Published online Aug 20, 2013. doi: 10.5321/wjs.v2.i3.56
Revised: February 17, 2013
Accepted: April 10, 2013
Published online: August 20, 2013
Processing time: 173 Days and 22.3 Hours
AIM: To investigate the success rate of mini-implants and its characteristics and risk factors by survival analyses.
METHODS: Three hundred and ninety-four mini-implants of the same type were placed by a single clinician. Age, gender, treatment duration, time of failure, side and jaw of implantation and the soft tissue at placement site were recorded. Odds ratio, survival curves, and Cox proportional hazard model were applied to evaluate the factors influencing the mini-implants’ success rate.
RESULTS: The cumulative success rate was 88.1%. The maxilla had a significantly higher success rate than that of the mandible (91.7% vs 83.7%, respectively, P = 0.019). Placement of mini-implants in the attached gingiva (AG) showed a higher success rate than that of the mucogingival junction (MGJ) and mucous membrane (MM) (AG, 94.3%; MGJ, 85.8%; MM, 79.4%; P < 0.001). Significant association was found between the jaw and the gingival tissue type (P < 0.001). There were no significant differences between maxilla and mandible when compared within each placement site.
CONCLUSION: The gingival tissue type had the most significant effect on the success rate of the mini-implant with higher success rate in the attached gingiva.
Core tip: Anchorage reinforcement is a critical factor for successful orthodontic treatment outcome. Mini-implants are applied to achieve various dental movements such as anterior retraction, molar protraction and distalization, intrusion, extrusion, and correction of midline and occlusal canting. The gingival tissue type had the most significant effect on the success rate of the mini-implant with higher success rate in the attached gingiva.
- Citation: Baik UB, Bayome M, Han KH, Park JH, Jung MH, Kook YA. Evaluation of factors affecting the success rate of orthodontic mini-implants by survival analysis. World J Stomatol 2013; 2(3): 56-61
- URL: https://www.wjgnet.com/2218-6263/full/v2/i3/56.htm
- DOI: https://dx.doi.org/10.5321/wjs.v2.i3.56
Anchorage reinforcement is a critical factor for successful orthodontic treatment outcome. Mini-implants are applied to achieve various dental movements such as anterior retraction, molar protraction and distalization, intrusion, extrusion, and correction of midline and occlusal canting[1-4].
The factors affecting the success rate of mini-implants have been investigated extensively but not all of them are agreed upon regarding their significance by the investigators[5-10]. Type of mini-implant was suggested as a contributor to the success rate[11,12]. Age and gender of patients, the jaw and side receiving the mini-implant, and the type of gingival tissues were not significantly associated with the success rate[8,11,13,14].
However, Lee et al[15] reported a significant effect of age, and Manni et al[12] demonstrated the gender as a significant factor. In addition, peri-implant soft tissue characteristics may be a contributing factor[16]. Moon et al[13] also reported significant differences between placement sites between different teeth. Also, vertical skeletal pattern was reported to influence the success rate[10].
Recently, three or more types of mini-implants were placed by more than one operator[10,11,14,16]. However, Lee et al[15] inserted a single type of mini-implants and reported that there are no significant differences in the success rate according to clinicians. In Park et al[17] the mini-implants were placed by one clinician, but the sample size was relatively small for both reports.
However, a well-controlled study with larger sample size of a single type of mini-implants placed by one experienced clinician has not been conducted. This can minimize the effect of the operator- and mini-implant-related factors on the evaluation of success rate.
Therefore, the purpose of this study was to investigate the success rate of mini-implants and its characteristics and risk factors using the same type of mini-implants placed by single clinician by survival analyses.
A hundred and sixty four patients (47 male, 117 female; mean age 24.0 ± 6.8 years) treated with fixed appliance from July, 2009 to March, 2010 in a private orthodontic clinic were included in this retrospective study. Those who had special medical history such as osteoporosis, thyroid problem, diabetes, and hypertension were excluded.
A total number of 394 mini-implants were placed for anchorage reinforcement by one right-handed experienced clinician using a single placement technique (30° to the surface of soft tissue and about 20 N•cm torque on the self drilling miniscrew) and were loaded 3 wk after placement with a similar amount of force. Only one type of mini-implants was used to exclude the effect of the screw material and design (6.0 mm in length and 1.5 mm in diameter, Biomaterials Korea, Seoul, Korea).
The records were examined to retrieve the following data: age, gender, date of mini-implant placement, date of failure (if occurred), date of removal at the end of treatment, location (upper, lower, right, left) and gingival tissue type at placement site [attached gingiva (AG), mucogingival junction (MGJ), mucous membrane (MM)]. The success of the mini-implant was defined as being functionally stable till the end of the treatment without signs of inflammation. Meanwhile, failure was recorded in case of removal of the mini-implant due to looseness.
SAS 9.2 (SAS Institute Inc. Cary, NC, United States) was used for the statistical analysis. The Fisher exact test significance and odds ratio statistics were calculated. A nonparametric life table method was used to easily visualize the hazard function over time. Association between significant variables was assessed by χ2 test. Kaplan-Meier survival curves were generated, and the Gehan generalized Wilcoxon test was used to identify the variables associated with implant failure. Prognostic variables associated with implant failure were identified with the Cox proportional hazard model which is a survival model that relate the time passed before an event happens to one or more covariates (in our study: age, gender, jaw, side, and gingival tissue) that might be associated with that quantity of time. The level of statistical significance was set at 5%.
There was no significant difference in the success rates between implantation sides, gender, and age. However, there were significant differences between upper and lower implantation (91.7% vs 83.7%, respectively, P = 0.019) and according to the gingival tissue type at the placement site (AG, 94.3%; MGJ, 85.8%; MM, 79.4%; P < 0.001) (Table 1).
| Variables | Success | Failure | Total | P-value | OR (95%CI) | |
| Gender | 0.231 | |||||
| Male | 96 (84.96) | 17 (15.04) | 113 | |||
| Female | 252 (89.36) | 30 (10.64) | 282 | 0.762 (0.354, 1.274) | ||
| Jaw | 0.019 | |||||
| Maxilla | 199 (91.71) | 18 (8.29) | 217 | |||
| Mandible | 149 (83.71) | 29 (16.29) | 178 | 2.152 (1.151, 4.021) | ||
| R/L side | 0.877 | |||||
| Left | 117 (88.50) | 23 (11.50) | 200 | |||
| Right | 171 (87.69) | 24 (12.31) | 195 | 1.080 (0.587, 1.986) | ||
| Age | 0.973 | |||||
| < 20 | 106 (87.60) | 15 (12.40) | 121 | |||
| 20-30 | 204 (88.31) | 27 (11.69) | 231 | 0.935 (0.477, 1.834) | ||
| > 30 | 38 (88.37) | 5 (11.63) | 43 | 0.930 (0.316, 2.732) | ||
| Gingival tissue | < 0.001 | |||||
| AG | 165 (94.29) | 10 (5.71) | 175 | 0.367 (0.163, 3.204) | ||
| MGJ | 109 (85.83) | 18 (14.17) | 127 | 2.724 (1.212, 6.124) | ||
| MM | 73 (79.35) | 19 (20.65) | 92 | 4.294 (1.903, 9.689) | 1.576 (0.775, 3.204) | |
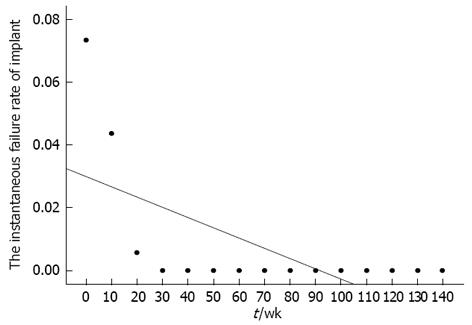
The hazard function of mini-implant survival time was regarded as the instantaneous failure rate[18]. As the latest failure event was at 27 wk, the function showed that the risk of failure was highest immediately after placement and then decreased to zero till the end of the treatment. The linear fit of the hazard function was R2 = 0.62 with a negative slope over time (Figure 1).
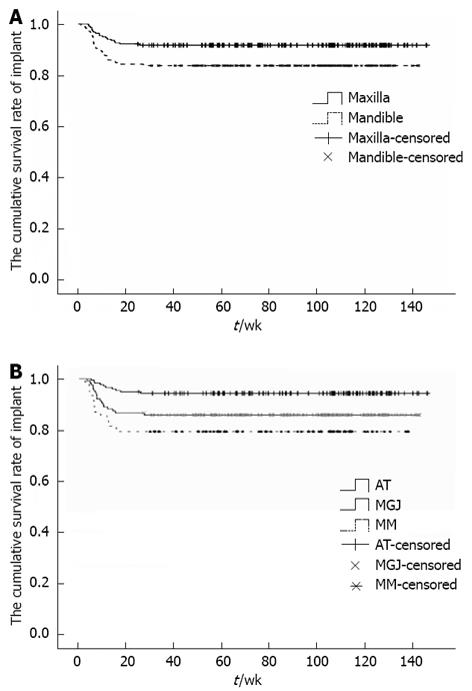
The Kaplan-Meier survival curve according to jaw and gingival tissue type (Figure 2) demonstrated high success rates for all subgroups. The Gehan generalized Wilcoxon test revealed that the implants placed in the maxilla had a higher success rate than those placed in the mandible (P = 0.014). Also, those placed in the attached gingiva had a significantly higher survival rate than other subgroups (P < 0.001).
χ2 test verified a significant association between the jaw and the gingival tissue type (P < 0.001) (Table 2). By Fisher’s exact test and odds ratio analysis, there were no significant differences between maxilla and mandible when compared according to gingival tissue type, independently (Table 3). The Cox proportional hazard model also showed that the gender and gingival tissue type are significant factors for mini-implant survival (Table 4). The estimated probability of failure was lower for females (P < 0.001) and the attached gingiva (P = 0.019).
| Mandible | Maxilla | P-value | |||
| Total | Failed | Total | Failed | ||
| Attached gingiva | 34 (19.1) | 4 (11.8) | 141 (65.3) | 6 (4.3) | |
| Mucogingival junction | 78 (43.8) | 11 (14.1) | 49 (22.7) | 7 (14.3) | < 0.001 |
| Mucous membrane | 66 (37.1) | 14 (21.2) | 26 (12.0) | 5 (19.2) | |
| Variables | Success | Failure | Total | P-value | OR (95%CI) |
| Attached gingiva | 0.105 | ||||
| Maxilla | 135 (95.74) | 6 (4.26) | 141 | ||
| Mandible | 30 (88.24) | 4 (11.76) | 34 | 3.000 (0.797, 11.293) | |
| Mucogingival junction | 1 | ||||
| Maxilla | 42 (85.71) | 7 (14.29) | 49 | ||
| Mandible | 67 (85.90) | 11 (14.10) | 78 | 0.985 (0.354, 2.740) | |
| Mucous membrane | 1 | ||||
| Maxilla | 21 (80.77) | 5 (19.23) | 26 | ||
| Mandible | 52 (78.79) | 14 (21.21) | 66 | 1.131 (0.362, 3.535) |
| Beta | SE | Wald | P-value | Exp (B) | 95%CI of Exp (B) | |
| Gender | 0.444 | 0.124 | 12.744 | < 0.001 | 1.559 | 1.222-1.989 |
| Jaw | 0.107 | 0.109 | 0.956 | 0.358 | 1.113 | 0.898-1.378 |
| R/L Side | -0.031 | 0.107 | 0.085 | 0.771 | 0.969 | 0.785-1.196 |
| Age | -0.027 | 0.084 | 0.101 | 0.751 | 0.974 | 0.826-1.148 |
| Gingival tissue | 0.162 | 0.069 | 5.512 | 0.012 | 1.176 | 1.027-1.347 |
With improvement of mini-implant materials, design and placement technique, recent studies have often reported mini-implant success rates higher than 90%[15,19]. On the other hand, since it is rare that a patient receives only one mini-implant during orthodontic treatment, the success rate faced by clinicians throughout treatment may be substantially lower due to presence of multiple mini-implants in each patient.
In our study, the success rate (88.1%) was slightly lower than that in Lee et al[15] (91.5%), higher than Manni et al[12] (81%) and similar to Cheng et al[16] (89%). Moreover, several studies evaluated numerous factors affecting the success rate of mini-implants[5,14,17,20]. However, most of them assessed many heterogenic variables using a small sample size that increase type II errors and decrease statistical power. In our study, to eliminate the factors related to the clinician and the mini-implant, only one clinician placed 394 mini-implant of the same type following the same insertion technique.
Recently, Manni et al[12] evaluated 12 different factors affecting the stability of mini-implants. Although the mini-implants in their study were placed by the same clinician, they were of 3 different types. Furthermore, the evaluation of too many variables may lead to generation of higher-order interactions resulting in a complicated result interpretation[21]. Our research was limited to only five host variables to avoid such a complication.
Lee et al[15] also evaluated five variables affecting the success rate of the mini-implants. However, the anatomical location and the soft tissue of the insertion site were not included in their study. They found patient’s age to be the only significant factor that affects the success rate of mini-implants. They recommended special caution when planning mini-implants for young patients. On the contrary, our results showed that the age was not a significant factor in determining the success of mini-implants.
Several reports demonstrated a significant effect for age on the success rate of mini-implants[15,20]. The higher risk of failure in younger patients could be attributed to their lower bone density[22,23]. However, in agreement with our results, other studies reported no significant differences among age-groups[13,14,17]. This inconsistency among results can be explained by the multifactorial nature of the mini-implant success rate. Moreover, it can be argued that Lee et al[15] and Chen et al[20] have overlooked the evaluation of the effect of gingival tissue type at the placement site.
In our study, the gingival tissue type at the placement site was the main factor affecting the success rate. In AG, the placement of mini-implant had a 2.7 times lower failure rate than in MGJ which in turn had a 1.6 times lower failure rate than in MM (Table 1). This was in accord with previous investigations[5,12,16]. Moreover, an animal study showed a significantly higher stability of mini-implants in keratinized gingiva. Within their limited sample size (22 mini-implants), all failed cases (n = 9) were placed in the non-keratinized gingiva[24]. The lower failure rate in the AG could be explained by the non-movable keratinized tissue that decreases the susceptibility to irritation and infection. On the other hand, some authors reported no significant differences in the success rate according to soft tissue[14,17,25].
Several studies reported higher success rate of mini-implant placement in the maxilla than that for those placed in the mandible[12,16,20]. On the other hand, some authors reported no significant differences between the upper and lower jaws in mini-implant success rate[11,13,14,25]. In our study, the jaw, initially, was a significant factor affecting the success rate. However, with further analysis, a significant association (P < 0.001) was found between the jaw and the gingival tissue type. The mini-implants placed in the mandible were mainly placed in mucous membrane or MGJ, while those placed in the maxilla were mainly in the attached gingiva. No significant differences in the success rates were found between the mini-implants placed in upper and lower jaws when compared within each gingival tissue type.
This was in agreement with Moon et al[13] who placed all the mini-implants in the attached gingiva and showed no significant difference in the success rate between maxilla and mandible. In addition, in our results, Cox proportional hazard model showed no significant effect of the jaw on the failure rate (P = 0.358). Therefore, the greater failure rate of mini-implants placed in the mandible can be explained by the lake of further analysis to examine any association between the jaw and other factors, such as inflammation, root proximity, and soft tissue mobility.
Similarly, gender was described as a significant factor in several studies. Moon et al[13] reported a higher success rate in male patients while in Antoszewska et al[5] study female subjects had a higher rate. Nevertheless, our results showed no significant difference in the rate according to gender. This was in accordance with several reports[14,17,20]. Interestingly, the Cox proportional hazard model in our study showed that gender was a significant factor. Therefore, future studies might be required to evaluate the influence of gender on the success rate with a larger sample size from both groups with uniform inclusion criteria that eliminate other confounding factors.
Time of loading has been evaluated in several reports but no consensus was reached. Trisi et al[26] demonstrated that immediate loading might undermine the stability of dental implants and increase the number of failures. On the contrary, other studies showed a positive influence for the immediate loading[12,27]. However, Miyawaki et al[11] found no correlation between the time of loading and success rate. In addition, Cheng et al[16] and Costa et al[28] achieved success rates of 89% and 87.5% with delayed and immediate loading, respectively. In our study, to minimize the effect of the loading time, all mini-implants were loaded three weeks after placement.
From our results, it is recommended that clinicians place mini-implant in the attached gingiva as long as possible to improve the success rate. However, further prospective controlled studies are required to evaluate the efficiency of different types of temporary anchorage devices used for various clinical situations.
In summary, with the single type of mini-implants used by the same clinician, survival analysis was performed to evaluate the success rate of mini-implant. The gender and gingival tissue type had significant effects on the success rate. Mini-implants placed in the attached gingiva had a higher success rate than that of those placed in the mucogingival junction and mucous membrane. However, no significant differences in the success rate were found according to age, gender, and implantation side and jaw. Therefore, it is recommended for clinician to consider the characteristics of gingival tissue prior to mini-implant insertion.
Anchorage reinforcement is a critical factor for successful orthodontic treatment outcome. Mini-implants are applied to achieve various dental movements such as anterior retraction, molar protraction and distalization, intrusion, extrusion, and correction of midline and occlusal canting.
With improvement of mini-implant materials, design and placement technique, recent studies have often reported mini-implant success rates higher than 90%. On the other hand, since it is rare that a patient receives only one mini-implant during orthodontic treatment, the success rate faced by clinicians throughout treatment may be substantially lower due to presence of multiple mini-implants in each patient.
With the single type of mini-implants used by the same clinician, survival analysis was performed to evaluate the success rate of mini-implant. The gender and gingival tissue type had significant effects on the success rate. Mini-implants placed in the attached gingiva had a higher success rate than that of those placed in the mucogingival junction and mucous membrane.
From their results, it is recommended that clinicians place mini-implant in the attached gingiva as long as possible to improve the success rate. However, further prospective controlled studies are required to evaluate the efficiency of different types of temporary anchorage devices used for various clinical situations.
This is a well-written and interesting article about mini-implants success rate. English grammar and language are good. The title reflects the major topic and contents of the study. The abstract clearly describes the research background, objectives, materials and methods, results and conclusions. The study design is appropriate, as well as the used statistical methods. The sample size and the statistical data are adequate for this clinical study.
P- Reviewer Arisan V, Boffano P S- Editor Gou SX L- Editor A E- Editor Lu YJ
| 1. | Kook YA, Bayome M, Kim SH, Lee DH, Kim YJ, Kim SG. Simplified abutment tooth extrusion using a mini-implant. World J Orthod. 2010;11:387-392. [PubMed] |
| 2. | Lim JK, Jeon HJ, Kim JH. Molar distalization with a miniscrew-anchored sliding jig. J Clin Orthod. 2011;45:368-377. [PubMed] |
| 3. | Modoni D, Modoni M, Romano G, Verdino A. Lower molar intrusion using skeletal anchorage. J Clin Orthod. 2011;45:22-24; quiz 39-40. [PubMed] |
| 4. | Upadhyay M, Yadav S, Nanda R. Vertical-dimension control during en-masse retraction with mini-implant anchorage. Am J Orthod Dentofacial Orthop. 2010;138:96-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Antoszewska J, Papadopoulos MA, Park HS, Ludwig B. Five-year experience with orthodontic miniscrew implants: a retrospective investigation of factors influencing success rates. Am J Orthod Dentofacial Orthop. 2009;136:158. e1-e10; discussion 158. e1-e10;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Kuroda S, Yamada K, Deguchi T, Hashimoto T, Kyung HM, Takano-Yamamoto T. Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2007;131:S68-S73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 251] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 7. | Justens E, De Bruyn H. Clinical outcome of mini-screws used as orthodontic anchorage. Clin Implant Dent Relat Res. 2008;10:174-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Motoyoshi M, Hirabayashi M, Uemura M, Shimizu N. Recommended placement torque when tightening an orthodontic mini-implant. Clin Oral Implants Res. 2006;17:109-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 261] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 9. | Wiechmann D, Meyer U, Büchter A. Success rate of mini- and micro-implants used for orthodontic anchorage: a prospective clinical study. Clin Oral Implants Res. 2007;18:263-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 113] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 10. | Moon CH, Park HK, Nam JS, Im JS, Baek SH. Relationship between vertical skeletal pattern and success rate of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010;138:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Miyawaki S, Koyama I, Inoue M, Mishima K, Sugahara T, Takano-Yamamoto T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2003;124:373-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Manni A, Cozzani M, Tamborrino F, De Rinaldis S, Menini A. Factors influencing the stability of miniscrews. A retrospective study on 300 miniscrews. Eur J Orthod. 2011;33:388-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Moon CH, Lee DG, Lee HS, Im JS, Baek SH. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod. 2008;78:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 140] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 14. | Lim HJ, Eun CS, Cho JH, Lee KH, Hwang HS. Factors associated with initial stability of miniscrews for orthodontic treatment. Am J Orthod Dentofacial Orthop. 2009;136:236-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | Lee SJ, Ahn SJ, Lee JW, Kim SH, Kim TW. Survival analysis of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010;137:194-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int J Oral Maxillofac Implants. 2004;19:100-106. [PubMed] |
| 17. | Park HS, Jeong SH, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130:18-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 368] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 18. | Lee ET, Wang JW. Statistical methods for survival data analysis. 3rd ed. Hoboken, NJ: Wiley 2003; . |
| 19. | Topouzelis N, Tsaousoglou P. Clinical factors correlated with the success rate of miniscrews in orthodontic treatment. Int J Oral Sci. 2012;4:38-44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Chen YJ, Chang HH, Huang CY, Hung HC, Lai EH, Yao CC. A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems. Clin Oral Implants Res. 2007;18:768-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 131] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 21. | Norman GR, Streiner DL. Biostatistics. The base essentials. St Louis: Mosby 1996; . |
| 22. | Kingsmill VJ, Boyde A. Variation in the apparent density of human mandibular bone with age and dental status. J Anat. 1998;192:233-244. [PubMed] |
| 23. | Han S, Bayome M, Lee J, Lee YJ, Song HH, Kook YA. Evaluation of palatal bone density in adults and adolescents for application of skeletal anchorage devices. Angle Orthod. 2012;82:625-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Ure DS, Oliver DR, Kim KB, Melo AC, Buschang PH. Stability changes of miniscrew implants over time. Angle Orthod. 2011;81:994-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 25. | Chen YJ, Chang HH, Lin HY, Lai EH, Hung HC, Yao CC. Stability of miniplates and miniscrews used for orthodontic anchorage: experience with 492 temporary anchorage devices. Clin Oral Implants Res. 2008;19:1188-1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 85] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 26. | Trisi P, Rebaudi A. Peri-implant bone reaction to immediate, early, and delayed orthodontic loading in humans. Int J Periodontics Restorative Dent. 2005;25:317-329. [PubMed] |
| 27. | Kuroda S, Sugawara Y, Deguchi T, Kyung HM, Takano-Yamamoto T. Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfort. Am J Orthod Dentofacial Orthop. 2007;131:9-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 292] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 28. | Costa A, Raffainl M, Melsen B. Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthodon Orthognath Surg. 1998;13:201-209. [PubMed] |