Published online Aug 10, 2014. doi: 10.5317/wjog.v3.i3.134
Revised: January 25, 2014
Accepted: April 16, 2014
Published online: August 10, 2014
Processing time: 311 Days and 1.6 Hours
AIM: To evaluate the role of lubricant gel in the cytology of a Pap smear and whether it results in an improvement in the discomfort experienced by women while undergoing Pap smear screening.
METHODS: A total of 151 women were analyzed in the study. After screening for inclusion criteria, a Pap smear was taken with no lubricant in all the women and the discomfort experienced was rated on a visual analogue scale. The women underwent a second Pap smear on the next visit using a lubricant gel and were again rated on a visual analogue scale for the discomfort felt. The pathologist was blinded to the fact of whether the lubricating gel was used.
RESULTS: The number of unsatisfactory smears in the no gel group was 3 vs 5 in the gel group, P < 0.05. However, a significant difference (P = 0.00) was observed in the visual analogue pain score in both groups, suggesting that application of lubricant gel over the speculum improves the pain experienced by women.
CONCLUSION: Using a small amount of lubricant over the speculum does not impair cervical cytology but significantly improves the discomfort experienced by women while undergoing a Pap smear.
Core tip: Vaginal speculum lubrication has no effect on cervical cytology and improves the discomfort experienced in Pap smear screening.
- Citation: Madaan M, Singh A, Puri M, Kaur H, Trivedi SS. Effect of vaginal speculum lubrication on cervical cytology and discomfort during smear examination. World J Obstet Gynecol 2014; 3(3): 134-137
- URL: https://www.wjgnet.com/2218-6220/full/v3/i3/134.htm
- DOI: https://dx.doi.org/10.5317/wjog.v3.i3.134
Worldwide, cervical cancer is the third most common cancer in women. In 2008, there were an estimated 529000 new cases of cervical cancer, of which over 85% occurred in developing countries[1]. Although these numbers are staggering, there has been a marked improvement in early detection of cervical carcinoma with the advent of Pap smears as a screening test. Despite this, there are many women who do not get regular screening with Pap smears. The reasons could be lack of health education, lack of health insurance, cultural barriers, discomfort[2] or anxiety regarding the procedure. Health care providers can address this issue by minimizing the patient’s discomfort while performing a Pap smear. Lubricating the speculum can reduce the patient’s discomfort and improve the woman’s compliance with a Pap smear examination.
The routine teaching in gynecology over the years has discouraged the use of gel lubricant because of concerns that the lubricant might interfere with the cytology results[3]. A few studies in the literature have addressed this issue and others have also raised some concerns.
We designed this study to formally investigate whether gel interferes with cervical cytology and whether it has any effect on the pain perception of the woman.
The study was conducted at Lady Hardinge Medical College and Smt Sucheta Kriplani Hospital, New Delhi from November 2010 to July 2011. The study was approved by the Institutional Review Board of the hospital. Women aged 18 to 50 years attending the gynecology outpatient clinic were enrolled in the study. Women presenting with infectious gynecological complaints, genital bleeding or with history of cervical cancer, chronic pelvic pain, hysterectomy or allergy to gel lubricant were excluded from the study. Prior informed consent was taken from the participants. Information regarding age, parity, duration of married life, contraceptive use and history of abnormal Pap smears was obtained from all the women.
All women recruited for the study underwent a Pap smear twice using an appropriate size metal Cusco’s speculum. In the first visit, the Pap smear was taken using a dry speculum, with no water or gel, as per the usual practice. The second smear was taken 3-4 d later after applying xylocaine jelly over the outer surfaces of the superior and inferior blades of the Cusco’s speculum. The xylocaine jelly contained lignocaine hydrochloride 20 milligram as the active ingredient, hypromellose, methyl hydroxybenzoate, propyl hydroxybenzoate, sodium hydroxide, purified water and hydrochloric acid for pH adjustment.
The smear was taken using an Ayre’s spatula and endocervical brush, spread on a glass slide and fixed in 95% isopropyl alcohol for 10 min. The glass slides from the no gel and the gel group were kept in separate containers to prevent contamination of the slides. After drying, the slides were sent to the cytopathologists who were blinded to the group assignments of the smear. The Pap smears were analyzed and classified according to the revised Bethesda scoring 2001. The smear was considered unsatisfactory if 75% of the epithelial cells were covered by blood, inflammation or artifacts.
After each Pap smear, the women were asked to rate their discomfort on a visual analogue scale (VAS) ranging from 0 (no discomfort) to 10 (most discomfort).
In the present study, each woman served as her own control. The Pap smears were collected by one of the three gynecologists at the level of consultant. It was a double blinded trial as both the patients and the cytopathologists were unaware of the method used in collecting the Pap smear.
Past studies have indicated the incidence of unsatisfactory smears to be 1.5%-4%. So taking the average incidence as 2.5% and the margin of error as 2.5%, the minimum sample size was calculated to be 150. A χ2 test and unpaired t test were used for different statistical calculations.
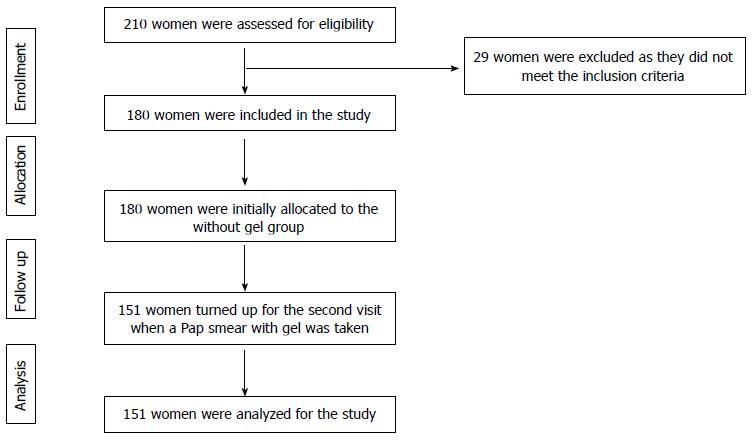
A total of 210 women were enrolled in the present study. The first Pap smear without gel was taken in 180 women who met the inclusion criteria. Out of these 180 women, 29 were lost to follow up. A repeat Pap smear with gel was taken in 151 women who reported for the second visit as per the protocol. Thus, our final sample size was 151. Figure 1 shows the consort flow diagram of the study.
The mean age of women in the study population was 34.6 ± 8.6 years. The mean duration of married life was 12.8 ± 8.1 years and mean parity was 2.0 ± 1.3 (Table 1).
| Age interval (yr) | Frequency |
| < 30 | 63 (41.7) |
| 30-40 | 48 (31.8) |
| 40-50 | 35 (23.2) |
| 50-60 | 5 (3.3) |
| Total | 151 |
There was no significant difference in the percentage of unsatisfactory smears, low grade squamous intraepithelial lesions or high grade squamous intraepithelial lesions in the gel versus no gel group (Table 2). There were no cases of invasive cancer in the study population.
| Cytology results | Without gel | With gel | P value |
| Unsatisfactory | 3 (1.9) | 5 (3.3) | 0.2 |
| NILM | 146 (96.7) | 142 (94.0) | 0.1 |
| Granulomatous cervicitis | 0 (0) | 1 (0.7) | 0.2 |
| LSIL | 0 (0) | 1 (0.7) | 0.2 |
| HSIL | 2 (1.3) | 2 (1.3) | 0.5 |
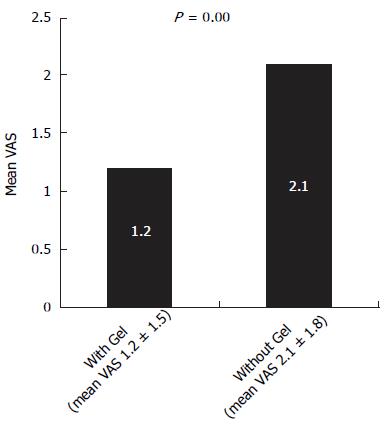
However, a significant difference (P = 0.0) was observed in the visual analogue pain score between the gel group (mean VAS: 1.2 ± 1.5) and no gel group (mean VAS: 2.1 ± 1.8), as shown in Figure 2.
Our study showed that using a small amount of lubricant on the outer side of superior and inferior blades of speculum does not affect the cytology of Pap smears. Thus, speculum lubrication may be performed as a routine practice during Pap smear collection to minimize discomfort to the woman. This is in accordance with earlier studies[4-7] where the same observation was made. In the majority of these studies, subjects were randomized into two groups, while in our study the same woman served as her own control.
A study by Charoenkwan et al[8] found a higher incidence of unsatisfactory smears (12.1% vs 1.7%) in gel contaminated smears. It should be noted that in their study they applied gel directly over the external cervical os in contrast to our study where we applied the gel over the outer aspects of speculum to facilitate the entry of the speculum. Köşüş et al[9] also reported significantly increased rates of unsatisfactory smears in the gel applied group.
The present study also showed that applying gel over the speculum significantly improves the pain score of the women, thus reflecting a reduction in the discomfort associated with undergoing a Pap smear. The majority of studies found in the literature comment on the effect of gel on cervical cytology and only a few studies have evaluated the effect on minimizing the pain for the woman. Gilson et al[7] found no significant alteration in patient discomfort with speculum gel lubrication in their study on 40 patients. In a study by Hill et al[10], lower pain scores were observed in the gel group compared to speculum lubrication with water (P < 0.01).
The strength of our study lies in the fact that we evaluated both the parameters simultaneously, i.e., the effect of gel on cervical cytology and pain scoring. The low overall pain scores observed in both groups could be due to experienced gynecologists performing the test.
However, our study is not without limitations. We repeated the procedure with gel on the same woman and this could have resulted in less anxiety due to preexisting increased awareness of the procedure and lower pain scores. However, this protocol was planned so that all women underwent their first smear without gel as per routine protocol so that the diagnoses was not missed in case gel obscured smear cytology or if the woman did not return for repeat testing. Postmenopausal women and women with infective etiology were intentionally excluded from the study as the discomfort caused by a speculum is more in these women. Women with epithelial cell abnormalities were too few in the study to be able to evaluate whether there is an increase in false negative rates with gel. We would recommend doing the same study on larger subset of population using liquid cytology.
The use of gel for vaginal speculum lubrication in the collection of Pap smears had no adverse effect on cervical cytology results and it significantly decreased the level of discomfort in women undergoing Pap smear screening.
Cervical cancer is still one of the most common cancers in females despite the application of widespread screening. The common reason cited for noncompliance among women for cervical cancer screening is the discomfort associated with speculum insertion.
This study was conducted to evaluate whether lubrication of the vaginal speculum improves the discomfort for women as well as its effect on cervical cytology.
Contrary to the old dictum that no speculum lubrication should be used while taking a Pap smear, a few studies have been conducted in the recent past that show that speculum lubrication improves the discomfort during smear examination. However, the effect of speculum lubrication on cervical cytology is conflicting.
The study shows that speculum lubrication improves the discomfort for women and that it does not affect cervical cytology. However, there is further scope to do a larger study using liquid cytology.
A visual analogue score is an objective means of assessing pain felt by a person who marks the intensity of pain experienced on a scale ranging from 0 to 10.
This article evaluated the effect of vaginal speculum lubrication with xylocaine gel on cervical cytology and pain scoring in Pap smear screening and concluded that vaginal speculum lubrication with xylocaine gel did not influence the Pap smear screening.
P- Reviewer: Celik H, Gardner Mutch D, Wang PH, Yokoyama Y S- Editor: Gou SX L- Editor: Roemmele A E- Editor: Zhang DN
| 1. | Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBaseNo.11[Internet]. Lyon, France: International Agency for Research on Cancer 2013; Available from: http://globocan.iarc.fr, accessed on 2/2/2013. |
| 2. | Hoyo C, Yarnall KS, Skinner CS, Moorman PG, Sellers D, Reid L. Pain predicts non-adherence to pap smear screening among middle-aged African American women. Prev Med. 2005;41:439-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Cunningham FG, Gant NF, Leveno KJ, Gilstrap III LC, Hauth JC, Wenstrom KD. William Obstetrics. 21st ed. New York (NY): McGraw-Hill 2001; 227. |
| 4. | Amies AM, Miller L, Lee SK, Koutsky L. The effect of vaginal speculum lubrication on the rate of unsatisfactory cervical cytology diagnosis. Obstet Gynecol. 2002;100:889-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Harer WB, Valenzuela G, Lebo D. Lubrication of the vaginal introitus and speculum does not affect Papanicolaou smears. Obstet Gynecol. 2002;100:887-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Griffith WF, Stuart GS, Gluck KL, Heartwell SF. Vaginal speculum lubrication and its effects on cervical cytology and microbiology. Contraception. 2005;72:60-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Gilson M, Desai A, Cardoza-Favarato G, Vroman P, Thornton JA. Does gel affect cytology or comfort in the screening papanicolaou smear? J Am Board Fam Med. 2005;19:340-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Charoenkwan K, Ninunanahaeminda K, Khunamornpong S, Srisomboon J, Thorner PS. Effects of gel lubricant on cervical cytology. Acta Cytol. 2008;52:654-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Köşüş A, Köşüş N, Duran M, Haltaş H, Hızlı D, Kafalı H. Effect of liquid-based gel application during speculum examination on satisfactory level of smear examination. Arch Gynecol Obstet. 2012;285:1599-1602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Hill DA, Lamvu G. Effect of lubricating gel on patient comfort during vaginal speculum examination: a randomized controlled trial. Obstet Gynecol. 2012;119:227-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |