Published online Jul 9, 2021. doi: 10.5409/wjcp.v10.i4.79
Peer-review started: December 30, 2020
First decision: May 6, 2021
Revised: May 11, 2021
Accepted: June 4, 2021
Article in press: June 4, 2021
Published online: July 9, 2021
Processing time: 188 Days and 15.6 Hours
Circumcision refers to the removal of the skin covering the tip of the penis and is one of the most common surgical procedures performed in childhood. Even though circumcision is a well-standardized operation, several minor and major complications may be experienced by paediatric surgeons. Glans ischemia (GI) has been widely reported in the paediatric literature as a complication following circumcision. Nonetheless, etiopathogenesis of GI is not well defined and mana
We describe our experience with this rare and scary complication using sub
Hypothetical causes and different management strategies are discussed.
Core Tip: Glans ischemia (GI) after circumcision is a rare complication, which has been widely described by paediatric surgeons in the modern literature. To date, etiopathogenesis of GI is not well defined and management guidelines are lacking. In order to achieve a prompt diagnosis and to start appropriate treatment, an accurate postope
- Citation: Codrich D, Boscarelli A, Cerrina A, Scarpa MG, Iaquinto M, Olenik D, Guida E, Schleef J. Glans ischemia after circumcision in children: Two case reports. World J Clin Pediatr 2021; 10(4): 79-83
- URL: https://www.wjgnet.com/2219-2808/full/v10/i4/79.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v10.i4.79
Circumcision refers to the surgical removal of the foreskin covering the glans and is one of the most common paediatric procedures. The complication rate after circumcision in childhood varies between 0% and 16%[1]. Minor complications include penile shaft swelling, bleeding, meatal stenosis, recurrent preputial stenosis and unsatisfactory cosmetic appearance. Major complications reported in the literature are glans or penile amputation, septicaemia, and urethrocutaneous fistulas[1,2]. Glans ischemia (GI) after circumcision is an extremely rare but scary complication in children[3]. We describe our experience with two cases of GI after circumcision in males aged 8 and 10 years old. Hypothetical causes and different treatment strategies are debated.
Case 1: An 8-year-old boy underwent circumcision at our paediatric surgery depart
Case 2: A 10-year-old boy presented to our paediatric outpatient clinic for a true phimosis. Personal history was unremarkable, except for childhood vitiligo. Circumcision was performed under general sedation with spinal anaesthesia. Bipolar electrocautery was used and coronal suture was performed with 5-0 interrupted absorbable stitches. No compressive bandaging was applied. No excessive bleeding was noted neither during intervention nor in the immediate postoperative course. Minimum glans swelling was reported two hours after surgery.
Phimosis.
Case 1: Uneventful.
Case 2: Unremarkable, except for childhood vitiligo.
Unremarkable.
At the clinical examination 6 h after surgery, an ischemic appearance of the glans was documented, without pain or difficulty to urinate. A colour doppler imaging (CDI) showed normal flow in the dorsal penile artery.
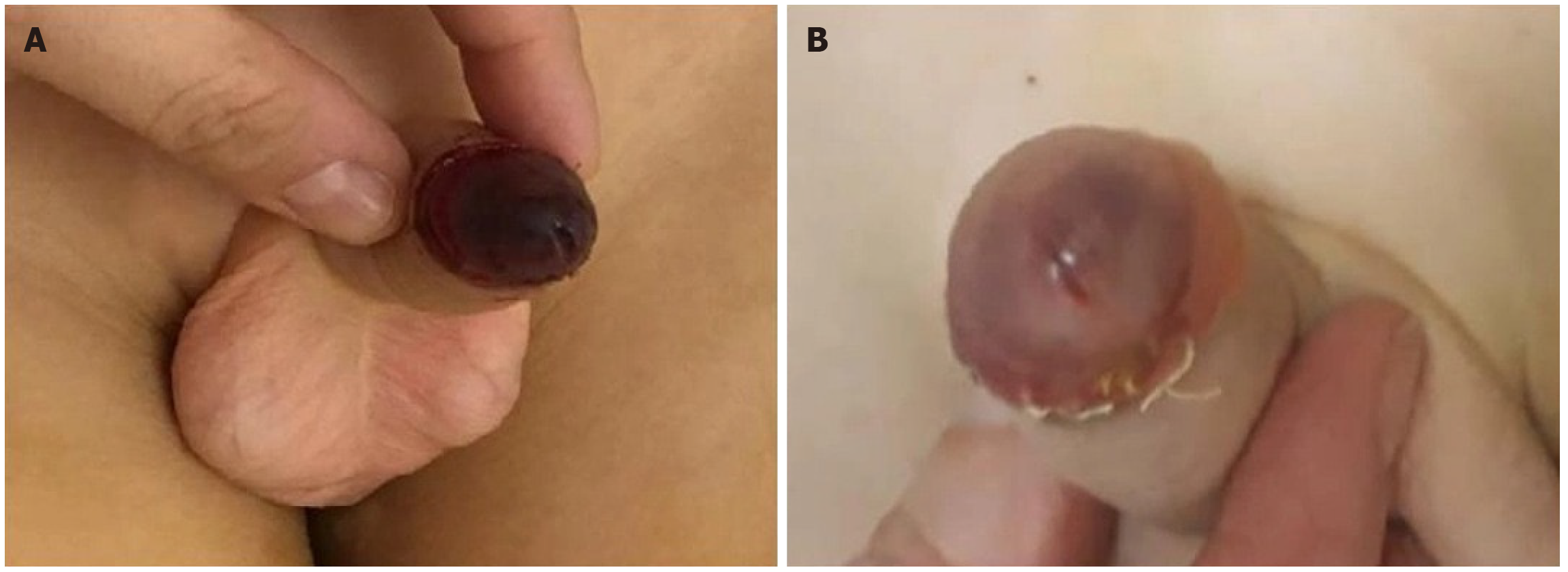
Four hours after surgery, an ischemic appearance of the glans was documented (Figure 1A). Whole blood count and blood clotting were checked and found to be within normal ranges.
Subcutaneous enoxaparin 2000 UI injection was started and continued once a day for 5 d. Moreover, a galenic preparation of nitric oxide ointment was applied on the glans once a day for a week.
Anticoagulant therapy was started with subcutaneous enoxaparin 3000 UI once a day for 5 d.
The child was discharged home on postoperative day 6 when an improvement of the GI was noted. Complete restitution integrum was achieved one month after surgery.
The colour of the glans rapidly improved to reddish (Figure 1B), and the patient was discharged home on postoperative day 4. At one-month follow-up, the penis and glans were found to be in a normal status.
Circumcision is a common paediatric surgical procedure; approximately 0.5% of patients require a repeat surgery. The most frequent complication reported in patients undergoing circumcision is haemorrhage (0.8%), with more than 60% of cases requiring surgical revision[2].
GI after circumcision has been widely reported in the paediatric literature. How
To date, several treatment options for GI are reported in the literature, but a defined protocol or guidelines are still lacking. Some authors reported a successful outcome with endovenous or oral administration of pentoxifylline (PTX), alone or in association with other therapeutic stratagems. PTX is a hemorheological agent which improves the viscosity of blood and is used in peripheral vascular and cerebrovascular insufficiency[4,9,10]. Comparatively, caudal block reduces sympathetic tone, improves arterial supply and venous drainage, and has been proposed as the sole therapeutic strategy[7], or in association with intracavernous injection of glycerol trinitrate, to improve postarteriolar smooth muscle relaxation[11]. Furthermore, Aminsharifi et al[11] repor
In conclusion, although a unique causative factor for GI after circumcision cannot be identified, a favourable outcome has been reported in nearly all cases. The unfavourable outcomes reported in literature are due to delayed discovery of the ischemic condition or late presentation of the patients back to the hospital. Conse
Manuscript source: Invited manuscript
Specialty type: Surgery
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hosseini MS S-Editor: Zhang L L-Editor: A P-Editor: Wang LYT
| 1. | Weiss HA, Larke N, Halperin D, Schenker I. Complications of circumcision in male neonates, infants and children: a systematic review. BMC Urol. 2010;10:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 236] [Cited by in RCA: 211] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 2. | Cathcart P, Nuttall M, van der Meulen J, Emberton M, Kenny SE. Trends in paediatric circumcision and its complications in England between 1997 and 2003. Br J Surg. 2006;93:885-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 58] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Ozzeybek D, Koca U, Elar Z, Olguner M, Hakgüder G. Glycerol trinitrate plus epidural sympathetic block in the ischemia of glans penis. Anesth Analg. 1999;89:1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Karaguzel E, Tok DS, Kazaz IO, Gur M, Colak F, Kutlu O, Ozgur GK. Postcircumcisional ischemia of the glans penis treated with pentoxifylline. Case Rep Urol. 2013;2013:278523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Efe E, Resim S, Bulut BB, Eren M, Garipardic M, Ozkan F, Ozkan KU. Successful treatment with enoxaparin of glans ischemia due to local anesthesia after circumcision. Pediatrics. 2013;131:e608-e611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Gnatzy R, Fuchs J, Siekmeyer M, Beeskow AB, Gosemann JH, Lacher M. Glans Ischemia after Circumcision in a 16-Year-Old Boy: Full Recovery after Angiography with Local Spasmolysis, Systemic Vasodilatation, and Anticoagulation. European J Pediatr Surg Rep. 2018;6:e66-e69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Kaplanian S, Chambers NA, Forsyth I. Caudal anaesthesia as a treatment for penile ischaemia following circumcision. Anaesthesia. 2007;62:741-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Sterenberg N, Golan J, Ben-Hur N. Necrosis of the glans penis following neonatal circumcision. Plast Reconstr Surg. 1981;68:237-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Cárdenas Elías MÁ, Vázquez Rueda F, Jiménez Crespo V, Siu Uribe A, Murcia Pascual FJ, Betancourth Alvarenga JE, Paredes Esteban RM. [An unexpected complication: glans ischemia after circumcision. Review of the literature]. Cir Pediatr. 2016;29:127-130. [PubMed] |
| 10. | Aslan A, Karagüzel G, Melikoglu M. Severe ischemia of the glans penis following circumcision: a successful treatment via pentoxifylline. Int J Urol. 2005;12:705-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Aminsharifi A, Afsar F, Tourchi A. Delayed glans necrosis after circumcision: role of testosterone in salvaging glans. Indian J Pediatr. 2013;80:791-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |