Published online May 12, 2015. doi: 10.5318/wjo.v5.i2.80
Peer-review started: March 2, 2014
First decision: April 4, 2014
Revised: February 15, 2015
Accepted: March 4, 2015
Article in press: March 5, 2015
Published online: May 12, 2015
Processing time: 449 Days and 6.6 Hours
AIM: To review results of traumatic cataracts in children.
METHODS: Only those pediatric patients who fitted in the definite inclusion criteria were considered for study enrollment. They were further examined for any kind of co-morbidities because of trauma, operated upon for traumatic cataracts with intraocular lens implantation. Amblyopia if present was treated. All were re-examined at the culmination of six-week postoperative period. According to the Birmingham Eye Trauma Terminology System the traumatic cataract cases were divided into group 1 (open globe) and group 2 (closed globe), and then determinants of visual acuity were compared.
RESULTS: There were 544 eyes in group 1 and 127 eyes in group 2 in our study of 671 eyes with pediatric traumatic cataracts. Visual acuity at the end of 6 wk after surgery in the operated eye was > 6/60 in 450 (82.7%) and ≥ 6/12 in 215 (39.4%) eyes in the open globe group and > 20/200 in 127 (81.8%) and ≥ 6/12 in 36 (28.4%) eyes in the closed globe group (P = 0.143), and the difference between the groups was not significant in children. Overall, 402 (39.4%) eyes gained ≥ 6/60 and > 5/12 in 238 (35.4%) cases. Surgical treatment caused a significant difference in visual outcome (P = 0.000). When we compared achieved visual outcome with ocular trauma score predicted vision, no significant difference was found.
CONCLUSION: Traumatic cataracts in children may have better outcome and ocular trauma score is a useful predictive method for the ocular trauma in children.
Core tip: We have studied visual outcome in children in one of the largest published database for cases of traumatic cataracts in children. We have also studied validity of ocular trauma score in case of ocular injuries in pediatric age group.
- Citation: Shah MA, Shah SM, Chaudhry AH, Pannu S. Traumatic cataracts in children: Visual outcome. World J Ophthalmol 2015; 5(2): 80-85
- URL: https://www.wjgnet.com/2218-6239/full/v5/i2/80.htm
- DOI: https://dx.doi.org/10.5318/wjo.v5.i2.80
Very few studies have attended to the challenge of ocular injuries in rural regions, though trauma itself is one of the leading reasons behind monocular blindness in the developed countries[1,2]. The probable causes of ocular injury vary in rural and urban regions and need to be looked into. Aiming available means in the right direction to strategize the prevention of such injuries requires knowledge regarding the etiology of injury[3,4]. Pediatric ocular trauma essentially is prognostically bad and hence is a burden to the society. This can be taken care of to some extent with the help of aforementioned knowledge of etiology of injury.
Trauma to the eye is capable of giving rise to cataracts. There is no difference in the methods which are employed to assess the visual outcome.
The standardization of ocular injury documentation was greatly facilitated following the introduction of Birmingham Eye Trauma Terminology System (BETTS)[5] in regular practice. Hence, the reviewing of visual outcomes will prove to be revealing. In this study, visual outcomes in eyes operated for cataracts resulting from trauma were analyzed at our centre. Also, post-treatment predictors of visual outcomes were studied. Our hospital is situated in an area which is predominantly inhabited by tribal populace (around 4.2 million), where certified eye specialists cater to them with a quality service at a very reasonable and low cost.
We started this study following attaining authorization from hospital management and research board. Guardians’ (of the patients) written permission was also procured. In 2002 this research was proposed as a retrospective review. All children (≤ 18 years old) who developed traumatic cataracts in any of the eyes detected and treated between 2003 and 2009 were registered in this research. Only those who were ready to join and those without any other severe physical collateral injury were taken in. All details related to the cases were obtained from our records and brought together by employing a pre-checked online form. A full history consisting of particulars of trauma, details of its management and type of surgery done to treat it was accumulated. BETTS format (available online) was employed first and subsequent visits reports were collected. In a similar way surgery details were gathered.
All patients with traumatic cataracts were split into two parts, namely, closed globe and open globe injuries. Open globe injuries were again sub-grouped into rupture and laceration injuries. This later type was again subdivided into trauma resulting in intraocular foreign body, perforating and penetrating traumas. Contusion and lamellar laceration were the sub-categories of closed ball injuries.
The usual demographic aspects were recorded, but the main attention was given to the facts related to the time and type of injury, the objects responsible for injury and movement as well as activity at the time of trauma. Also verified were the treatment and details of earlier examinations.
By means of accepted protocol, thereafter, all the patients underwent examination, in which we tested visual acuity according to age as per guidelines laid down by American Academy of Ophthalmology (AAO). Slit lamp examination was carried out for anterior segment.
Depending on the extent of lenticular opacity, all the cataracts were categorized as membranous cataract in those cases where organized lens matter and capsule formed a visually inseparable membrane, rosette cataract where rosette pattern was noted, and white soft cataract when the anterior chamber displayed loose cortical matter along with ruptured capsule.
To assess posterior segment B-scan examination was carried out where media did not permit, otherwise indirect ophthalmoscopy with +20D lens was done[6].
The operative procedure was chosen depending on the state of lens and other ocular tissues. Cataracts with large, harder nuclei were necessarily dealt with by phacoemulsification technique. Softer ones were aspirated either co-axially or bimanually. Membranous cataracts were operated through pars-plana or anterior route with membranectomy and anterior vitrectomy.
Corneal injuries were prioritized and hence repaired first, whereas cataract was managed later on. However, recurrent inflammation was a rule rather than exception in patients who were operated upon previously for injury, which made the anterior vitreous body hazy and required anterior or pars plana vitrectomy and/or capsulectomy (in older patients). In children under two years of age pars plana lensectomy along with anterior vitrectomy was a regulation procedure. Here primary intraocular lens implantation was not considered.
As far as medical management is concerned, cycloplegics and steroids in topical form were given in all cases of which did not have infection. The severity of inflammation in anterior and posterior segments in the surgically treated eye decided the extent of medical treatment. All operated cases were reviewed on the 1st, 3rd, 7th and 14th day. At the end of six weeks of surgery, refraction was ascertained. The routine follow-up review was planned after 3 d, then every week for six weeks, every month for three months and quarterly for 1 year.
Visual acuity of all patients was checked according to AAO directives on all review visits. Slit lamp examination for anterior and indirect ophthalmoscopes for the posterior segment was essentially done at follow-ups. Visual acuity more than 20/60 at the time of refraction examination was considered as having an acceptable grade of vision.
All these follow-up examination data were fed online by means of a format developed by the International Society of Ocular Trauma and sent to a Microsoft Excel Spreadsheet. Time and again thorough appraisal of the data was done on a regular basis to make sure its completion. SPSS17 was utilized to evaluate the data, and a biostatician certified data analysis report.
In this study we had 671 patients, all of whom had traumatic cataracts. 544 (81.07%) eyes had open globe injuries, and 127 (18.9%) were of closed globe injury type. 70.9% (496) were males, and 29.2% (196) were females. The average age was 10.53 ± 4.2 years (range, 0-17 years) (Table 1).
| Sex | Total | ||
| F | M | ||
| 0 to 2 | 6 | 7 | 13 |
| 3 to 5 | 27 | 52 | 79 |
| 6 to 10 | 74 | 179 | 253 |
| 11 to 18 | 88 | 238 | 326 |
| Total | 195 | 476 | 671 |
Analysis (by means of statistical tests and cross tabulation) of many factors related to demographic details such as socio-economic condition (79% belonged to lower stratum), locality (95% were from rural backdrop) and patient entry (P = 0.000) revealed that none of them had any significant bearing on visual acuity after 6 wk (Table 2, Table 3, Table 4 and Table 5).
| Vision | Entry | Total | |
| Self | ORD | ||
| < 1/60 | 19 | 0 | 19 |
| 1/60 to 3/60 | 68 | 30 | 98 |
| 6/60 to 6/36 | 74 | 53 | 127 |
| 6/24 to 6/18 | 125 | 55 | 180 |
| > 6/12 to 6/9 | 178 | 53 | 231 |
| Uncooperative | 11 | 5 | 16 |
| Total | 475 | 196 | 671 |
| Object | Number (n) | Percentage (%) |
| Ball | 9 | 1.4 |
| Cattle horn | 11 | 1.7 |
| Cattle tail | 2 | 0.3 |
| Finger | 5 | 0.8 |
| Fire | 19 | 2.8 |
| Glass | 7 | 1.1 |
| Thorn | 23 | 3.4 |
| Others | 59 | 8.8 |
| Sharp object | 59 | 8.8 |
| Stone | 72 | 10.7 |
| Unknown | 60 | 8.8 |
| Stick | 345 | 51.4 |
| Total | 671 | 100.0 |
| Object | Number (n) | Percentage (%) |
| Fall | 11 | 1.7 |
| Making a fire | 19 | 2.8 |
| Housework | 110 | 16.4 |
| Employment | 38 | 5.6 |
| Others | 85 | 12.7 |
| Walking | 8 | 1.1 |
| Playing | 370 | 55.1 |
| Travelling | 22 | 3.4 |
| Unknown | 8 | 1.1 |
| Total | 671 | 100.0 |
| Postoperative vision | Age category | Total | |||
| 0 to 2 | 3 to 5 | 6 to 10 | 11 to 18 | ||
| < 1/60 | 2 | 32 | 76 | 83 | 193 |
| 1/60 to 3/60 | 1 | 3 | 37 | 35 | 76 |
| 6/60 to 6/36 | 7 | 25 | 29 | 19 | 80 |
| 6/24 to 6/18 | 1 | 8 | 35 | 40 | 84 |
| 6/12 to 6/9 | 1 | 8 | 53 | 89 | 151 |
| 6/6 to 6/5 | 1 | 2 | 21 | 60 | 84 |
| Uncooperative | 0 | 1 | 2 | 0 | 3 |
| Total | 13 | 79 | 253 | 326 | 671 |
Causative agent of injury and person’s physical movements as well as type of activity were also not noteworthy reasons as far as six-week post-operative visual acuity was concerned. The most frequent agent causing trauma was stick.
Evaluation of visual acuity before and after surgery revealed that management did essentially increase the visual acuity (Table 6).
| Postoperativevision | Preoperative vision | Total | |||||
| <1/60 | 1/60 to 3/60 | 6/60 to 6/36 | 6/24 to 6/18 | 6/12 to 6/9 | Uncooperative | ||
| < 1/60 | 182 | 4 | 6 | 0 | 1 | 0 | 193 |
| 1/60 to 3/60 | 70 | 5 | 1 | 0 | 0 | 0 | 76 |
| 6/60 to 6/36 | 55 | 8 | 15 | 1 | 0 | 1 | 80 |
| 6/24 to 6/18 | 71 | 10 | 2 | 1 | 0 | 0 | 84 |
| 6/12 to 6/9 | 125 | 17 | 7 | 1 | 1 | 0 | 151 |
| 6/6 to 6/5 | 64 | 10 | 6 | 4 | 0 | 0 | 84 |
| Uncooperative | 2 | 0 | 0 | 0 | 0 | 1 | 3 |
| Total | 569 | 54 | 37 | 7 | 2 | 2 | 671 |
Co-axial or bi-manual aspiration of the ruptured cataract with cortical matter in the anterior chamber (in 48.6% cases among the open globe group) showed better visual acuity (Table 7).
| Postoperativevision | Morphology | Total | ||||
| Membranous | Rosette | Soft fluffy | Subluxated | Total | ||
| < 1/60 | 45 | 1 | 71 | 2 | 74 | 193 |
| 1/60 to 3/60 | 15 | 2 | 29 | 0 | 30 | 76 |
| 6/60 to 6/36 | 15 | 4 | 29 | 0 | 32 | 80 |
| 6/24 to 6/18 | 20 | 2 | 39 | 0 | 23 | 84 |
| 6/12 to 6/9 | 16 | 6 | 90 | 0 | 39 | 151 |
| 6/6 to 6/5 | 3 | 7 | 53 | 2 | 19 | 84 |
| Uncooperative | 0 | 0 | 3 | 0 | 0 | 3 |
| Total | 114 | 22 | 314 | 4 | 217 | 671 |
In eyes which were greatly inflamed, we routinely did primary posterior capsulotomy with anterior vitrectomy. This also did not influence the six-week postoperative visual acuity to any extent.
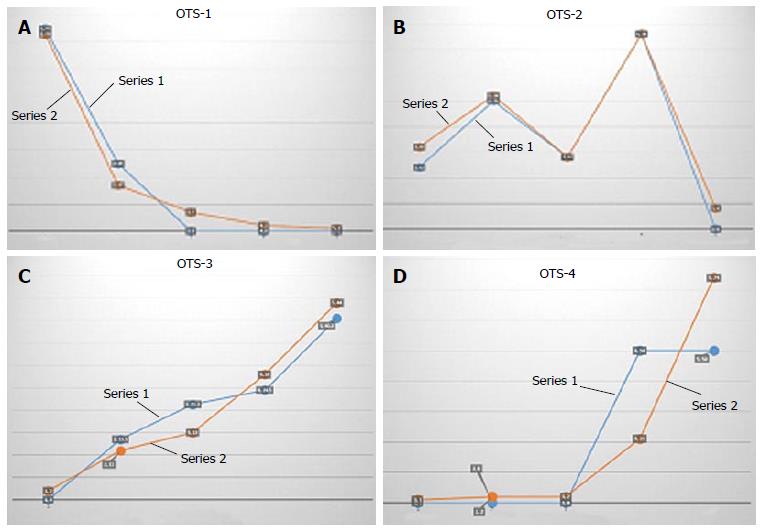
The achieved visual acuity after 6 wk of surgery was > 6/60 in 450 (82.7%) and ≥ 6/12 in 215 (39.4%) eyes in the open globe group and > 20/200 in 127 (81.8%) and ≥ 6/1236 (28.4%) eyes in the closed globe group (P = 0.143), and the difference between the groups was not significant in children. Overall, 402 (39.4%) eyes gained ≥ 6/60 and > 5/12 in 238 (35.4%) cases. Surgical treatment caused a significant difference in visual outcome (P = 0.000). When we compared achieved visual outcome with ocular trauma score predicted vision, we did not find a significant difference (Table 8, Table 9, and Table 10, Figure 1).
| Vision | Category | Total | |
| Closed | Open | ||
| 1/60 | 6 | 12 | 18 |
| 1/60 to 3/60 | 19 | 80 | 99 |
| 6/60 to 6/36 | 29 | 97 | 126 |
| 6/24 to 6/18 | 39 | 138 | 177 |
| > 6/12 | 30 | 206 | 236 |
| UC | 6 | 9 | 15 |
| Total | 127 | 544 | 671 |
| Final visual outcome | Ocular trauma score | Total | ||||
| 1 | 2 | 3 | 4 | 5 | ||
| UC | 2 | 2 | 9 | 0 | 2 | 15 |
| No PL | 6 | 13 | 0 | 0 | 0 | 19 |
| HM, PL | 2 | 27 | 72 | 0 | 0 | 101 |
| 1/200 to 19/200 | 0 | 15 | 112 | 0 | 0 | 127 |
| 20/200 to 20/50 | 0 | 40 | 134 | 4 | 0 | 178 |
| ≥ 0/40 | 0 | 9 | 218 | 4 | 0 | 233 |
| Total | 10 | 106 | 545 | 8 | 0 | 671 |
| Visioncategory | OTS-1 | OTS-2 | OTS-3 | OTS-4 | ||||
| Achieved final visual acuity | OTS Predicted final visual acuity | Achieved final visual acuity | OTS Predicted final visual acuity | Achieved final visual acuity | OTS Predicted final visual acuity | Achieved final visual acuity | OTS Predicted final visual acuity | |
| No PL | 75 | 73 | 12 | 16 | 0 | 2 | 0 | 1 |
| PL HM | 25 | 17 | 25 | 26 | 13.5 | 11 | 0 | 2 |
| 1/200 to19/200 | 0 | 7 | 14 | 14 | 21.3 | 15 | 0 | 2 |
| 20/200 to 20/50 | 0 | 2 | 38 | 38 | 24.5 | 28 | 50 | 21 |
| ≥ 20/40 | 0 | 1 | 0 | 4 | 40.5 | 44 | 50 | 74 |
| P | 0.265 | 0.22 | 0.22 | 0.172 | ||||
Our study compared patients with open- and closed-globe injuries who developed traumatic cataracts. Open globe injury associated cataracts had improved vision following surgical treatment (Tables 6 and 7).
Various authors have reported different results in children with traumatic cataracts. Shah et al[4] reported 20/60 or better in 56% of their cases; Gradin Morgan[7,8] reported 20/60 or better in 64.7%; Krishnamachary et al[9] 6/24 or better in 74%; Kumar et al[10] 6/18 or better in 50%; Staffieri et al[11] 6/12 or better in 35%; Bekibele et al[12] 6/18 or better in 35.6%; Brar et al[13] 0.2 or better in 62%; Cheema et al[14] 6/18 in more than 68%; Karim et al[15] 0.2 or better in 62%; Knight-Nanan et al[16] 20/60 or better in 64%; Bienfait et al[17] 0.7 in 27%; and Anwar et al[18] 20/40 or better in 73%.
Using a polymethyl methacrylate lens, Verma et al[19] reported a visual outcome similar to that found in our study. Eckstein et al[20] and Zou et al[21] reported that primary intraocular lens implantation is important for a better visual outcome, similar to our results. Also similar to our results, Vajpayee et al[22] and Gupta et al[23] reported primary insertion of an intraocular lens with posterior capsule rupture.
Shah et al[24] reported that a better visual outcome was achieved when intervention was done between 5 and 30 d in adults with traumatic cataracts. As in our study, Rumelt et al[25] found no significant difference between primary and secondary implantation. Staffieri et al[11] performed primary implantation in 62% of cases vs 82% in our study. Kumar et al[10] and Verma et al[19] advocated primary posterior capsulotomy and vitrectomy for a better outcome; our results concurred with these findings.
We are not aware of any such study. Shah et al[26] reported a comparison between open- and closed-globe injuries in the general population. We are also not aware of another large series of successfully treated traumatic cataracts in children. In our study, final visual outcomes were achieved according to the OTS[27] prediction in children with traumatic cataracts. Lesniak et al[28] reported no significant differences between the final visual acuities and the visual acuities predicted by OTS in children. Sharma et al[29] proposed that the OTS calculated at the initial examination may be of prognostic value in children with penetrating eye injuries. However, Unver et al[30] suggested that OTS calculations may have limited value as predictors of visual outcome in a pediatric population. Lima-Gómez et al[31] reported estimates for a 6-mo visual prognosis, but some of the variables required evaluation by an ophthalmologist. Using the OTS, 98.9% of the eyes in the general population could be graded in a trauma room. Knyazer et al[32] reported the prognostic value of the OTS in zone-3 open globe injuries, and Yu Wai Man et al[33] claimed equal prognostic effectiveness of both the OTS and CART in the general population. Although similar findings have been reported by others[32,33], our study presents one of the largest reported databases following cases of pediatric traumatic cataracts classified according to BETTS. Despite the long time delay between injury and treatment in many of the cases in our study, the OTS was still relevant.
In conclusion, satisfactory visual outcome can be achieved in children with traumatic cataracts, and no significant difference was found amongst open and closed globe injuries in pediatric age group.
This study shows the comparative evaluation of patients having closed globe injuries and open globe injuries in those cases who developed traumatic cataract. Final visual result achieved in cases of traumatic cataracts in pediatric patients can fairly be foretold with the help of ocular trauma score.
Ocular trauma in children in less explored area of visual outcome following cataract surgery in children was studied here.
Surgical treatment has made a significant difference in outcome. No significant difference found in open globe and closed globe injury groups. Ocular trauma score is a valid predictive model for visual outcome in children.
This study addressed the probably largest published database for traumatic cataracts in children classified according to the Birmingham Eye Trauma Terminology System, and compared visual outcome according to ocular trauma score.
Morphological consideration of traumatic cataracts and treatment guidelines according to the morphological classification may be useful.
BETTS: Birmingham Eye Trauma Terminology System; OTS: Ocular trauma score.
This study presents important data that would be of interest.
P- Reviewer: BaykaraM, Nowak MS S- Editor: Song XX L- Editor: Wang TQ E- Editor: Wu HL
| 1. | Khatry SK, Lewis AE, Schein OD, Thapa MD, Pradhan EK, Katz J. The epidemiology of ocular trauma in rural Nepal. Br J Ophthalmol. 2004;88:456-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Abraham DI, Vitale SI, West SI, Isseme I. Epidemiology of eye injuries in rural Tanzania. Ophthalmic Epidemiol. 1999;6:85-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Alfaro DV, Jablon EP, Rodriguez Fontal M, Villalba SJ, Morris RE, Grossman M, Roig-Melo E. Fishing-related ocular trauma. Am J Ophthalmol. 2005;139:488-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Shah M, Shah S, Khandekar R. Ocular injuries and visual status before and after their management in the tribal areas of Western India: a historical cohort study. Graefes Arch Clin Exp Ophthalmol. 2008;246:191-197. [PubMed] |
| 5. | Kuhn F, Morris R, Witherspoon CD, Mester V. The Birmingham Eye Trauma Terminology system (BETT). J Fr Ophtalmol. 2004;27:206-210. [PubMed] |
| 6. | Zhang Y, Zhang J, Shi S. Determination of posterior lens capsule status in traumatic cataract with B-ultrasonography. Zhonghua Yanke Zazhi. 1998;34:298-299. [PubMed] |
| 7. | Gradin D, Yorston D. Intraocular lens implantation for traumatic cataract in children in East Africa. J Cataract Refract Surg. 2001;27:2017-2025. [PubMed] |
| 8. | Morgan KS. Cataract surgery and intraocular lens implantation in children. Curr Opin Ophthalmol. 1993;4:54-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Krishnamachary M, Rathi V, Gupta S. Management of traumatic cataract in children. J Cataract Refract Surg. 1997;23 Suppl 1:681-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Kumar S, Panda A, Badhu BP, Das H. Safety of primary intraocular lens insertion in unilateral childhood traumatic cataract. JNMA J Nepal Med Assoc. 2008;47:179-185. [PubMed] |
| 11. | Staffieri SE, Ruddle JB, Mackey DA. Rock, paper and scissors Traumatic paediatric cataract in Victoria 1992-2006. Clin Experiment Ophthalmol. 2010;38:237-241. [PubMed] |
| 12. | Bekibele CO, Fasina O. Visual outcome of traumatic cataract surgery in Ibadan, Nigeria. Niger J Clin Pract. 2008;11:372-375. [PubMed] |
| 13. | Brar GS, Ram J, Pandav SS, Reddy GS, Singh U, Gupta A. Postoperative complications and visual results in uniocular pediatric traumatic cataract. Ophthalmic Surg Lasers. 2001;32:233-238. [PubMed] |
| 14. | Cheema RA, LukarisAD . “Visual recovery in unilateral traumatic pediatric cataracts treated with posterior chamber intraocular lens and anterior vitrectomy in Pakistan.”. IntOphthalmol. 1999;23:85-89. |
| 15. | Karim A, Laghmari A, Benharbit M, Ibrahimy W, Essakali N, Daoudi R, Mohcine Z. Therapeutic and prognostic problems of traumatic cataracts. Apropos of 45 cases. J Fr Ophtalmol. 1998;21:112-117. [PubMed] |
| 16. | Knight-Nanan D, O’Keefe M, Bowell R. Outcome and complications of intraocular lenses in children with cataract. J Cataract Refract Surg. 1996;22:730-736. [PubMed] |
| 17. | Bienfait MF, Pameijer JH, Wildervanck de Blécourt-Devilee M. Intraocular lens implantation in children with unilateral traumatic cataract. Int Ophthalmol. 1990;14:271-276. [PubMed] |
| 18. | Anwar M, Bleik JH, von Noorden GK, el-Maghraby AA, Attia F. Posterior chamber lens implantation for primary repair of corneal lacerations and traumatic cataracts in children. J Pediatr Ophthalmol Strabismus. 1994;31:157-161. [PubMed] |
| 19. | Verma N, Ram J, Sukhija J, Pandav SS, Gupta A. Outcome of in-the-bag implanted square-edge polymethyl methacrylate intraocular lenses with and without primary posterior capsulotomy in pediatric traumatic cataract. Indian J Ophthalmol. 2011;59:347-351. [PubMed] |
| 20. | Eckstein M, Vijayalakshmi P, Killedar M, Gilbert C, Foster A. Aetiology of childhood cataract in south India. Br J Ophthalmol. 1996;80:628-632. [PubMed] |
| 21. | Zou Y, Yang W, Li S, Yue L. Primary posterior chamber intraocular lens implantation in traumatic cataract with posterior capsule breaks. Yanke Xuebao. 1995;11:140-142. [PubMed] |
| 22. | Vajpayee RB, Angra SK, Honavar SG, Titiyal JS, Sharma YR, Sakhuja N. Pre-existing posterior capsule breaks from perforating ocular injuries. J Cataract Refract Surg. 1994;20:291-294. [PubMed] |
| 23. | Gupta AK, Grover AK, Gurha N. Traumatic cataract surgery with intraocular lens implantation in children. J Pediatr Ophthalmol Strabismus. 1992;29:73-78. [PubMed] |
| 24. | Shah MA, Shah SM, Shah SB, Patel UA. Effect of interval between time of injury and timing of intervention on final visual outcome in cases of traumatic cataract. Eur J Ophthalmol. 2011;21:760-765. [PubMed] |
| 25. | Rumelt S, Rehany U. The influence of surgery and intraocular lens implantation timing on visual outcome in traumatic cataract. Graefes Arch Clin Exp Ophthalmol. 2010;248:1293-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Shah MA, Shah SM, Shah SB, Patel CG, Patel UA, Appleware A, Gupta A. Comparative study of final visual outcome between open- and closed-globe injuries following surgical treatment of traumatic cataract. Graefes Arch Clin Exp Ophthalmol. 2011;249:1775-1781. [PubMed] |
| 27. | Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002;15:163-165, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 362] [Cited by in RCA: 391] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 28. | Lesniak SP, Bauza A, Son JH, Zarbin MA, Langer P, Guo S, Wagner RS, Bhagat N. Twelve-year review of pediatric traumatic open globe injuries in an urban U.S. population. J Pediatr Ophthalmol Strabismus. 2012;49:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 29. | Sharma HE, Sharma N, Kipioti A. Comment on a new ocular trauma score in pediatric penetrating eye injuries. Eye (Lond). 2011;25:1240; author reply 1240-1241. [PubMed] |
| 30. | Unver YB, Acar N, Kapran Z, Altan T. Visual predictive value of the ocular trauma score in children. Br J Ophthalmol. 2008;92:1122-1124. [PubMed] |
| 31. | Lima-Gómez V, Blanco-Hernández DM, Rojas-Dosal JA. Ocular trauma score at the initial evaluation of ocular trauma. Cir Cir. 2010;78:209-213. [PubMed] |
| 32. | Knyazer B, Levy J, Rosen S, Belfair N, Klemperer I, Lifshitz T. Prognostic factors in posterior open globe injuries (zone-III injuries). Clin Experiment Ophthalmol. 2008;36:836-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 33. | Yu Wai Man C, Steel D. Visual outcome after open globe injury: a comparison of two prognostic models--the Ocular Trauma Score and the Classification and Regression Tree. Eye (Lond). 2010;24:84-89. [PubMed] |