Revised: October 16, 2013
Accepted: March 3, 2014
Published online: March 28, 2014
Processing time: 258 Days and 0.9 Hours
Solitary pituitary metastasis is a rare phenomenon in human neoplasms. We report a case of lung cancer with the initial manifestation of endocrinopathy resulting from pituitary metastasis. The patient’s initial diagnosis was a poorly differentiated carcinoma, however, morbid anatomy revealed a definite diagnosis of large cell neuroendocrine carcinoma (LCNEC). Clinical physicians should be aware of potential initial manifestations such as endocrine abnormalities including panhypopituitarism and diabetes insipidus due to solitary pituitary metastasis. This case demonstrates that an endocrine abnormality such as panhypopituitarism could be an initial manifestation of LCNEC.
Core tip: Solitary pituitary metastasis is a rare phenomenon in human neoplasms. An endocrine abnormality such as panhypopituitarism could be an initial manifestation of large cell neuroendocrine carcinoma.
- Citation: Watanabe T, Kaira K, Mizuide M, Sunaga N, Shibusawa N, Hisada T, Satoh T, Mori M, Yamada M. Solitary pituitary metastasis resulting from pulmonary large cell neuroendocrine carcinoma. World J Respirol 2014; 4(1): 8-10
- URL: https://www.wjgnet.com/2218-6255/full/v4/i1/8.htm
- DOI: https://dx.doi.org/10.5320/wjr.v4.i1.8
Pulmonary neuroendocrine tumors consist of typical carcinoid, atypical carcinoid, large cell neuroendocrine carcinoma (LCNEC) and small-cell lung carcinoma (SCLC). LCNEC is an uncommon malignancy with aggressive features and a dismal prognosis. Although brain metastasis is often observed in patients with LCNEC, to our knowledge, there is no description of solitary pituitary metastasis due to LCNEC. Here, we describe a case of LCNEC with the initial manifestation of endocrinopathy secondary to pituitary metastasis.
A 74-year-old man with a smoking history presented with anorexia, vomiting, fever and thirst. Physical examination revealed dry mouth, decreased skin turgor and hypotonia with a blood pressure of 80/50 mmHg. Laboratory investigations revealed thyroid stimulatory hormone of 0.05 U/mL [normal range (NR): 0.5-5.5 U/mL], luteal hormone < 0.07 IU/mL, follicle stimulating hormone of 0.6 mIU/mL, testosterone of 2.51 ng/mL (NR: 1.31-8.71 ng/mL), growth hormone of 1.00 ng/mL, insulin-like growth factor 1 of 11.0 ng/mL (NR: 121-436 ng/mL), adrenocorticotropic hormone of 2.4 pg/mL (NR: 1.0-5.2 pg/mL), and urinary free cortisol < 0.5 μg/d (NR: 11.2-80.3 μg/d), suggesting panhypopituitarism including secondary adrenal failure. The patient had symptoms of thirst, polyposia and increased urination (over 3 L/d). Laboratory investigations revealed low urine specific gravity of 1.004, plasma osmolarity of 319 mOSM, low urine osmolarity of 194 mOSM (< 300 mOSM/kg), and the ratio was 0.686 (< 1). The administration of 1-desamino-8-D-arginine vasopressin resulted in urine volume reduction and urine condensation. A definite diagnosis of diabetes insipidus was made following these laboratory investigations and physical examination.
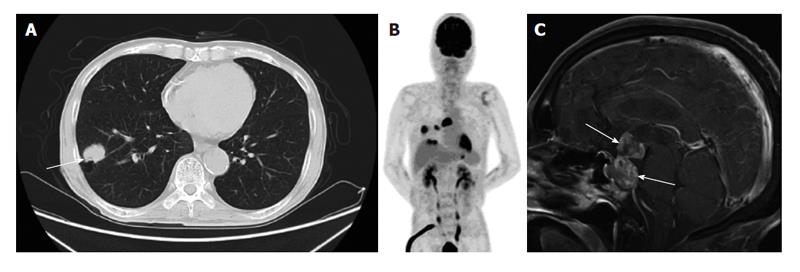
Computed tomography of the chest showed a mass on the right upper lobe and swelling of mediastinal lymph nodes (Figure 1A). Percutaneous needle biopsy diagnosed a poorly differentiated adenocarcinoma. Brain magnetic resonance imaging showed a dumbbell-shaped gadolinium-enhanced tumor in the pituitary (Figure 1B). 2-18F-fluoro-2-deoxy-D-glucose (18F-FDG) positron emission tomography (PET) revealed an increased accumulation of 18F-FDG in the lung, pituitary, liver and mediastinal lymph nodes (Figure 1C). A definite diagnosis of primary lung cancer stage IV (cT1bN2M1b) was made. However, the patient had pan hypopituitary symptoms with a performance status of 4. Therefore, palliative radiation therapy was administered for the solitary pituitary mass in order to improve the patient’s quality of life. Following radiotherapy of 50 Gy/25 fr, the patient experienced an improvement in appetite and nausea. On the 58th hospital day, the patient was discharged from our institution due to improving quality of life. However, he died as a result of severe pneumonia and disseminated intravascular clotting due to progression of the primary disease 10 d after discharge. Evaluation of morbid anatomy was performed following permission from the bereaved family. The immunohistochemical findings of primary lung tumor and solitary pituitary metastasis revealed marked positive staining of chromogranin A, CD56 (NCAM) and synaptophysin. The final diagnosis was solitary pituitary metastasis resulting from LCNEC.
Postmortem studies have shown that pituitary gland metastasis is observed in 0.14% to 28.1% of all brain metastases and patients with breast and lung cancer account for approximately two thirds of these metastases[1]. Although solitary pituitary metastasis is an extremely rare condition, the histology of adenocarcinoma or small-cell carcinoma is often seen in patients with lung cancer[2]. In our patient, the diagnosis was poorly differentiated adenocarcinoma by percutaneous needle biopsy, however, a definite diagnosis of LCNEC was subsequently made. The diagnosis of LCNEC is difficult to establish based on small biopsies or cytology, because there is a limit to evaluating a neuroendocrine pattern morphologically[3]. Recently, Shimada et al[4] proposed the term “high-grade neuroendocrine carcinoma-probable LCNEC (HG-pLCNEC)” from biopsy findings and aimed to elucidate the clinical features compared with SCLC, suggesting that therapeutic efficacy in HG-pLCNEC is similar to that of SCLC. The diagnostic criteria of LCNEC are problematic in biopsy specimens, and our patient was initially diagnosed with poorly differentiated adenocarcinoma.
The patient developed the primary symptom of panhypopituitarism due to pituitary metastasis. Radiologically, it is important to differentiate between pituitary metastasis derived from primary lung cancer and pituitary carcinoma. As primary pituitary carcinoma has an occurrence of 0.1%[5,6], its definite diagnosis requires pathological evidence of a pituitary mass. In our case, the pituitary mass was not treated surgically due to the patient’s poor performance status.
A retrospective study demonstrated that 10 of 1639 lung cancer patients (0.61%) had the initial manifestation of central diabetes insipidus[7]. Panhypopituitarism due to solitary pituitary metastasis is relatively rare, therefore, may be overlooked as an initial symptom of lung cancer. Although multiple brain metastases due to LCNEC are a frequent occurrence, a single pituitary metastasis may also occur. These symptoms can be masked by systemic complications of malignancy, including nonspecific symptoms (malaise, weakness, vomiting, weight loss) and central nervous system involvement. There may be a number of patients with primary cancer whose pituitary insufficiency is not appropriately diagnosed. The possibility that lung cancer has metastasized to the pituitary gland should be considered, and the administration of appropriate endocrine replacement in a timely manner can improve symptoms due to these lesions.
Clinical physicians should be aware of potential initial manifestations such as endocrine abnormalities including panhypopituitarism and diabetes insipidus due to solitary pituitary metastasis.
A 74-year-old man with a smoking history presented with anorexia, vomiting, fever and thirst.
The diagnostic criteria of large cell neuroendocrine carcinoma (LCNEC) are problematic in biopsy specimens, and the present case was initially diagnosed with poorly differentiated adenocarcinoma.
Panhypopituitarism due to solitary pituitary metastasis is relatively rare, therefore may be overlooked as an initial symptom of lung cancer.
Clinical physicians should be aware of potential initial manifestations such as endocrine abnormalities including panhypopituitarism and diabetes insipidus due to solitary pituitary metastasis.
This case demonstrates that an endocrine abnormality such as panhypopituitarism could be an initial manifestation of LCNEC.
The pituitary metastasis of LCNEC is a very rare condition and the message derived from the case is clinically useful.
P- Reviewer: Tanriverdi F S- Editor: Gou SX L- Editor: Webster JR E- Editor: Liu SQ
| 1. | Komninos J, Vlassopoulou V, Protopapa D, Korfias S, Kontogeorgos G, Sakas DE, Thalassinos NC. Tumors metastatic to the pituitary gland: case report and literature review. J Clin Endocrinol Metab. 2004;89:574-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 266] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 2. | Jung JW, Noh GY, Lee TH, Lee YY, Yi KH, Kim CH, Lee JC. Polyuria and polydipsia in a patient with non-small-cell lung cancer. Clin Lung Cancer. 2007;8:565-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Travis WD. Advances in neuroendocrine lung tumors. Ann Oncol. 2010;21 Suppl 7:vii65-vii71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 224] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 4. | Shimada Y, Niho S, Ishii G, Hishida T, Yoshida J, Nishimura M, Yoh K, Goto K, Ohmatsu H, Ohe Y. Clinical features of unresectable high-grade lung neuroendocrine carcinoma diagnosed using biopsy specimens. Lung Cancer. 2012;75:368-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Ishiguro T, Kasahara K, Kimura H. Diabetes Insipidus Induced by Metastasis of Lung denocarcinoma to Pituitary Gland. Jpn J Lung Canc. 2007;47:125-130. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Heaney AP. Clinical review: Pituitary carcinoma: difficult diagnosis and treatment. J Clin Endocrinol Metab. 2011;96:3649-3660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 135] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 7. | Mao JF, Zhang JL, Nie M, Lu SH, Wu XY. Diabetes insipidus as the first symptom caused by lung cancer metastasis to the pituitary glands: clinical presentations, diagnosis, and management. J Postgrad Med. 2011;57:302-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |