Copyright
©The Author(s) 2023.
World J Clin Pediatr. Dec 9, 2023; 12(5): 331-349
Published online Dec 9, 2023. doi: 10.5409/wjcp.v12.i5.331
Published online Dec 9, 2023. doi: 10.5409/wjcp.v12.i5.331
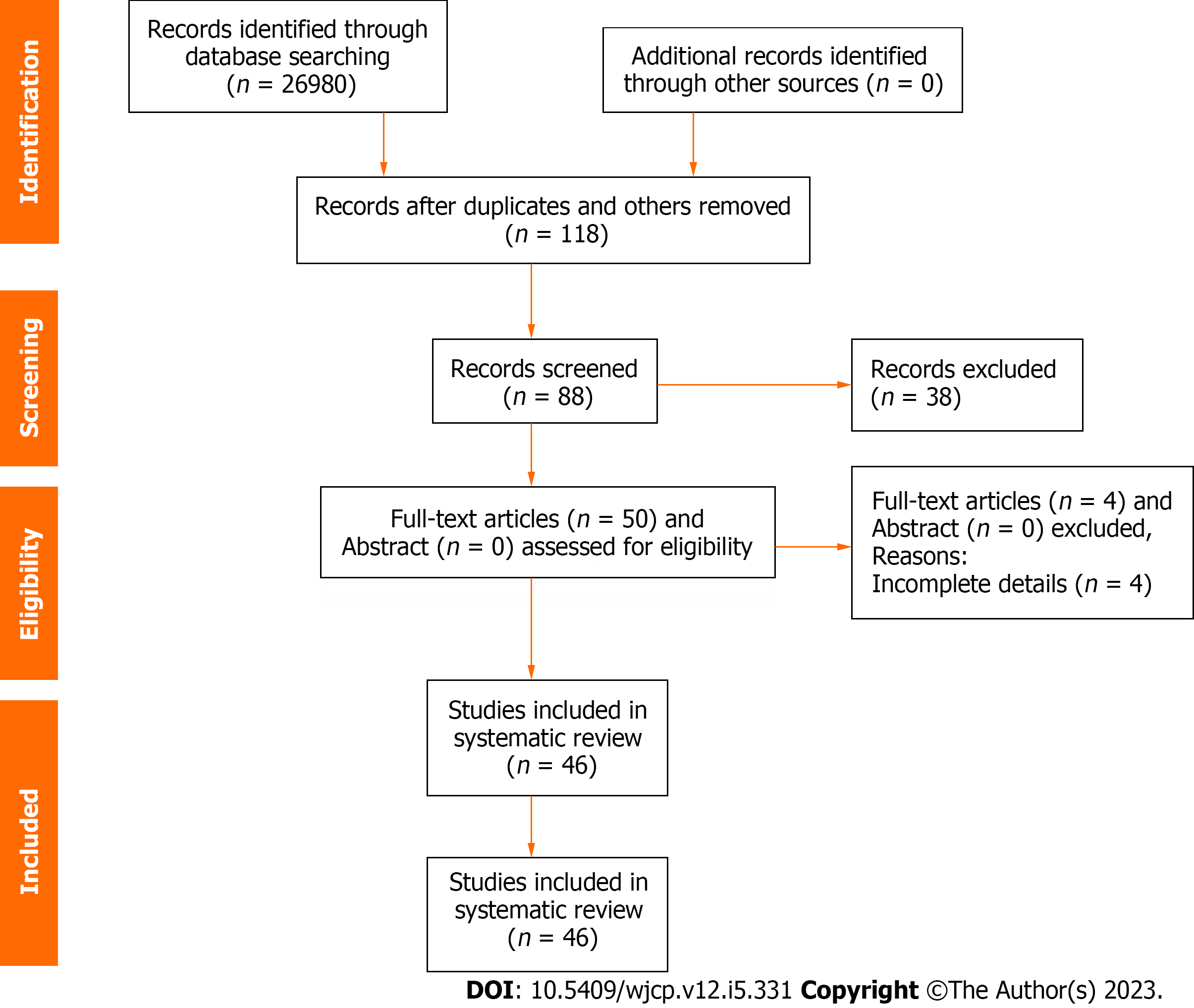
Figure 1 Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram for manuscripts screening and selection for the systematic review of the management of migration of the distal ventriculoperitoneal shunt catheter into the stomach with or without trans-oral extrusion.
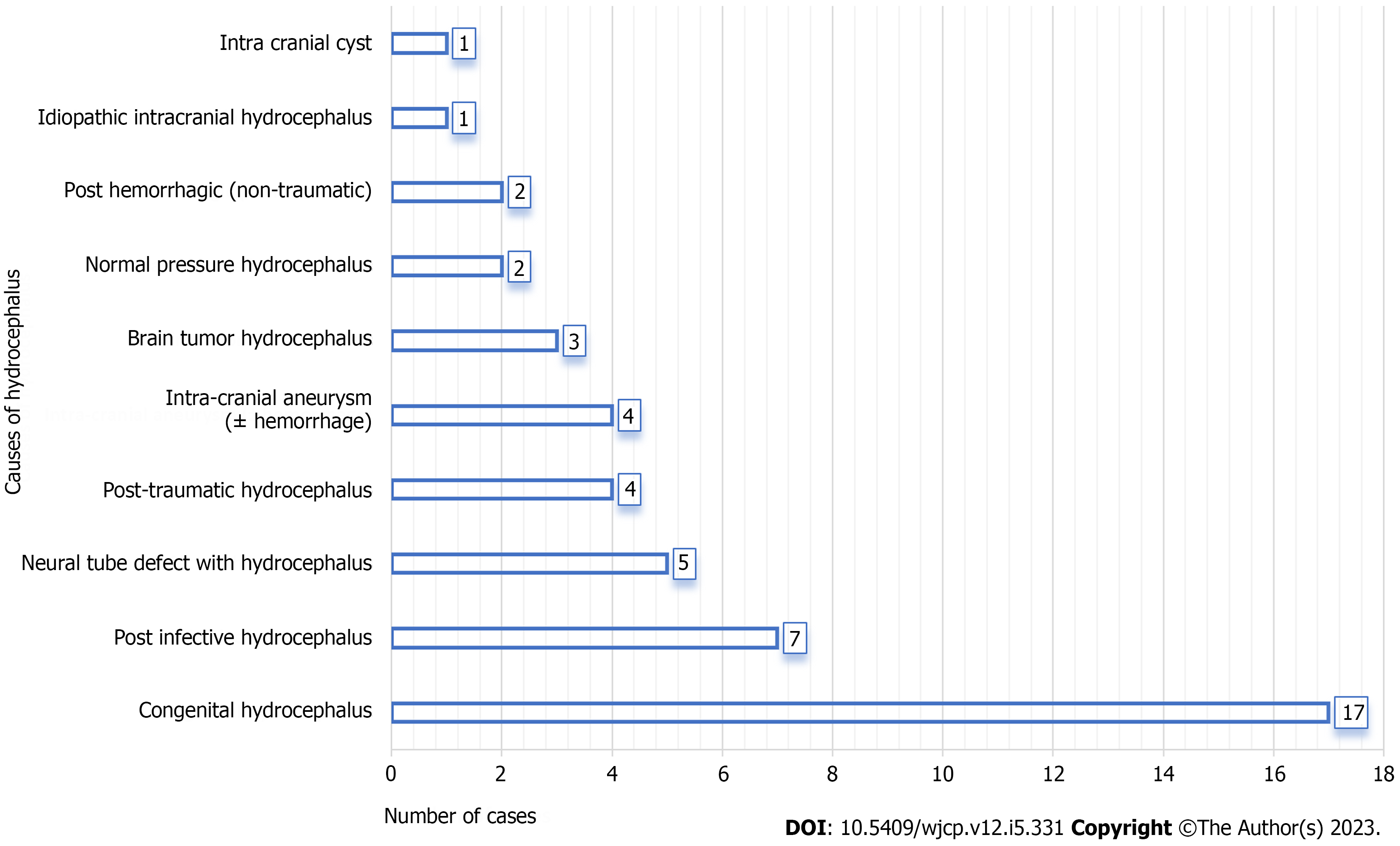
Figure 2 Indication (causes of hydrocephalus) for primary ventriculoperitoneal shunt insertion for entire cases (n = 46).
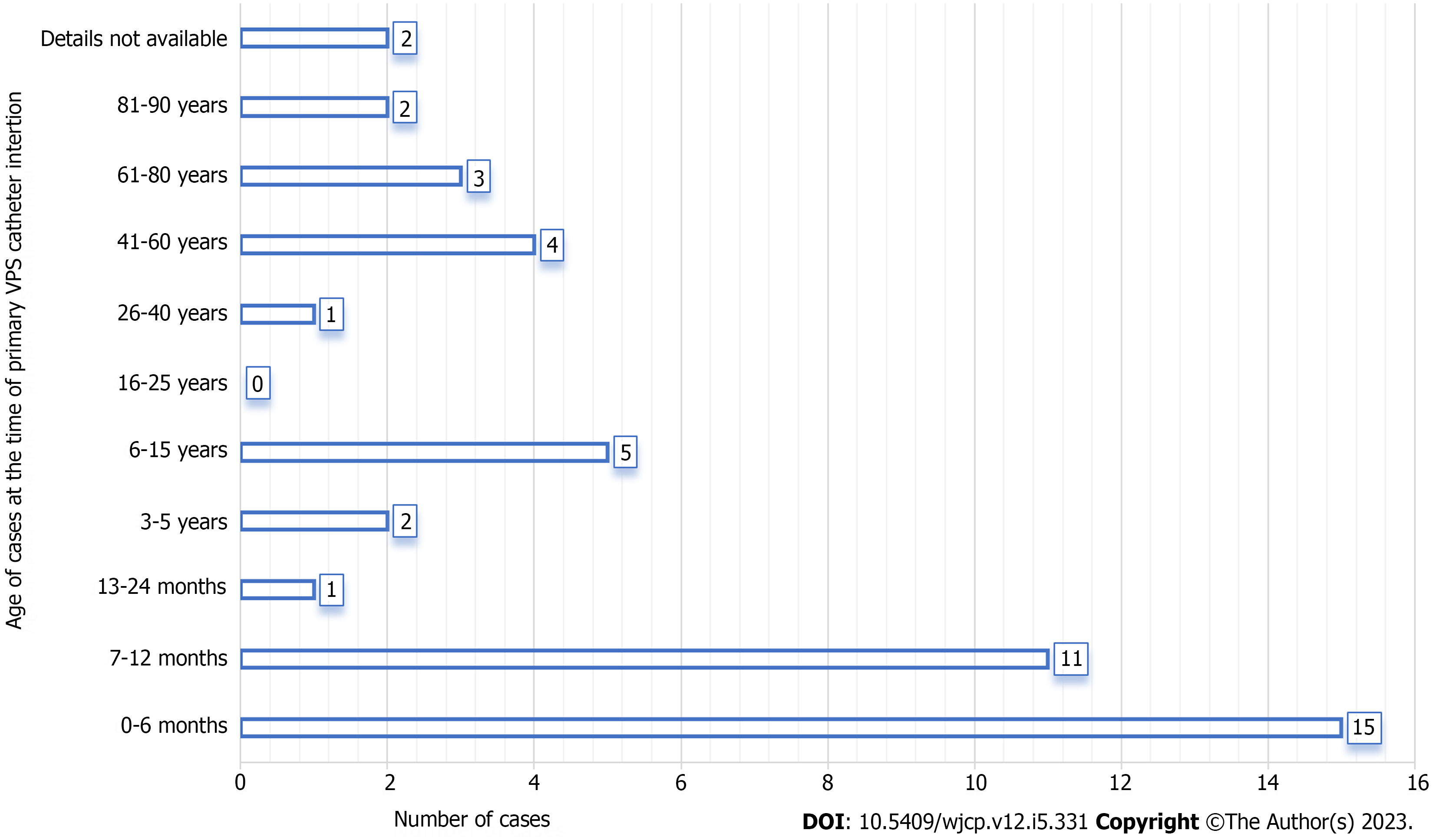
Figure 3 Age distribution (entire cases) at the time of primary ventriculoperitoneal shunt insertion (n = 46).
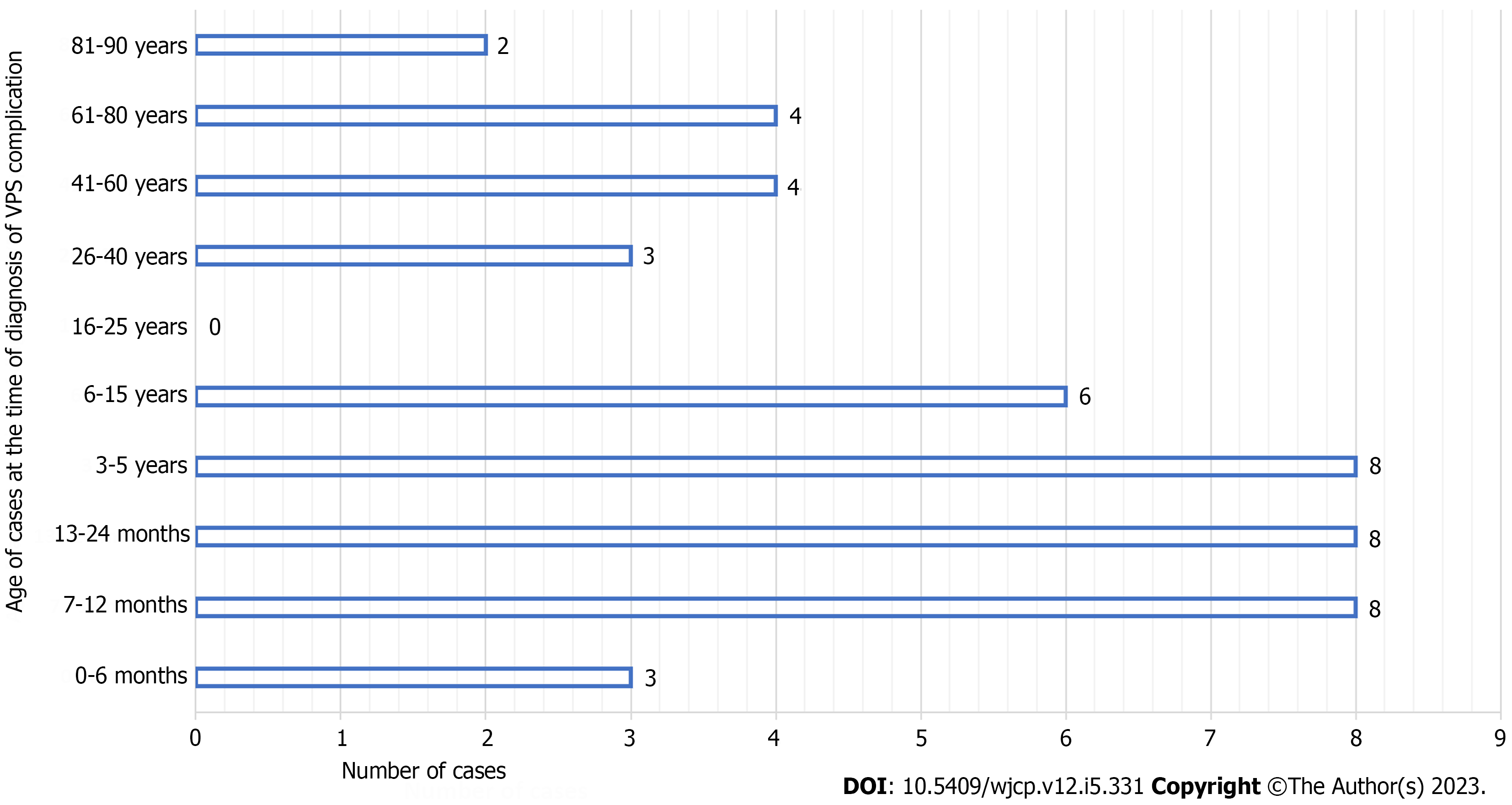
Figure 4 Age distribution (entire cases) at the time of diagnosis of migration of the distal ventriculoperitoneal shunt catheter into the stomach with or without trans-oral extrusion (n = 46).
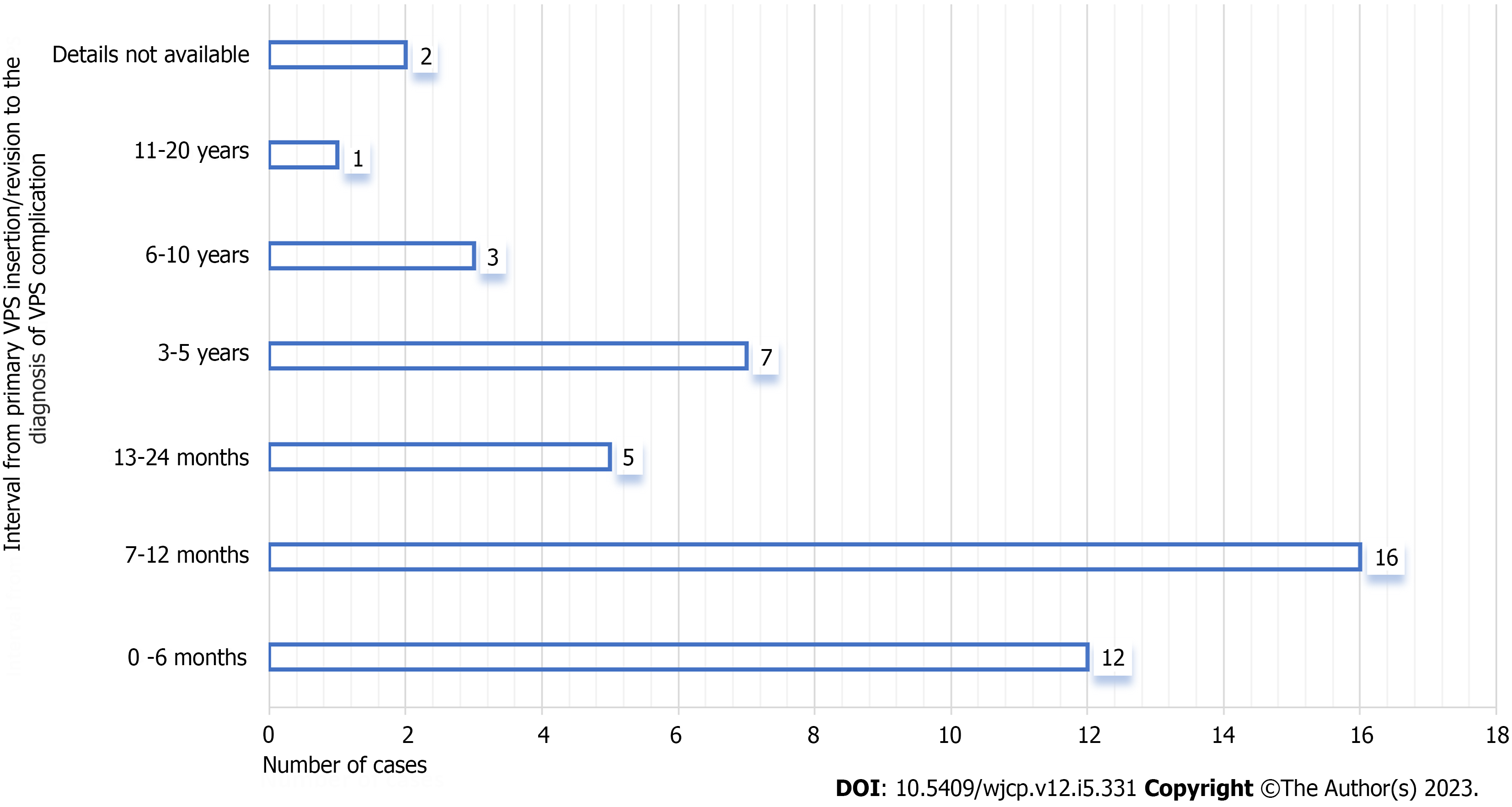
Figure 5 Interval (entire cases) from primary ventriculoperitoneal shunt catheter insertion/revision to the diagnosis of migration of the distal ventriculoperitoneal shunt catheter into the stomach with or without trans-oral extrusion (n = 46).
Figure 6 Clinical photograph of a 2 years-old-girl presented with trans-oral extrusion of the distal ventriculoperitoneal shunt catheter.
This child was operated upon/managed by the author and published[37].
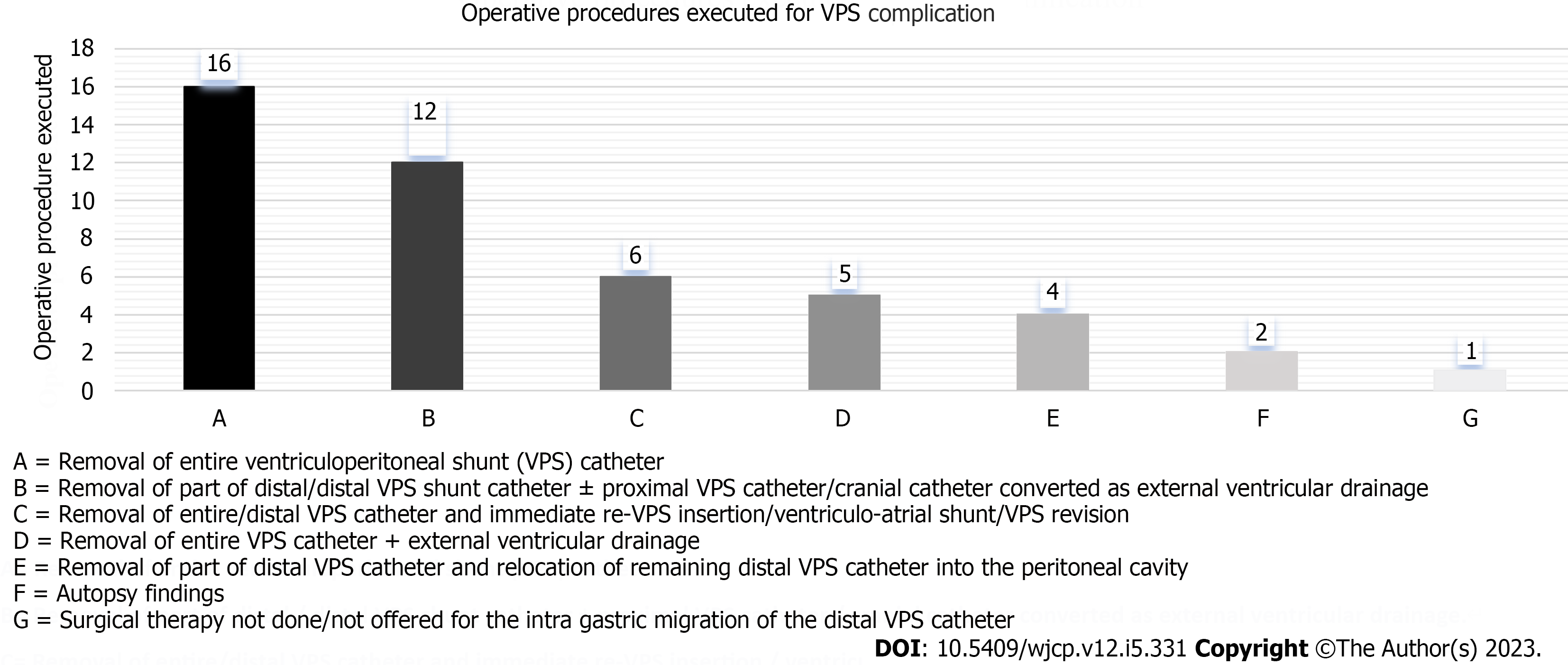
Figure 7 Operative procedures executed for the migration of distal ventriculoperitoneal shunt catheter into the stomach with or without trans-oral extrusion (n = 46).
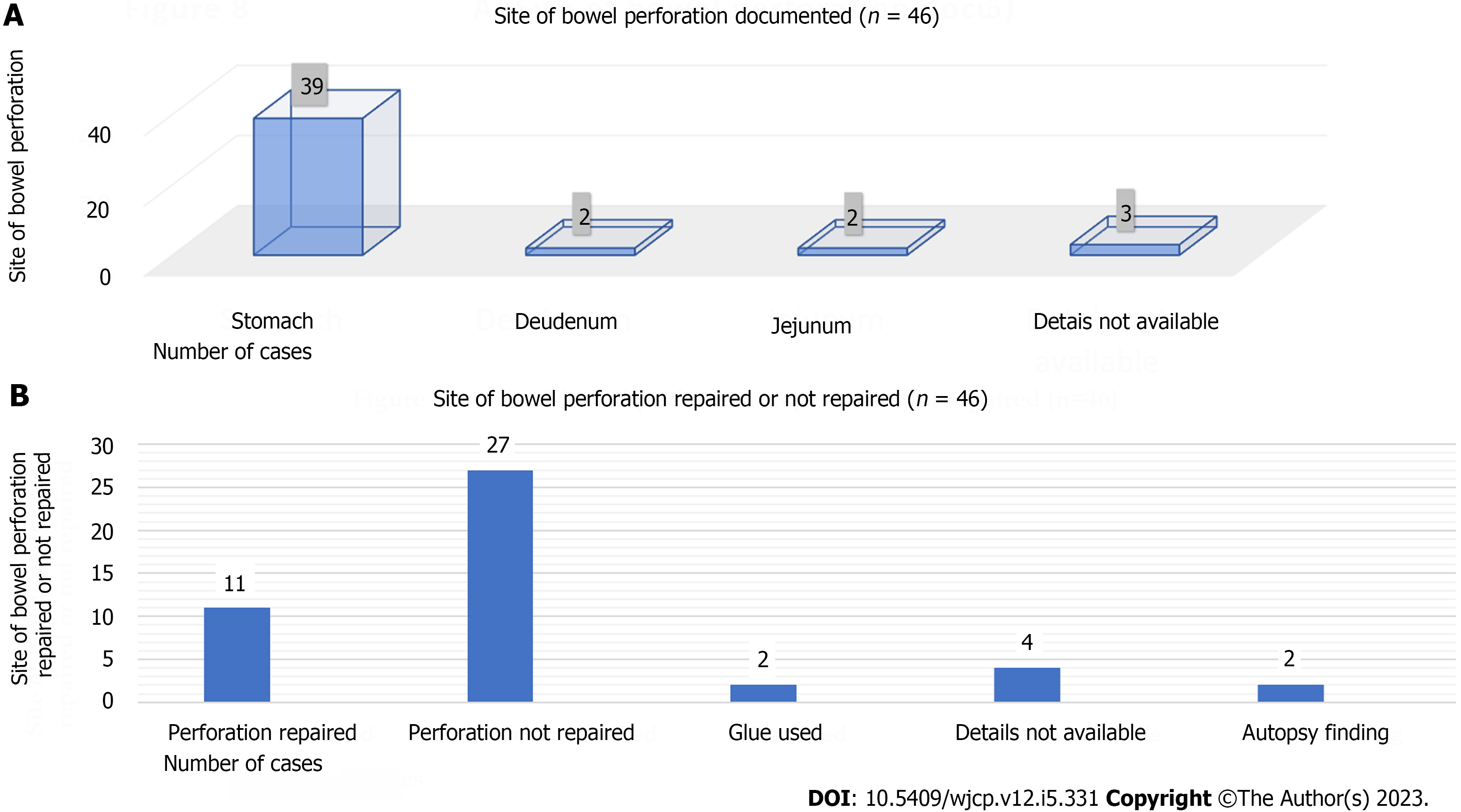
Figure 8 The site of bowel perforation caused by the distal ventriculoperitoneal shunt catheter.
A: Site of bowel perforation documented in the entire cases (n = 46); B: Site of bowel perforation repaired or not repaired (n = 46).
- Citation: Ghritlaharey RK. Migration of the distal ventriculoperitoneal shunt catheter into the stomach with or without trans-oral extrusion: A systematic literature review and meta-analysis. World J Clin Pediatr 2023; 12(5): 331-349
- URL: https://www.wjgnet.com/2219-2808/full/v12/i5/331.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v12.i5.331