Copyright
©The Author(s) 2022.
World J Clin Pediatr. May 9, 2022; 11(3): 221-238
Published online May 9, 2022. doi: 10.5409/wjcp.v11.i3.221
Published online May 9, 2022. doi: 10.5409/wjcp.v11.i3.221
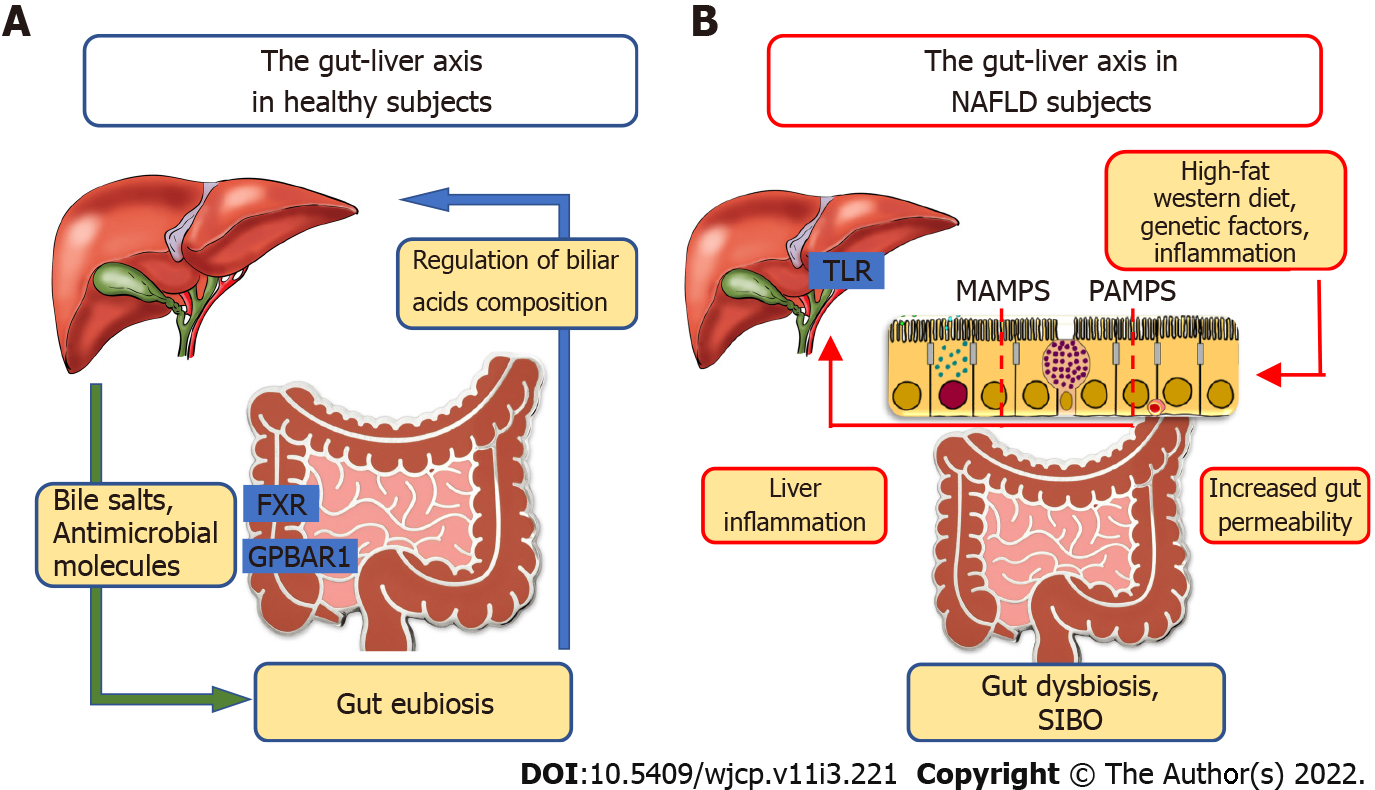
Figure 1 The role of the gut-liver axis in non-alcoholic fatty liver disease.
A: In healthy patients, the liver through the transport of bile salts and antimicrobial molecules to the intestinal lumen contributes to the maintenance of gut eubiosis. Conversely, the gut regulates bile acids (BAs) composition. BAs using farnesoid X receptor in the enterocytes and G protein-coupled bile acid receptor 1 are involved in the regulation of glucose and lipid metabolism, anti-inflammatory immune responses and host energy expenditure; B: In subjects with non-alcoholic fatty liver disease, altered gut microbial composition (dysbiosis), small intestinal bacterial overgrowth, and increased intestinal permeability (resulting from different factors including high-fat Western diet, genetic, inflammation) promote the influx of microbial-associated molecular patterns or pathogen-associated molecular patterns into the portal system reaching the liver. These molecular patterns are able to induce inflammatory responses mediated by the activation of pattern recognition receptors, like toll-like receptor, in Kupffer cells and hepatic stellate cells, leading to liver inflammation and fibrosis.
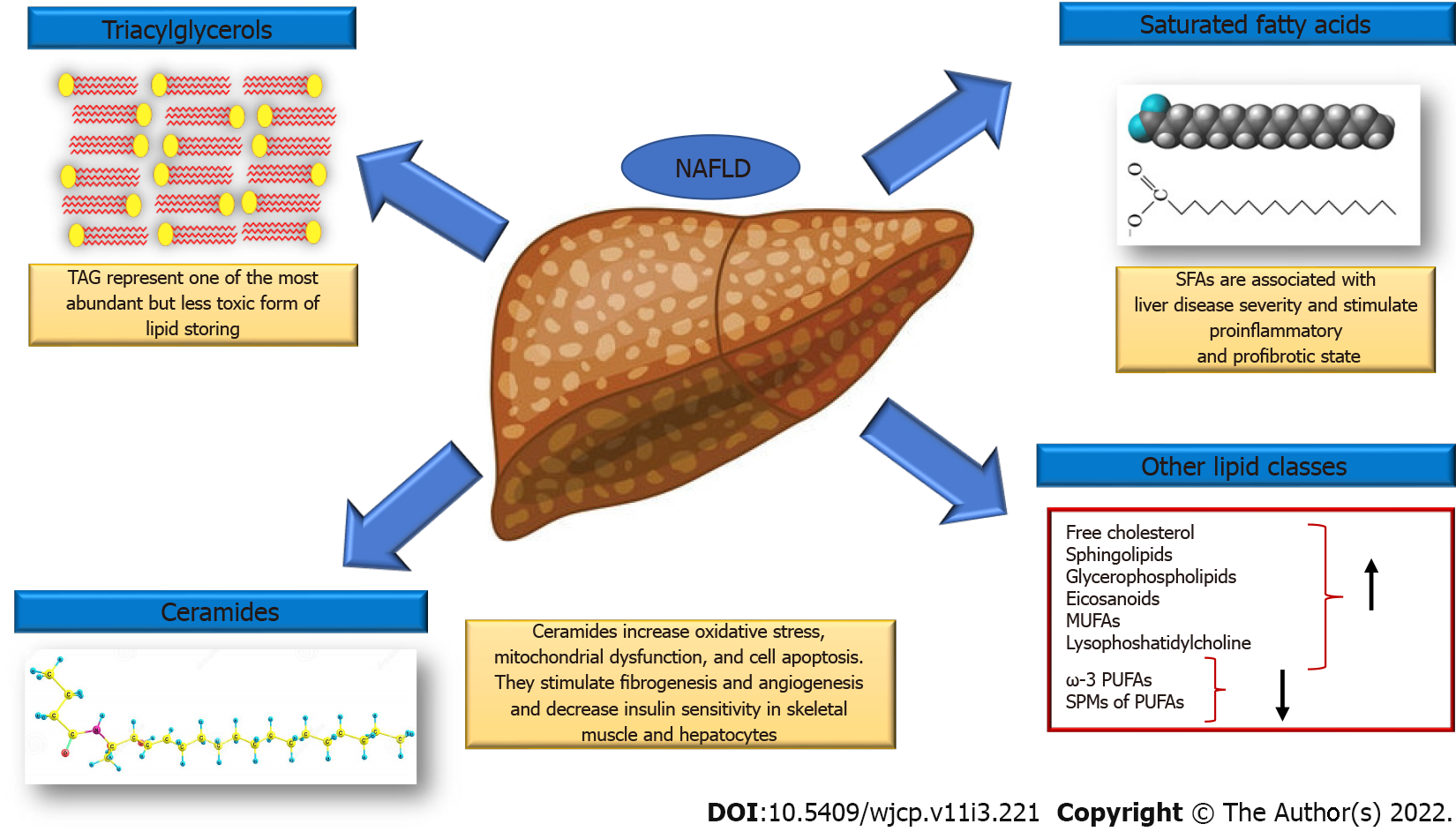
Figure 2 Main changes in hepatic lipid composition in non-alcoholic fatty liver disease.
In non-alcoholic fatty liver disease subjects, hepatic concentrations of triacylglycerols, saturated fatty acids, free cholesterol, sphingolipids, glycerophospholipids and eicosanoids are increased, whereas ω-3 polyunsaturated fatty acids (PUFAs) and specialized proresolving mediators of PUFAs are decreased. Monounsaturated fatty acids, lysophosphatidylcholine and ceramide are also increased in the liver of these subjects.
- Citation: Riccio S, Melone R, Vitulano C, Guida P, Maddaluno I, Guarino S, Marzuillo P, Miraglia del Giudice E, Di Sessa A. Advances in pediatric non-alcoholic fatty liver disease: From genetics to lipidomics. World J Clin Pediatr 2022; 11(3): 221-238
- URL: https://www.wjgnet.com/2219-2808/full/v11/i3/221.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v11.i3.221