Copyright
©2014 Baishideng Publishing Group Inc.
World J Ophthalmol. Aug 12, 2014; 4(3): 35-46
Published online Aug 12, 2014. doi: 10.5318/wjo.v4.i3.35
Published online Aug 12, 2014. doi: 10.5318/wjo.v4.i3.35
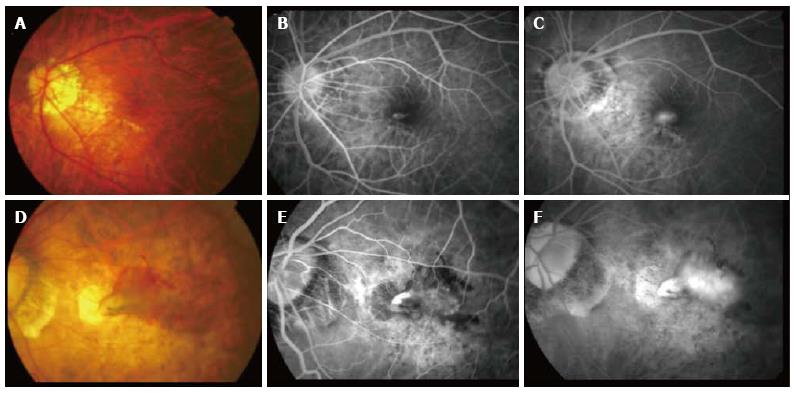
Figure 1 Clinical features of a typical choroidal neovascularization secondary to pathological myopia.
(A) Color fundus photography and corresponding fluorescein angiography (FA) (B and C) showing a younger patient with a small choroidal neovascularization lesion adjacent to the lacquer crack compared to (D) color fundus photograph and corresponding FA (E and F) showing an older patient with a much larger lesion with significant intraretinal fluid and extensive background atrophic changes.
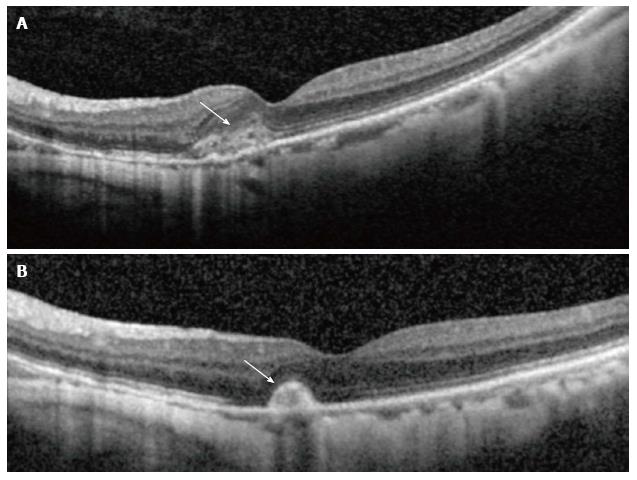
Figure 2 Optical coherence tomography showing corresponding changes in activity.
(A) Shows hyperreflective lesion corresponding to a small juxtafoveal myopic choroidal neovascularization (arrow) located above the retinal pigment epithelial cell layer with minimal exudation. After 3 mo (B), the lesion had scarred up, represented by a highly reflective lesion with sharp outline, and no intraretinal fluid is seen, which suggests an inactive lesion (arrow).
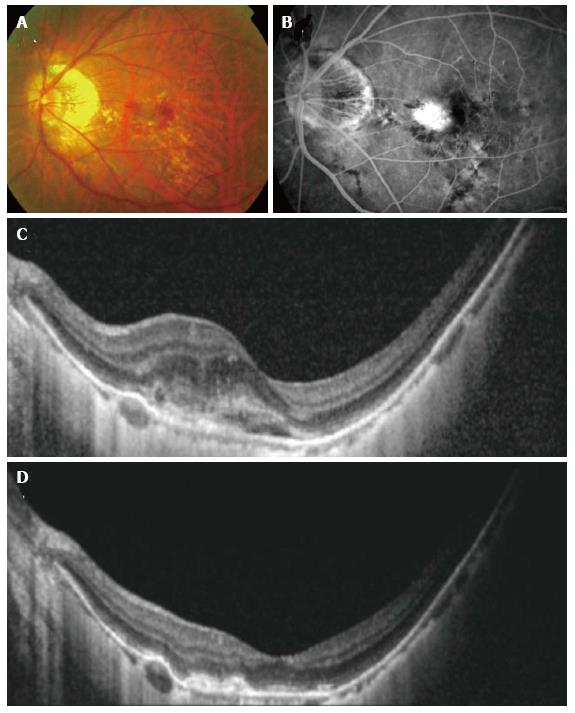
Figure 3 Resolution seen with anti-vascular endothelial growth factor treatment in myopic.
Choroidal neovascularization (CNV) color fundus photograph (A), fluorescein angiography (FA) (B) and optical coherence tomography (OCT) (C) showing a larger juxtafoveal myopic CNV with significant amount of intraretinal fluid. Note the lacquer cracks which are clearly visible on the FA. After a course of intravitreal bevacizumab, OCT demonstrated resolution of intraretinal fluid and consolidation of the CNV (D).
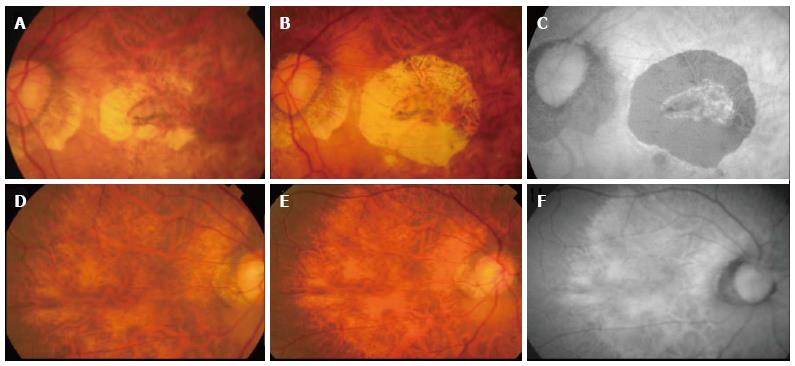
Figure 4 Progression of atrophy around treated choroidal neovascularization.
Color fundus photograph (A) showing inactive choroidal neovascularization (CNV) after 1 year therapy with ranibizumab, color fundus photography (B) showing increase in CNV related chorioretinal atrophy two years later. No further therapy was given during the intervening period. Autofluorescence imaging (C) demonstrating clearly the area of retinal pigment epithelial atrophy as hypoautofluorescent area. The fellow eye showed diffuse atrophy but no significant progression was seen during the same follow-up period (D-F).
- Citation: Teo K, Cheung CMG. Choroidal neovascularization secondary to pathological myopia. World J Ophthalmol 2014; 4(3): 35-46
- URL: https://www.wjgnet.com/2218-6239/full/v4/i3/35.htm
- DOI: https://dx.doi.org/10.5318/wjo.v4.i3.35