Published online Aug 10, 2014. doi: 10.5317/wjog.v3.i3.138
Revised: May 8, 2014
Accepted: July 18, 2014
Published online: August 10, 2014
Processing time: 264 Days and 3 Hours
A leiomyoma is a benign tumor originating from non-striated muscle that is typically found in the uterus. Intravenous leiomyomatosis is a rare form found within the veins, usually associated with uterine fibroids, and tends to recur. These masses can spread from the uterus throughout the venous system. A rare case involving a subendothelial leiomyoma found in an umbilical cord artery is presented in this article. A 21-year-old patient presented with symptoms of preterm labor, which resulted in the premature birth of a female below the 10th percentile for 24-wk gestational age. The newborn died three days later, and microscopic analysis of the umbilical cord revealed occlusion of the artery by nodular structures. The antepartum diagnosis of intravascular leiomyoma was identified by immunohistochemistry showing that approximately 70% of all tumor cells were diffusely positive for smooth muscle markers, including desmin and smooth muscle actin. These findings indicate the possibility of a pathologic association between the umbilical cord leiomyoma, restriction of fetal growth and preterm delivery due to impaired circulation of blood in the umbilical cord.
Core tip: Leiomyoma is a benign tumor originating from non-striated muscle that is rare in tissues outside of the uterus. This article presents an extremely rare case of umbilical cord artery subendothelial leiomyoma.
- Citation: Rovas L, Dauksas R, Simavicius A. Leiomyoma of the umbilical cord artery: A case report. World J Obstet Gynecol 2014; 3(3): 138-140
- URL: https://www.wjgnet.com/2218-6220/full/v3/i3/138.htm
- DOI: https://dx.doi.org/10.5317/wjog.v3.i3.138
Intravenous leiomyomatosis (IVL) is a rare smooth muscle tumor found within the veins of the uterus. The masses are benign-appearing but can exit the uterus and spread throughout the venous system[1]. This condition is related to benign metastasizing leiomyoma, in which the masses appear in distant locations such as the lung, heart and kidneys.
Tumors of the umbilical cord are rare, and cases of subendothelial leiomyoma are even more infrequent. To our knowledge, there are no published reports concerning umbilical cord leiomyomas. However, we recently encountered a case of an unusual non-trophoblastic tumor in an umbilical cord that was diagnosed during histochemical examination after childbirth.
A healthy, 21-year-old multiparous pregnant woman presented at Siauliai Hospital at 24 wk of gestation because of bleeding and uterine contractions. The patient had no significant medical history except for a miscarriage at 13 gestational weeks one year before. The current pregnancy was spontaneous without any problems to date.
Transvaginal and transabdominal ultrasound did not detect any lesions within the fetus, placenta or umbilical cord. The estimated weight of the fetus was less than the 10th percentile. A blood analysis did not indicate the presence of any inflammatory processes. Regular contractions were detected during cardiotocography. Despite treatment with nifedipine, a selective calcium channel inhibitor used to stop premature uterine contractions, a spontaneous preterm birth occurred. The extremely premature newborn died after three days, and no anomalies were found at autopsy. The maternal surface and membranes of the placenta were unremarkable.
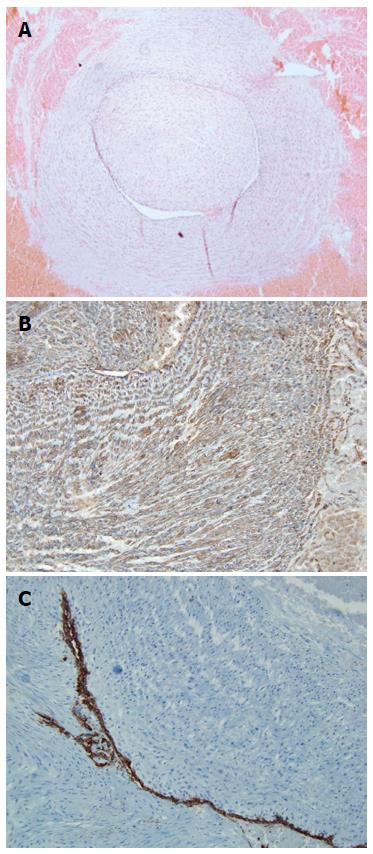
The umbilical cord measured 50 cm in length and was inserted centrally. Microscopic examination of an umbilical cord specimen revealed that arteries were occluded by polyploid nodular structures consisting of oblong, mitotic non-active cells, which formed patches in some places. Further analysis revealed a lesion lined with endothelium (Figure 1A). A diagnosis of intravascular leiomyoma was confirmed by immunohistochemistry that showed that the tumor cells were diffusely positive for smooth muscle markers, including desmin and smooth muscle actin (Figure 1B). Approximately 70% of the tumor cells showed cytoplasmic actin immunoreactivity. Tumor cells were also immunoreactive for antibodies against CD34 (Figure 1C).
The histogenesis of primary neoplastic alterations of placenta and umbilical cord are divided into two main groups[2]. They can be of a trophoblastic origin, including placental trophoblastic tumors, choriocarcinomas and hydatidiform moles, or non-trophoblastic, such as in chorioangioma and teratomas. Leiomyomas are of the second group of non-trophoblastic origin, which are extremely rare in the umbilical cord[3]. However, non-trophoblastic tumors are asymptomatic, and can remain undetected during examination of secundines, only being detected incidentally[2].
IVL is a nonmalignant tumor usually confined to the pelvic venous system and histologically characterized as a smooth muscle tumor mass growing within the uterus[4,5]. The cardinal microscopic feature is the protrusion of a smooth muscle endothelium-covered tumor into the vessels. Vascular leiomyomas may be difficult to distinguish from hemangiomas, which are more commonly found in the umbilical cord, and are cavernous[6]. Although IVL are typically confined to the uterine veins, they can progress along the veins into the inferior vena cava, and have been described within intracaval, intracardiac, intrarenal and pulmonary arteries[7,8]. Of the reported cases of IVL[4], none were detected in umbilical cord.
The case described in this article is the first known report of IVL in an umbilical cord artery. There were no suspicions concerning an umbilical cord tumor before delivery, and the leiomyoma was detected only during microscopic examination after birth. It is not clear how the leiomyoma extended in to umbilical cord artery. The umbilical cord forms within the body stalk of the developing embryo from the omphalomesenteric duct, yolk sac and the allantoic duct at around 6 wk into the gestational period[9]. IVL grows in the uterine vascular tree and can presumably metastasize into the fetal-maternal circulation. Although the cause of the fetal growth restriction and preterm delivery in this case is unknown, it is possible that the umbilical cord artery pathology and impaired blood circulation resulting from the leiomyoma contributed.
A healthy 21-year-old pregnant women presented with symptoms of preterm labor.
Premature labor, intrauterine growth restriction.
Premature labor, abruptio placenta.
Blood analysis did not reveal any sign of inflammatory processes.
Pregnancy: 24 wk gestation with normal anatomic development of the fetus. Cervix: 3 cm; normal placenta and umbilical cord. Intrauterine growth restriction.
Leiomyoma.
The patient was treated with nifedipine (calcium channel blocker).
The CD34 protein is a member of a family of single-pass transmembrane proteins expressed in early hematopoietic and vascular-associated tissue.
This case report not only describes the extremely rare intravenous locations of leiomyomas, but also suggests that all available methods should be used to ascertain causes of poor pregnancy outcomes.
This article presents the first known report of an intravenous leiomyoma within the umbilical cord. The tumor was diagnosed after immunohistochemical analysis to confirm the origin.
P- Reviewer: Dilek N, Mark Reynolds T S- Editor: Wen LL L- Editor: A E- Editor: Wu HL
| 1. | Worley MJ, Aelion A, Caputo TA, Kent KC, Salemi A, Krieger KH, Goldstein MJ, Kuo DY, Slomovitz BM. Intravenous leiomyomatosis with intracardiac extension: a single-institution experience. Am J Obstet Gynecol. 2009;201:574.e1-574.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Fiutowski M, Pawelski A. Primary nontrophoblastic tumors of the placenta. Ginekol Pol. 1996;67:515-519. [PubMed] |
| 3. | Shipp TD, Bromley B, Benacerraf BR. Sonographically detected abnormalities of the umbilical cord. Int J Gynaecol Obstet. 1995;48:179-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Norris HJ, Parmley T. Mesenchymal tumors of the uterus. V. Intravenous leiomyomatosis. A clinical and pathologic study of 14 cases. Cancer. 1975;36:2164-2178. [PubMed] |
| 5. | Lam PM, Lo KW, Yu MY, Wong WS, Lau JY, Arifi AA, Cheung TH. Intravenous leiomyomatosis: two cases with different routes of tumor extension. J Vasc Surg. 2004;39:465-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 108] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Kurman RJ. Blaustein’s Pathology of the Female Genital Tract. 5th ed. Berlin: Springer-Verlag 2001; 574-575. |
| 7. | Du J, Zhao X, Guo D, Li H, Sun B. Intravenous leiomyomatosis of the uterus: a clinicopathologic study of 18 cases, with emphasis on early diagnosis and appropriate treatment strategies. Hum Pathol. 2011;42:1240-1246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 87] [Article Influence: 6.2] [Reference Citation Analysis (1)] |
| 8. | Ling FT, David TE, Merchant N, Yu E, Butany JW. Intracardiac extension of intravenous leiomyomatosis in a pregnant woman: A case report and review of the literature. Can J Cardiol. 2000;16:73-79. [PubMed] |
| 9. | Moore KL, Persuad TVN. The Developing Human: clinically oriented embryology. 6th ed. Philadelphia: WB Saunders 1998; 130-136. |