 |
| Vasconcellos et al[26], 2021 | Does Recreational Soccer Change Metabolic Syndrome Status in Obese Adolescents? A Pilot Study | To evaluate whether a soccer program (RSP) might lower risk factors related to MetS in obese adolescents | 13 adolescents aged 13-17 yr (n = 6 soccer program and n = 7 control) | Between 12-17 | 12 wk | Soccer | SBP (-7.0 mmHg) and DBP (-3.0 mmHg) did not change significantly in the soccer group | 8 |
| Ref. | Title of paper | Aim/purpose | Total sample, n = 273 | Sample age | Follow-up time | Sports participation definition | Main results | Quality assessment1 |
| Cayres-Santos et al[29], 2020 | Sports participation improves metabolic profile in adolescents: ABCD growth study | To analyze the impact of participation in sports with different CRF demands on changes in metabolic and cardiovascular markers in adolescents | 184 adolescents (n = 122 engaged in sports and n = 62 not engaged in sports) | Between 11-18 | 12 mo | High CRF: Basketball, swimming, tennis, and track and field. Low CRF: Baseball, gymnastics, judo, karate, and kung fu | Carotid IMT did not change in both sports with high [0.002 mm (95%CI: -0.018 to 0.023)] and low CRF [-0.001 mm (95%CI: -0.024 to 0.023)]. Femoral IMT did not change in both sports with high [0.013 mm (95%CI: -0.010 to 0.037)] and low CRF [-0.004 mm (95%CI: -0.024 to 0.033)] | 8 |
| Cayres et al[30], 2018 | Sport-based physical activity recommendations and modifications in C-reactive protein and arterial thickness | We analyzed the effects of 1 yr of engagement in ≥ 300 min/wk of organized sports on inflammatory levels and vascular structure in adolescents | 89 adolescents (n = 15 Sport practice and n = 74 non-sport practice) | Between 11-14 | 12 mo | Soccer, swimming, and others not shown | Carotid IMT did not change in the sports participation group [0.006 mm (95%CI: -0.013 to 0.024)], but Femoral IMT did [-0.043 mm (95%CI: -0.081 to -0.006)] | 8 |
Blood pressure: The four publications included 326 adolescents aged from eight to 18 years (163 engaged in sports and 163 defined as control). All the studies had a longitudinal design and the findings are detailed in Table 1. The four publications varied according to the time of follow-up (ranging from 3 mo to 12 mo) and the sports considered included soccer, swimming, judo, karate, kung fu, gymnastics, basketball, track and field and baseball. All studies were published from 2018 to 2021.
In an individual way, studies did not show relevant changes through the follow-up for SBP and DBP. However, the meta-analysis model with the sum of all studies identified a decrease in DBP in favor of the sports participation group [-1.67 mmHg (95%CI: -2.90 to -0.43)].
IMT: The two papers included 402 adolescents aged from 11 years to 17 years. Both studies had a longitudinal design and the findings are detailed in Table 2. The studies were conducted between 2018 and 2020 and both recorded a 12-mo follow-up. No relevant changes were observed between sports participation and control groups in either the analysis of the individual results or in the meta-analysis model (Figure 2A and D).
All 6 studies that met the inclusion criteria and from which data were extracted, presented a quality rating between good (Cayres-Santos 2020 and 2018) and high quality (Seabra 2020 and Vasconcellos). All studies clearly defined the objectives, the participants included, inclusion/exclusion criteria adopted, independent variables, outcome measures and exposure status (sport), along with training history. No studies reported investigators being blinded to participant sport/training exposures.
The aims of this review were to synthesize and analyze the available literature about the impact of sports participation on cardiovascular outcomes in children and adolescents, particularly blood pressure and intima media thickness.
For blood pressure, only four studies met the inclusion criteria. The limited number of longitudinal studies considering the impact of sports participation on cardiovascular health of pediatric groups highlights the absence of data assessing the impact of physical exercise in the real world mainly because sports participation is the most common manifestation of physical exercise in the pediatric groups[22]. Most of the literature available on this issue relies on exercise protocols carried out in research laboratories and limits application in non-laboratorial settings.
In terms of findings, sports participation seems to be related to lower DBP. In fact, the beneficial impact of physical exercise on blood pressure of obese children and adolescents seems relevant but is still unclear in non-obese groups[26]. In fact, the pathways linking physical exercise and reductions in blood pressure strongly rely on the presence of obesity mainly due to its pro-inflammatory role in the organism[26]. The four included manuscripts considered children and adolescents with and without obesity which demonstrates the potential of sports participation to affect blood pressure in non-obese children and adolescents. However, the reduced number of manuscripts limits further interpretations of the findings.
For intima media thickness, sports participation was not significantly related to any modifications. Among adults, the literature recognizes that physical exercise improves the morphometry of arteries (arterial diameter increases improving dilation capacity which leads to reduced wall thickness)[27]. Thus, regular engagement in physical exercise is pointed out as effective in primary and secondary prevention strategies to reduce arterial wall thickness and arterial stiffness, especially in at-risk populations[27,28]. However, in our study with pediatric groups, both studies were carried out by the same research team and only cohort studies were found (no randomized clinical trials) which also limits further interpretations.
In terms of limitations, some aspects should be considered. First, our search was restricted only to the English language, not considering manuscripts published in different languages. Second, some relevant data in our meta-analysis (e.g., standard deviation of the difference) were estimated by the authors and not provided by the authors of the publication considered in the meta-analysis. Third, the reduced number of publications limits further inferences about the findings.
In summary, although sports participation seems to be related to improvements in blood pressure (diastolic), the literature assessing the impact of sports participation on cardiovascular health in children and adolescents is extremely scarce.
Adolescents are commonly engaged in sports but its impact on pediatric health is poorly explored in the literature.
There are many adolescents engaged in sports around the world and many organizations recommend sports participation as promoters of health among adolescents. However, little is known about its impacts on pediatric health.
To identify in the literature the potential benefits of sports participation on the cardiovascular health of children and adolescents.
We ran a systematic review with meta-analysis.
Sports participation is related to blood pressure but not related to intima-media thickness. However, the amount of literature about the issue is extremely scarce.
The literature assessing the impact of sports participation on cardiovascular health in children and adolescents is extremely scarce and it is unclear its impact on pediatric health.
We hope these findings will be useful to motivate researchers to expand the amount of data about the impact of sports participation on the cardiovascular health of pediatric groups.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pediatrics
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abdelbasset WK, Saudi Arabia A-Editor: Yao QG, China S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Urbina EM, Williams RV, Alpert BS, Collins RT, Daniels SR, Hayman L, Jacobson M, Mahoney L, Mietus-Snyder M, Rocchini A, Steinberger J, McCrindle B; American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young. Noninvasive assessment of subclinical atherosclerosis in children and adolescents: recommendations for standard assessment for clinical research: a scientific statement from the American Heart Association. Hypertension. 2009;54:919-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 451] [Cited by in RCA: 492] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 2. | Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747-1757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3532] [Cited by in RCA: 3494] [Article Influence: 183.9] [Reference Citation Analysis (0)] |
| 3. | Ewald DR, Haldeman PhD LA. Risk Factors in Adolescent Hypertension. Glob Pediatr Health. 2016;3:2333794X15625159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | Magalhaes MG, Oliveira LM, Christofaro DG, Ritti-Dias RM. Prevalence of high blood pressure in Brazilian adolescents and quality of the employed methodological procedures: systematic review. Rev Bras Epidemiol. 2013;16:849-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Song P, Zhang Y, Yu J, Zha M, Zhu Y, Rahimi K, Rudan I. Global Prevalence of Hypertension in Children: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019;173:1154-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 411] [Article Influence: 68.5] [Reference Citation Analysis (0)] |
| 6. | Sundström J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ. 2011;342:d643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 178] [Cited by in RCA: 193] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 7. | Berge HM, Isern CB, Berge E. Blood pressure and hypertension in athletes: a systematic review. Br J Sports Med. 2015;49:716-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Guven B, Demirpence S, Yilmazer MM, Carti OU, Tavli V, Mese T, Oner T. Arterial function and anatomy in obese children with cardiovascular risk factors. Pediatr Int. 2013;55:696-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Shah PK. Inflammation, infection and atherosclerosis. Trends Cardiovasc Med. 2019;29:468-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 76] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 10. | Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139:e56-e528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4294] [Cited by in RCA: 5867] [Article Influence: 977.8] [Reference Citation Analysis (5)] |
| 11. | Guerra PH, de Farias Júnior JC, Florindo AA. Sedentary behavior in Brazilian children and adolescents: a systematic review. Rev Saude Publica. 2016;50:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Monteiro AR, Dumith SC, Gonçalves TS, Cesar JA. [Overweight among young people in a city in the Brazilian semiarid region: a population-based study]. Cien Saude Colet. 2016;21:1157-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Baroncini LAV, Sylvestre LC, Baroncini CV, Pecoits R Filho. Assessment of Carotid Intima-Media Thickness as an Early Marker Of Vascular Damage In Hypertensive Children. Arq Bras Cardiol. 2017;108:452-457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423-1434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3281] [Cited by in RCA: 3229] [Article Influence: 179.4] [Reference Citation Analysis (0)] |
| 15. | McGill HC Jr, McMahan CA, Herderick EE, Malcom GT, Tracy RE, Strong JP. Origin of atherosclerosis in childhood and adolescence. Am J Clin Nutr. 2000;72:1307S-1315S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 348] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 16. | World Health Organization (WHO). Global Action Plan for the Prevention and Control of NCDs 2013-2020. [cited 10 June 2021]. Available from: https://www.who.int/publications/i/item/9789241506236. |
| 17. | NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627-2642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4848] [Cited by in RCA: 4666] [Article Influence: 583.3] [Reference Citation Analysis (2)] |
| 18. | Gao Z, Khoury PR, McCoy CE, Shah AS, Kimball TR, Dolan LM, Urbina EM. Adiposity has no direct effect on carotid intima-media thickness in adolescents and young adults: Use of structural equation modeling to elucidate indirect & direct pathways. Atherosclerosis. 2016;246:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Cayres SU, Vanderlei LC, Silva DR, Lima MC, Barbosa MF, Fernandes RA. Cardiovascular and metabolic risk markers are related to parasympathetic indices in pre-pubertal adolescents. Cardiol Young. 2016;26:280-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | CDC. How much physical activity do adults need?|Physical Activity|CDC. Center for Diesease Control and Prevention 2015: 1. [cited 10 June 2021]. Available from: https://www.cdc.gov/physicalactivity/basics/index.htm. |
| 21. | Hallal PC, Victora CG, Azevedo MR, Wells JC. Adolescent physical activity and health: a systematic review. Sports Med. 2006;36:1019-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 494] [Cited by in RCA: 490] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 22. | Hulteen RM, Smith JJ, Morgan PJ, Barnett LM, Hallal PC, Colyvas K, Lubans DR. Global participation in sport and leisure-time physical activities: A systematic review and meta-analysis. Prev Med. 2017;95:14-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 313] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 23. | Pahkala K, Hietalampi H, Laitinen TT, Viikari JS, Rönnemaa T, Niinikoski H, Lagström H, Talvia S, Jula A, Heinonen OJ, Juonala M, Simell O, Raitakari OT. Ideal cardiovascular health in adolescence: effect of lifestyle intervention and association with vascular intima-media thickness and elasticity (the Special Turku Coronary Risk Factor Intervention Project for Children [STRIP] study). Circulation. 2013;127:2088-2096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 136] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 24. | García-Hermoso A, Ceballos-Ceballos RJ, Poblete-Aro CE, Hackney AC, Mota J, Ramírez-Vélez R. Exercise, adipokines and pediatric obesity: a meta-analysis of randomized controlled trials. Int J Obes (Lond). 2017;41:475-482. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 25. | Wells G, Shea B, Robertson J, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analysis. [cited 10 June 2021]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. |
| 26. | Vasconcellos F, Cunha FA, Gonet DT, Farinatti PTV. Does Recreational Soccer Change Metabolic Syndrome Status in Obese Adolescents? Res Q Exerc Sport. 2021;92:91-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 27. | Green DJ, Hopman MT, Padilla J, Laughlin MH, Thijssen DH. Vascular Adaptation to Exercise in Humans: Role of Hemodynamic Stimuli. Physiol Rev. 2017;97:495-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 335] [Cited by in RCA: 500] [Article Influence: 62.5] [Reference Citation Analysis (0)] |
| 28. | Baumgartner L, Weberruß H, Appel K, Engl T, Goeder D, Oberhoffer-Fritz R, Schulz T. Improved Carotid Elasticity but Altered Central Hemodynamics and Carotid Structure in Young Athletes. Front Sports Act Living. 2021;3:633873. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Cayres-Santos SU, Urban JB, Barbosa MF, Lemes IR, Kemper HCG, Fernandes RA. Sports participation improves metabolic profile in adolescents: ABCD growth study. Am J Hum Biol. 2020;32:e23387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Cayres SU, de Lira FS, Kemper HCG, Codogno JS, Barbosa MF, Fernandes RA. Sport-based physical activity recommendations and modifications in C-reactive protein and arterial thickness. Eur J Pediatr. 2018;177:551-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Seabra A, Brito J, Figueiredo P, Beirão L, Seabra A, Carvalho MJ, Abreu S, Vale S, Pedretti A, Nascimento H, Belo L, Rêgo C. School-based soccer practice is an effective strategy to improve cardiovascular and metabolic risk factors in overweight children. Prog Cardiovasc Dis. 2020;63:807-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |