Copyright
©The Author(s) 2017.
World J Clin Pediatr. May 8, 2017; 6(2): 110-117
Published online May 8, 2017. doi: 10.5409/wjcp.v6.i2.110
Published online May 8, 2017. doi: 10.5409/wjcp.v6.i2.110
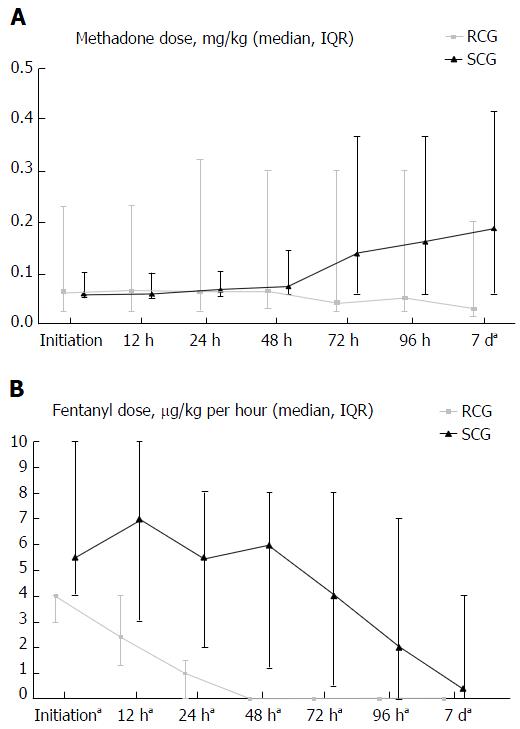
Figure 1 Comparison of enteral methadone and intravenous fentanyl titration across groups in the study.
A: Paired comparison of median enteral methadone doses (mg/kg) between rapid conversion group and slow conversion group at serial time points following initiation of enteral methadone (aP < 0.05); B: Paired comparison of median intravenous fentanyl infusion doses (μg/kg per hour) between rapid conversion group and slow conversion group at serial time points following initiation of enteral methadone (aP < 0.05). RCG: Rapid conversion group consisted of patients who were completely converted from fentanyl infusion directly to enteral methadone in 48 h or less; SCG: Slow conversion group consisted of patients who were completely converted from fentanyl infusion directly to enteral methadone in more than 48 h.
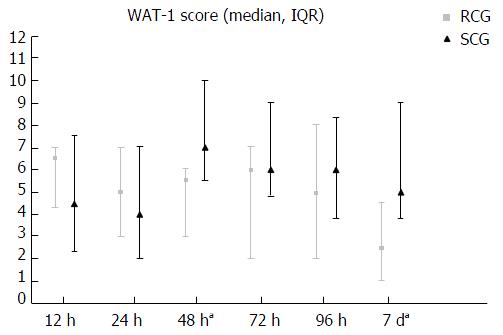
Figure 2 Paired comparison of median withdrawal (Withdrawal Assessment Tool-Version 1) scores between rapid conversion group and slow conversion group at serial time points following initiation of enteral methadone (aP < 0.
05). RCG: Rapid conversion group consisted of patients who were completely converted from fentanyl infusion directly to enteral methadone in 48 h or less; SCG: Slow conversion group consisted of patients who were completely converted from fentanyl infusion directly to enteral methadone in more than 48 h. WAT-1: Withdrawal Assessment Tool-Version 1.
- Citation: Srinivasan V, Pung D, O’Neill SP. Conversion from prolonged intravenous fentanyl infusion to enteral methadone in critically ill children. World J Clin Pediatr 2017; 6(2): 110-117
- URL: https://www.wjgnet.com/2219-2808/full/v6/i2/110.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v6.i2.110