Revised: January 7, 2014
Accepted: January 17, 2014
Published online: February 12, 2014
Processing time: 110 Days and 16.5 Hours
An armamentarium of the latest light and laser technologies are used by physicians of different disciplines to address a variety of aesthetic challenges in the periocular region and throughout the body. If improperly used, these modalities can inflict serious ocular injury on the patient, support personnel, and operator. It is paramount that providers involved in operating these technologies be knowledgeable about the physical and clinically relevant properties of the unit being used. This involves training in the proper utilization, appropriate treatment parameters, and safety measure for each. Selection of the appropriate eye protection is particularly important for both the patient and the personnel. It is also imperative for the laser operator to understand the range of potential ocular complications associated with the cosmetic use of lasers and lights, to recognize the signs and symptoms associated with ocular damage, and to provide efficient first aid measures should damage ensue. Possible ocular complications related to the cosmetic use of lasers and lights range from mild eyelid swelling and erythema to potentially blinding macular injury. Ocular injury may also be inflicted by the improper selection or placement of eye protection. A complete ophthalmologic evaluation and timely management of potential complications is mandated when there is any concern for ocular injury.
Core tip: The selection of the appropriate laser safety eyewear (LSE) and eye shields while performing laser and/or light therapy to the face and periocular region may, among other precautionary measures, prevent the occurrence of ocular complications that can sometimes be severe and even blinding. Since LSE is specific for each particular wavelength, extreme caution should be exercised to avoid selecting the inappropriate LSE. The choice of external or corneal shields for the protection of the patient’s eyes depends on the particular area to be treated.
- Citation: Sayed MS, Ko MJ, Ko AC, Lee WW. Ocular damage secondary to lights and lasers: How to avoid and treat if necessary. World J Ophthalmol 2014; 4(1): 1-6
- URL: https://www.wjgnet.com/2218-6239/full/v4/i1/1.htm
- DOI: https://dx.doi.org/10.5318/wjo.v4.i1.1
Light rays, whether naturally occurring (solar) or medically used, have a range of effects on the eye and the surrounding tissues depending on the wavelength of light, the nature of exposure, and whether protective mechanisms are applied. Lights can be classified according to their wavelength on the electromagnetic spectrum into ultraviolet rays (UVR; wavelength 100-400 nm), visible light (400-700 nm), infrared (700-1200 nm) and far infrared (> 1200 nm). UVR can be further subdivided to UV-A (315-400 nm), UV-B (280-315 nm) and UV-C (100-280)[1]. Only UV-A and a small portion (10%) of UV-B reach the earth surface and therefore have an opportunity for ocular exposure.
Laser radiation wavelengths fall within the ultraviolet, visible and infrared wavebands of the electromagnetic spectrum. The shorter, biologically active wavelengths (below 300 nm) are mostly absorbed at the cornea, while the longer wavelengths pass through the cornea to reach the lens and retina[1]. Lights and lasers with wavelengths from 400 nm to 1400 nm (retinal hazard region) are particularly dangerous as they can be transmitted through the clear media of the eye and become focused on the retina. While a portion of the retinal hazard zone falls within the visible light spectrum (400-700 nm), which will trigger the blink reflex and protect the eye, the invisible portion falling in the 700-1400 nm waveband constitutes a major window of danger.
The main source of UVR that the eye and periocular tissues are exposed to is sunlight. A range of conditions involving the eyelids, the ocular surface, the crystalline lens, the retina and choroid have been strongly linked to acute or cumulative UVR exposure[1]. Detailed discussion of UVR effects on the eye and protection from solar radiation is beyond the scope of this article.
Laser properties such as coherence and low divergence, together with the focusing mechanism of the eye optical system, can result in significant ocular injury if specific safety measures are not strictly followed. This can be particularly devastating if the retina is the recipient of end-organ damage. Because of the sensitivity and vulnerability of the eye to overstimulation, laser safety guidelines are largely established on injury thresholds of the ocular structures, especially the retina[2]. Furthermore, lasers are classified according to the ability of the laser beam to cause biological damage to the eye or skin during use (Table 1)[3,4].
| Class 1 | Considered to be incapable of producing damaging radiation levels during operation and are safe under all conditions of normal use to naked eye or magnifying optics. These systems are exempt from any control measures or other forms of surveillance. Examples are lasers used in diagnostics in laboratories |
| Class 1M | Considered to be incapable of producing hazardous exposure conditions during normal operation unless the beam is viewed with an optical instrument (magnifying optics) |
| Class 2 | Low power laser systems; they emit in the visible portion of the spectrum (400-700 nm), and are considered safe because aversive mechanisms (i.e., the blink reflex) afford protection. An example is the helium-neon laser (laser pointer) |
| Class 2M | Emit in the visible portion of the spectrum. Eye protection is normal afforded by the aversion response for unaided viewing. However, these systems are potentially hazardous when viewed with certain optical aids |
| Class 3 | Medium power laser systems; they may be hazardous under direct and specular reflection viewing conditions. They are normally not a diffuse reflection or fire hazard. An example of a class 3 laser is the Nd:YAG laser used in ophthalmology. There are 2 subclasses: 3R and 3B |
| Class 3R | Can be hazardous under some direct and specular reflection viewing condition if the eye is appropriately focused and stable, but the probability of an actual injury is small. They will not pose either a fire-hazard or diffuse-reflection hazard. They are safe if handled carefully with restricted beam viewing |
| Class 3B | May be hazardous under direct and specular reflection viewing conditions, but are normally not a diffuse reflection or fire hazard |
| Class 4 | High power systems and are the most dangerous. They are hazardous to the eye or skin from the direct beam, may pose a diffuse reflection or fire hazard, and may produce laser-generated air contaminants and hazardous plasma radiations. Examples include the CO2, argon, continuous wave Nd:YAG, and pulsed dye laser |
Absorption and scattering are important concepts in understanding tissue response to laser and light exposure[4]. Absorption depends on the tissue’s affinity for the laser’s wavelength. Specific wavelengths are preferentially absorbed by a specific tissue chromophore which has a different absorption spectrum determined by its chemical structure. The most clinically relevant organic chromophores are water, hemoglobin and melanin. For example, to treat a vascular lesion, oxyhemoglobin, the predominant form of hemoglobin, is chosen as a target chromophore. It has absorption peaks of 418 nm, 542 nm, and 577 nm.
Scattering is also related to wavelength. Shorter wavelength lasers (cold lasers; below visible spectrum; e.g., Excimer laser) have a greater scatter and less tissue penetration, while the reverse is true for longer wavelength lasers[4]. The action of lasers also depends on the power (watts/s; joules/s), the spot size (cm2) and the duration of action. With larger spot size, there is less scattering but deeper tissue penetration.
Although lasers target specific chromophores, the surrounding scatter and the resulting thermal effect can cause collateral damage[4]. Thermal damage occurs when enough energy is absorbed by a suitable chromphore at a faster rate than the resultant heat can be dissipated[5,6]. Also, while the main tissue chromophores are targeted, other ocular structures that are also rich in these chromophores are susceptible to inadvertent damage (e.g., retina rich in hemoglobin and melanin; uvea rich in melanin; cornea and lens rich in water).
Mechanisms of laser injuries to the eye vary according to the type of laser used and the properties of the particular ocular structures. Lasers and lights in the retinal hazard region (wavelength 400-1400 nm) can cause significant injury to the macula due to the focusing ability of the crystalline lens. For example, argon laser (wavelength 488 nm and 515 nm) is mainly absorbed by vessels and melanin. If improper eye protection is used, the laser can pass through the cornea, become focused by the lens onto the retina, and result in heat denaturation of proteins (photocoagulation)[4,7].
Lasers in the near- and mid-infrared spectrum (e.g., Nd:YAG, wavelength 1064 nm, used for various indications such as vascular lesions, hair removal and rejuvenation) have longer wavelengths and are weakly attracted to melanin, relative to other lasers, with subsequently less melanin chromophore absorption[8], but can still cause retinal damage[4,9]. It should be emphasized that lasers in the 700-1400 nm band of the spectrum are particularly hazardous because while they are invisible to the eye, they can still cause serious ocular injury.
Although lasers in the far infrared spectrum (wavelength 1400-10600 nm) cannot penetrate the ocular tissues far enough to reach the retina, these wavelengths can still cause injury to the cornea and crystalline lens. Carbon dioxide (CO2) laser (wavelength 10600 nm) is an ablative laser used to achieve skin tightening and for the treatment of certain vascular lesions such as orbital lymphangioma[7]. Its main target chromophore is intracellular water, which is instantaneously vaporized with application of the laser, resulting in lateral thermal damage and coagulative necrosis of the surrounding tissues. The CO2 laser can cause corneal or scleral injury due to their rich water content[4,7].
Erbium:YAG laser (wavelength 2940 nm), another ablative laser, which can also be used in a fractional manner, is more efficiently absorbed by water and collagen, inducing less thermal damage than CO2 laser. Complications of these lasers include erythema, hyper- and hypo-pigmentation, skin infections, and accidental corneal injury.
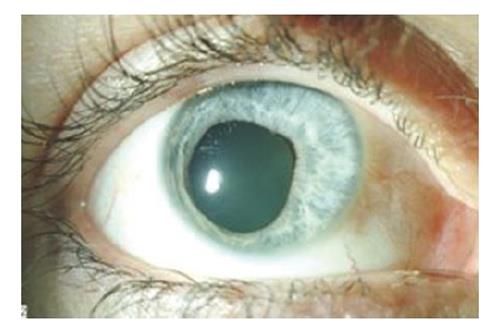
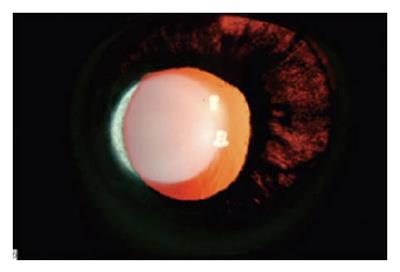
Intense pulsed light (IPL) is a non-ablative technology used to treat telangiectatic lesions, skin pigmentation and abnormal skin texture[10]. The device emits non-collimated, non-coherent lights of multiple wavelengths (500-1200 nm; within the retinal hazard zone). Although it is, therefore, not classified as a laser, this modality can still cause significant ocular damage. Pigmented structures, like the iris, are extremely susceptible to accidental injury during IPL treatment. The senior author (WL) published a retrospective review of two cases with permanent ocular damage secondary to IPL performed at outlying facilities and referred for management of complications[10]. Both patients developed severe eye pain, anterior uveitis, pupillary distortion (Figure 1), permanent iris atrophy (Figure 2) and photophobia. There tends to be a false sense of security when dealing with light therapy because many operators do not realize the potential damage that this technology can cause to the eye. Most damage occurs when operators either reposition the eye shields to treat awkward areas such as the medial canthus, or they don’t use eye protection at all. It is important to know the dangers of light therapy as well as laser therapy.
There are numerous reports of inadvertent laser ocular injuries in the literature. Park et al[11] reported a case of a patient who sustained macular injury following accidental exposure to Q-switched Nd:YAG laser (1064 nm). The patient experienced instantaneous bright flash light perception followed by loss of vision (best corrected visual acuity 20/100 in affected eye immediately following exposure). Examination revealed metamorphopsia and central scotoma by Amsler grid, and a laser macular burn and vitreous hemorrhage by fundoscopy. Despite treatment with oral prednisolone (60 mg daily with a 10 mg/wk taper), the patient developed an epiretinal membrane that spontaneously regressed later and visual acuity remained 20/100. At six-year follow up, the patient’s visual acuity had not improved and fundus exam revealed a centrally pigmented chorioretinal scar in the macula.
Marcus et al[12] reported another case of a laser ocular injury where the patient was exposed to YAG laser without safety goggles when the triggering mechanism of the laser accidentally went off. The patient noticed immediate loss of vision and a black spot in the center of her vision. She could only count fingers one hour after exposure. Fundus examination revealed a mild vitreous hemorrhage near the fovea, and fluorescein angiography showed two choroidal ruptures at right angles to each other through the center of the fovea. A full thickness macular hole developed a week later, and subretinal neovascularization was identified alongside the superior edge of the macular hole six months later, with a subsequent metaplastic scar formation and enlargement of the macular hole. The visual acuity stabilized at 20/200 in the affected eye as documented in a nine-year follow up. Surgical treatment of the patient was not attempted.
Sun et al[13] reported a case of an early subfoveal choroidal neovascular membrane (CNV) in a technician who accidentally looked into the path of a 532 nm pulsed green light beam. The patient experienced an immediate flash of bright pink light followed by an immovable shadow in the central vision four hours later. Examination only five days following exposure revealed a best corrected visual acuity of 0.08 (decimal) and a small subfoveal grayish-yellow lesion on fundoscopy representing a CNV. Fundus fluorescein angiography showed a lacy hyperfluorescent pattern with subsequent leakage. The patient received no treatment on the ground of cost and on four-month follow up her best corrected visual acuity was found to have improved to 0.01 (decimal) while the lesion was unchanged in appearance by fundoscopy.
Harris et al[6] described ten cases of laser ocular injury that occurred in the United States military between 1984 and 2000. Most of the cases were caused by accidental exposure to Q-switched Nd:YAG laser (1064 nm). Eye protection was not worn by any of the victims at the time of injury. Injuries described included vitreous hemorrhage, preretinal hemorrhage, macular hemorrhage, subretinal hemorrhage, vitreous detachment, parafoveal scarring, progressive macular scarring, macular pucker, retinal burns, macular/retinal edema, retinal pigment epithelial disruption, macular hole, epiretinal traction membranes, central serous retinopathy and punctate macular lesions.
Eye protection during cosmetic procedures with lights and lasers during treatment administration is of paramount importance for the patient, the operator, the observer and the assistant[14]. With the advent of new laser devices operating at multiple wavelengths, understanding the hazards of lasers and lights has become even more critical. Despite the increased knowledge of lasers and laser safety, eye injuries in the workplace still occur, even with the use of protective eyewear.
General protective measures that guard against accidental laser injuries include warning signage and proper personnel training. Laser warning signs must be placed at the entrance of the laser treatment room when lasers are operating. Adequate laser safety training for personnel must be provided. Extra care should be taken when the laser is taken off “standby” mode, as lasers can be initiated by accidental pressing of the foot switch while the hand-piece is directed away from the patient or toward their unprotected eye[14].
Potential injury to the eyelids can be minimized by adjusting the treatment parameters appropriately, using cooling devices during the procedure, applying ice packs after the procedure, and elevating the head of the bed. Patients should be informed of what to expect pre- and post-treatment, like edema and erythema. Potential ocular complications can be avoided or minimized by means of careful application of topical anesthetics, proper sizing, sterilization and gentle placements of corneal shields. Excessive pressure on the globe during treatment should be avoided. Corneal shields should be removed carefully, and the lids cleansed appropriately post-treatment.
Early recognition of ocular complications is critical. Symptoms and signs of eyelid complications include erythema, edema, pain, burning, abnormal sensation of lids and pinpoint bleeding. Laser damage to the eye itself may go unrecognized initially. It can be painless, or the operator might hear a “pop” sound. Patients might complain of photophobia, redness, tearing or blurry vision following the procedure, Other clinical signs include pupil abnormalities or a new blind spot in the patient’s vision. Subconjunctival hemorrhage, infection, chemical irritation and corneal abrasion can occur as a result of laser and/or protective eyewear injury. All of these signs and symptoms can represent serious, sight-threatening laser or light injuries to the cornea, sclera, iris, or retina. If the clinician is suspicious of an injury, a full, thorough ophthalmologic evaluation must be performed in a timely manner.
Choosing the appropriate eye protection for everyone in the treatment room is the key to prevention of ocular damage. The American National Standards Institute has established guidelines for laser safety and defines maximum permissible exposure (MPE) levels, which is the amount of laser radiation exposure allowable without hazardous effects for specific laser wavelengths[3].
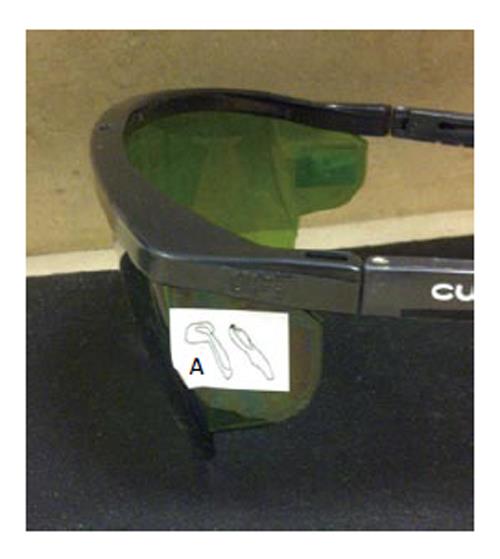
Each laser requires a specific type of eyewear depending on its specific wavelength and peak irradiance[12]. Optical density (OD) of the LSE determines its ability to reduce the energy of a specific laser wavelength to a safe level (below MPE). The OD of a specific goggle should be engraved on the side of the eyewear (Figure 3). Occasionally, a drawing of the hand-piece is placed on the side of the goggle (Figure 4) to avoid confusion. OD is expressed as the logarithmic value of the incident beam irradiance divided by the transmitted beam irradiance. As such, an OD of 1.0 allows 0.1% of laser energy to be transmitted through the goggle lens, while an OD of 6 allows only 0.000001% of laser energy to be transmitted, virtually protecting the eye from direct beam exposure.
Another important factor to consider when choosing LSE is the visible light transmittance (VLT)[15]. LSE should be able to filter out the laser wavelength while transmitting as much light as possible so the operator can visualize the treatment area. The ideal LSE should have both a high OD and VLT for the particular wavelength of the laser used. The style, field of view and comfort of the LSE are also important as they can affect the compliance of personnel. Regarding IPL, the LSE able to protect in this entire range (400-1200 nm) would offer little visibility (low VLT). Goggles with a fast shutter mechanism that detects light intensity and immediately dims the filter can be utilized for IPL (Figure 5).
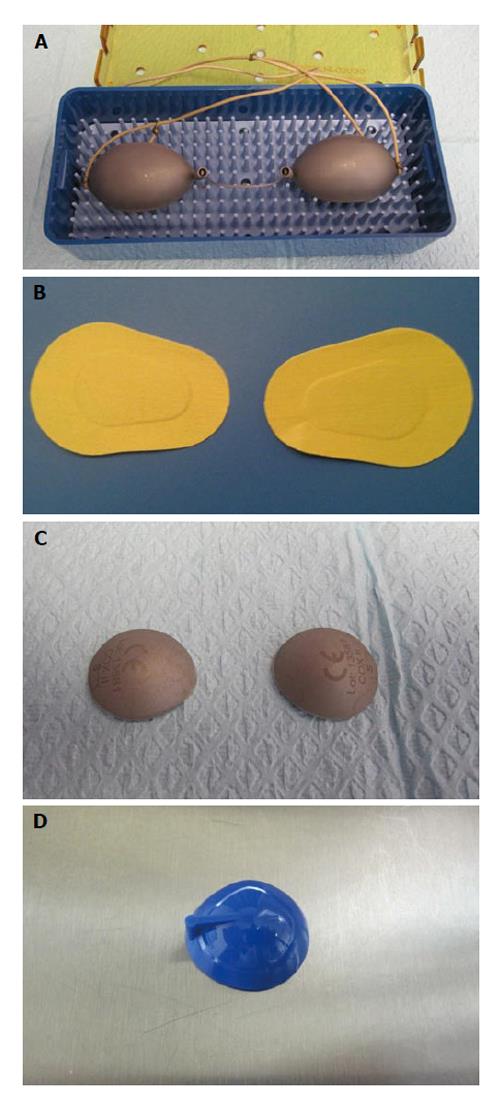
Eye protection for the patient depends on the area to be treated. If the crows’ feet, face, or skin overlying the orbital rim are treated, external eye protection, made of either stainless steel (Figure 6A) or stick-on fabric (e.g., Coverlet Eye Occlusor, BSN Medical Inc., NC) (Figure 6B), can be used. When using the adhesive eye patches, the skin should be cleansed and dried off. Patients should be asked about contact allergies, as the adhesive patches may contain latex.
If the treatment is to be performed on the eyelid itself, corneal shields should be used. They allow treatment all the way up to the lash line. Furthermore, they provide a taut surface over which the laser hand piece can more easily glide.
Corneal shields, however, have the potential to induce corneal abrasions if extreme care is not taken. The operator should make sure that there are no contraindications for corneal shield placement, such as recent ocular trauma or corneal surgery. Contact lenses should be removed and 1-2 topical anesthetic drops instilled before placing the corneal shield. Corneal shields should be checked for sharp edges and for debris prior to each use. Stainless steel corneal shields (Figure 6C) can be gas or steam autoclaved. They are buffed and electro-polished to a smooth surface, and are less likely to conduct heat. However, they can be more susceptible to the development of sharp edges. Methyl methacrylate corneal shields (Figure 6D) can be gas autoclaved. However, there is a risk of thermal conduction associated with their use if the laser beam comes in contact with the shields.
All operators of lasers should be able to recognize ocular laser injury and be prepared to provide the necessary first-aid measures. It is important for ophthalmologists performing laser treatments to have an eye wash station, a slit lamp, fluorescein stain, dilating eye drops and lenses for possible fundoscopy. A copious, profuse irrigation with sterile eyewash solution should be performed if the patient complains of foreign-body sensation, irritation or pain. A thorough slit lamp evaluation with corneal fluorescein staining may be required. Blurry vision after eye shields are removed may also occur secondary to anesthetic, tears, or mucous on the surface of the eye, and is first treated with copious irrigation with saline or eyewash. If symptoms persist or if the patient complains of photophobia, blepharospasm or significant diminution of vision, a thorough slit lamp examination and fundoscopy should be performed. Appropriate referral to a subspecialist is warranted in the unfortunate event of a significant injury, particularly to the retina. Cases are then managed according to the type of injury inflicted. Unfortunately, many of the patients who sustain laser ocular injuries with macular involvement end up with permanent visual loss.
The role of lasers and lights has become increasingly popular in aesthetic medicine. Due to the physical properties of light, tissue-light interaction and human error, damage to ocular structures can occur if precautionary measures are not strictly followed. Proper training of personnel on laser and light properties, use and safety is key to preventing serious ocular and soft tissue complications in the patient as well as the personnel. Potential ocular injury can be minimized by adhering to a relatively simple set of safety measures, including the choice of appropriate protective eyewear and eye shields. If ocular injury is suspected, prompt ophthalmologic evaluation and treatment is mandatory.
P- Reviewers: Kim H, Mahendradas P, Shih YF S- Editor: Song XX L- Editor: A E- Editor: Liu SQ
| 1. | Yam JC, Kwok AK. Ultraviolet light and ocular diseases. Int Ophthalmol. 2013;May 31; Epub ahead of print. [PubMed] |
| 2. | Mihran RT. Interaction of laser radiation with structures of the eye. IEEE Trans Educ. 1991;34:250-259. [DOI] [Full Text] |
| 3. | Laser Institute of America. American National Standard for Safe Use of Lasers. United States of America: Laser Institute of America 2007; . |
| 4. | Ha RY, Burns JL, Hoopman JE, and Burns AJ. Lasers in plastic surgery. Selected Readings Plast Surg. 2003;9. |
| 5. | Barkana Y, Belkin M. Laser eye injuries. Surv Ophthalmol. 2000;44:459-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 135] [Article Influence: 5.4] [Reference Citation Analysis (1)] |
| 6. | Harris MD, Lincoln AE, Amoroso PJ, Stuck B, Sliney D. Laser eye injuries in military occupations. Aviat Space Environ Med. 2003;74:947-952. [PubMed] |
| 7. | Blanco G, Soparkar CN, Jordan DR, Patrinely JR. The ocular complications of periocular laser surgery. Curr Opin Ophthalmol. 1999;10:264-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Dayan SH, Vartanian AJ, Menaker G, Mobley SR, Dayan AN. Nonablative laser resurfacing using the long-pulse (1064-nm) Nd:YAG laser. Arch Facial Plast Surg. 2008;5:310-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 46] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 9. | Gao L, Dong F, Chan WM. Traumatic macular hole secondary to Nd:YAG laser. Eye (Lond). 2007;21:571-573. [PubMed] |
| 10. | Lee WW, Murdock J, Albini TA, O’brien TP, Levine ML. Ocular damage secondary to intense pulse light therapy to the face. Ophthal Plast Reconstr Surg. 2011;27:263-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 11. | Park DH, Kim IT. A case of accidental macular injury by Nd: YAG laser and subsequent 6 year follow-up. Korean J Ophthalmol. 2009;23:207-209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Marcus DF, Ravin J. A new report of laser eye injury. Surv Ophthalmol. 2000;45:262-263. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 13. | Sun Z, Wen F, Li X, Wu D. Early subfoveal choroidal neovascularization secondary to an accidental stage laser injury. Graefes Arch Clin Exp Ophthalmol. 2006;244:888-890. [PubMed] |
| 14. | Sliney DH. Laser safety. Lasers Surg Med. 1995;16:215-225. [PubMed] |
| 15. | Occupational Safety and Health Administration. OSHA Instruction PUB 8-1.7. Guidelines For Laser Safety and Hazard Assessment. United States Department of Labor: Washington DC 1991; . |