Published online May 10, 2014. doi: 10.5317/wjog.v3.i2.85
Revised: February 17, 2014
Accepted: April 11, 2014
Published online: May 10, 2014
Processing time: 175 Days and 2.4 Hours
AIM: To investigate the use of the Gaumard’s Noelle S550.100 Maternal and Neonatal Simulators for teaching forceps delivery.
METHODS: Twenty two (n = 22) resident physicians were enrolled in a simulation course on operative forceps deliveries. The physicians enrolled in the course were all part of an accredited Obstetrics and Gynecology residency program and ranged in their training from post graduate year (PGY) 1-4. Each participant received simulation based teaching on the indications, contraindications, proper application, delivery and removal of forceps by a single teacher. The Gaumard’s simulator and Simpson forceps were used for this course. Statistical analysis using SPSS statistical software was performed after the completion of the simulation training program. A paired student t-test was performed to compare the cohort’s mean pretest and post simulation training scores. Follow up skills assessment scores at one month, 3 mo and 6 mo were compared to the baseline pretest score using a paired student t-test.
RESULTS: There was statistically significant improvement in the post simulation training performance evaluations compared to the pretest, 13.7 (SD = 3.14) vs 7.9 (SD = 4.92), P < 0.05. Scores at 1 mo, 3 mo, and 6 mo were compared to the pretest score and showed retention of skills: 4.6 (SD = 5.5, 95%CI: 2.21-7.07), 4.4 (SD = 5.2, 95%CI: 2.13-6.70), and 5.6 (SD = 4.8, 95%CI: 3.53-7.75) points, respectively. There were statistically significant differences between residents by post graduate training year on pretest scores, however these differences were not present after simulation training. Pretest scores for PGY 1, 2, 3, 4 were 3.5 (SD = 2.27, 95%CI: 2.13-5.00), 7.25 (SD = 6.70, 95%CI: 1.50-13.00), 10.75 (SD = 1.5, 95%CI: 9.50-12.00), 12.17 (SD = 2.57, 95%CI: 10.33-14.00). After simulation training PGY 1 residents did as well as well as the upper level residents. Posttest mean test scores for PGY 1, 2, 3, 4 were 13.75 (SD = 1.49, 95%CI: 12.75-14.63), 10.25 (SD = 0.24, 95%CI: 4.25-14.00), 15.00 (SD = 1.16, 95%CI: 14.00-16.00), 15.17 (SD = 0.75, 95%CI: 14.67-15.67).
CONCLUSION: Our simulation based training program not only produced short term gains, but participants were able to retain the skills learned and demonstrate their knowledge months later.
Core tip: In this article the authors investigated the use of the Gaumard's Noelle S550.100 Maternal and Neonatal Simulators for teaching forceps delivery. They describe the process of developing a simulation program, application, and evaluation at Banner Good Samaritan Medical Center. The intervention was successful in teaching resident physicians the steps of application, delivery and removal in forceps operative delivery. The authors hope is that their method may be applied in development of a variety of simulation based programs to improved education in obstetrics.
- Citation: Doehrman P, Erickson L, Galfione K, Geier B, Kahol K, Ashby A. Simulation training in contemporary obstetrics education. World J Obstet Gynecol 2014; 3(2): 85-89
- URL: https://www.wjgnet.com/2218-6220/full/v3/i2/85.htm
- DOI: https://dx.doi.org/10.5317/wjog.v3.i2.85
As rapid technologic growth expands the skills set of graduating residents in obstetrics and gynecology (ob/gyn) in the areas of minimally invasive surgery, there is a profound loss of basic skills in operative delivery. The current average number forceps deliveries for graduating ob/gyn residents are below what is necessary to be proficient in this invaluable skill. The average ob/gyn resident has performed 6 forceps assisted operative vaginal deliveries, compared to 120 laparoscopic surgeries[1]. As the use of forceps decline, cesarean sections and the associated complications are more prevalent than ever. Cesarean sections account for over one third of deliveries performed each year and outnumber operative vaginal deliveries by three to one. In 2007, cesarean sections were at an all-time high at 32%[2,3]. Cesarean delivery involves major abdominal surgery, and is associated with higher rates of maternal and neonatal complications compared with vaginal birth[4,5]. The rates of cesarean sections vary widely depending on geographic region, and some authors argue this is due to a regional lack of skilled providers in operative vaginal delivery[6].
The residency program at Banner Good Samaritan Medical Center was keenly aware of this trend as their own residents experienced decreasing numbers of real life forceps deliveries. Simulation training was presented as a viable solution to providing graduate medical training in forceps delivery without effecting patient safety.
Other surgical specialties have harnessed the power of simulation to provide residents with a foundation of skills prior to performing procedures on live patients[7]. This is particularly important for emergency situations and high stress surgical scenarios[7,8]. General surgeons have developed simulation courses based on proven techniques for teaching fundamental laparoscopic skills. The strength of these courses is in providing residents experience performing skills in the safety of the simulation lab where failures of efficiency can be overcome without effecting patient care. Furthermore, simulation training provides equality in resident training as it is not dependent on the chance of exposure to surgical emergencies.
The existence of the Simulation Education and Training Center at Banner Good Samaritan Medical Center was a critical factor in the creation of this program. Opened in 2006, this 6000 square foot, two million dollar facility has trained 5000 health care professional. The aim of this program was to evaluate the use of the Gaumard’s Noelle S550.100 Maternal and Neonatal Simulators in the development of a forceps simulation program for training residents in obstetrics and gynecology.
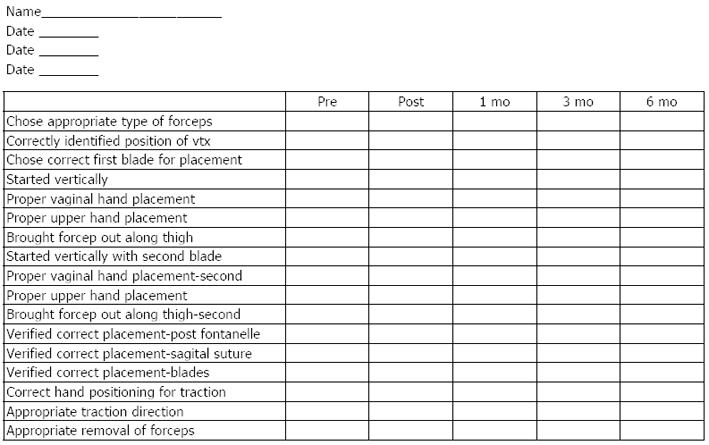
Resident physicians in obstetrics and gynecology from a single center participated in simulation training as part of their education in operative delivery techniques. Their performance before and after training was recorded to evaluate and improve forceps training for resident physicians. Initially, 25 residents chose to participate, with only 3 unable to complete the course. The residents were divided into five groups. Participants were first able to perform a simulated forceps delivery and given a pretest score on their performance based on a specific checklist (Figure 1). Each group then received simulation based teaching on the indications, contraindications, proper application, delivery and removal of forceps by a single teacher. A posttest was then administered using the same assessment checklist to evaluate their forceps delivery skills. Video recordings of the 22 residents were obtained at their 1 mo, 3 mo, and 6 mo follow up assessments.
Sixteen steps were identified as critical aspects for forceps application and delivery based on Dennen’s Forceps Deliveries, 3rd Ed[9]. The steps were reviewed by six independent board certified physicians in obstetrics and gynecology from the Department of Obstetrics and Gynecology at Banner Good Samaritan Medical Center. The steps were rated in terms of importance and weighted averages calculated to gauge if any steps should be excluded from the assessment or tutorial.
The same checklist was used for each of the evaluations. A blinded scorer was used to grade each anonymous video recording. The physician scoring each video was unaware of the resident’s identity, as well as their year of post graduate training to limit bias. Residents were gowned and gloved in the video to hide their identity. A second evaluator reviewed all of the follow up videos to establish reliability of the score assessment tool. Both evaluators were board certified in obstetrics and gynecology for over 10 years and routinely performed forceps deliveries at a large tertiary care center. Both evaluators had performed over 100 forceps deliveries and had experience evaluating resident performance in operative deliveries for over 10 years.
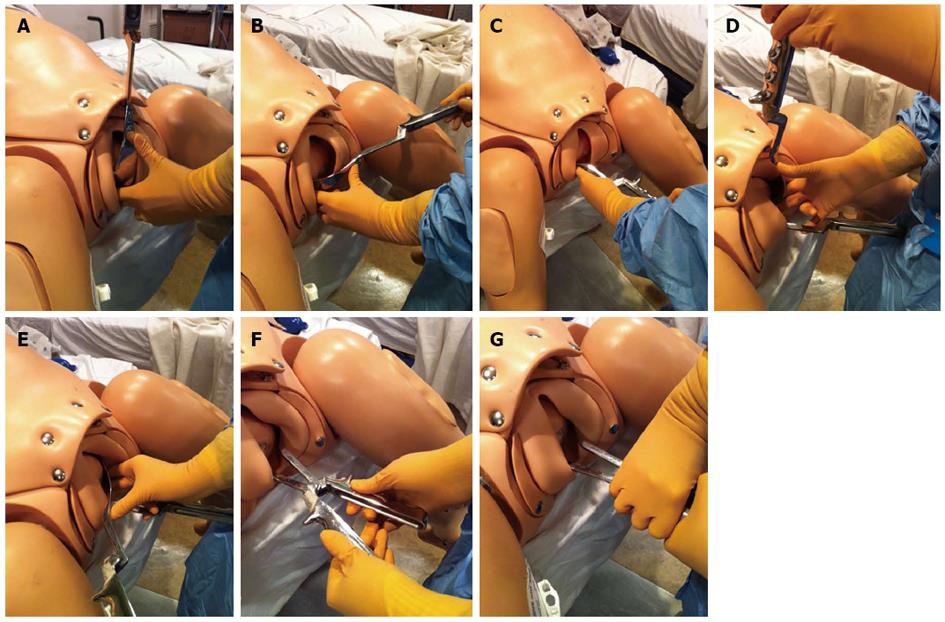
The decision was made to teach the following steps for placement of the first blade: identifying fetal position, orientation of the forceps, choice of first blade, application of the first blade in the vertical position, use of the vaginal hand to guide placement of the first blade, advancement of the blade into the horizontal position along the opposite thigh.
Steps for placing the second blade included: starting in the vertical position, placement of vaginal hand to guide blade, and advancing blade from vertical to horizontal along the opposite thigh.
Additional steps included, checking the placement of the forceps on the neonatal head by feeling for the posterior fontanel and sagittal suture. Finally, steps for delivery included correct hand position for traction and appropriate removal.
Examples of the steps in forceps application and desired hand positions are illustrated in Figure 2.
Statistical analysis using SPSS statistical software was performed after the completion of the simulation training program. A paired student t-test was performed to compare the cohort’s mean pretest and post simulation scores. Follow up skills assessment scores at 1 mo, 3 mo and 6 mo were compared to the baseline pretest score using a paired student t-test.
Inter-rater reliability was investigated by calculating the Pearson correlation coefficient. This provided evidence on the reliability of the testing instrument itself. Pearson correlation between evaluator one and two was 0.7 (P < 0.001).
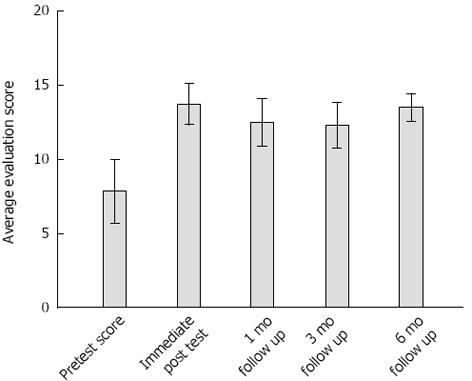
The pretests were compared to posttest scores for the 22 participants who complete the simulation curriculum. There was statistically significant improvement in the post simulation training performance evaluations compared to the pretest, 13.7 (SD = 3.14) vs 7.9 (SD = 4.92), P < 0.05. Scores at one month, three months, and six months were compared to the pretest score and showed retention of skills (Figure 3). The difference between pretest and follow up scores at one month, three month and six month were: 4.6 (SD = 5.5, 95%CI: 2.21-7.07), 4.4 (SD = 5.2, 95%CI: 2.13-6.70), and 5.6 (SD = 4.8, 95%CI: 3.53-7.75) points, respectively (Table 1).
| Paired differences | t | df | Sig. (2-tailed) | |||||
| Mean | SD | SEM | 95%CI of the difference | |||||
| Lower | Upper | |||||||
| Pretest-immediate posttest | -5.864 | 4.357 | 0.929 | -7.795 | -3.932 | -6.313 | 21 | 0.000 |
| Pretest-one month follow up | -4.636 | 5.482 | 1.169 | -7.067 | -2.206 | -3.967 | 21 | 0.001 |
| Pretest-post 3 mo | -4.409 | 5.152 | 1.098 | -6.693 | -2.125 | -4.014 | 21 | 0.001 |
| Pretest-post 6 mo | -5.636 | 4.756 | 1.014 | -7.745 | -3.527 | -5.558 | 21 | 0.000 |
There were statistically significant differences between residents by post graduate training year on pretest scores, however these differences were not present after simulation training. Pretest scores for PGY 1, 2, 3, 4 were 3.5 (SD = 2.27, 95%CI: 2.13-5.00), 7.25 (SD = 6.70, 95%CI: 1.50-13.00), 10.75 (SD = 1.5, 95%CI: 9.50-12.00), 12.17 (SD = 2.57, 95%CI: 10.33-14.00). PGY 1 residents as a group scored lower compared with PGY 2, 3, and 4. After simulation training PGY 1 residents did as well as well as the upper level residents. Posttest mean test scores for PGY 1, 2, 3, 4 were 13.75 (SD = 1.49, 95%CI: 12.75-14.63), 10.25 (SD = 0.24, 95%CI: 4.25-14.00), 15.00 (SD = 1.16, 95%CI: 14.00-16.00), 15.17 (SD = 0.75, 95%CI: 14.67-15.67).
Increased year of resident training had a statistically significant association with higher pretest skills assessment scores, (Pearson correlation = 0.637, P = 0.001). However, after simulation training there was no difference in skills assessment scores among resident based on year of training with forceps delivery.
Simulation training offers a solution to the problem of declining resident exposure to forceps operative deliveries nationally. Our simulation based training program not only produced short term gains, but residents were able to retain the skills learned and demonstrate their knowledge months later. Analysis of pretest scores showed an association between forceps skills and year of training, with improved scores with increased year of post graduate year. However, after simulation training this association no longer exists. Considering, clinical experience with forceps generally increases by year of training, our study suggests that these differences in real life experience may be overcome by simulation training. Simulation training has the potential for providing the necessary experience resident physicians need in adjunct with real life experience to produce qualified obstetricians with the necessary skills to perform operative deliveries independently.
The Gaumard’s Noelle S550.100 Maternal and Neonatal Simulators was limited in its ability to replicate a forceps delivery. The anatomy of a real fetal skull, specifically the contours if the maxillary bone, provide the points of articulation for the forceps instrument. The Noelle S550.100 Neonatal Simulator did not have the same cranial bone structure and thus the forceps frequently slipped or became misplaced during the delivery. Therefore, the trainees in this study were only expected to apply the forceps correctly and demonstrate the correct plane of traction. The residents were not expected to complete the delivery due to the limitations of the simulator. The maternal simulator in contrast had very realistic anatomy; fetal station could correctly be identified by palpation of the ischial spines just as in a live patient.
Another limitation of this program is the lack of data collected on the effect of simulation training on resident performance in real life settings. An opportunity for further program evaluation includes follow up surveys to assess if simulation training increased resident confidence and likeliness to perform forceps deliveries when in practice. Twenty percent of the residents who took part in this program are now in practice and their feedback on whether or not they routinely perform forceps deliveries would provide important follow up data to support continued simulation education.
Additionally, research opportunities to further investigate the effect of simulation training on resident performance in real life settings would include a prospective study with assessment of real life operative delivery skills assessments before and after simulation training.
The current average number forceps deliveries for graduating ob/gyn residents are below what is necessary to be proficient in this invaluable skill. Cesarean sections account for over one third of deliveries performed each year. Cesarean delivery involves major abdominal surgery, and is associated with higher rates of maternal and neonatal complications compared with vaginal birth. The rates of cesarean sections vary widely depending on geographic region, and some authors argue this is due to a regional lack of skilled providers in operative vaginal delivery. Simulation training is a viable solution to providing graduate medical training in forceps delivery without effecting patient safety.
There are increasing demands on the health care system to adhere to the highest standards of safety and cost efficiency. Additionally, new changes to the Accreditation Council for Graduate Medical Education restrictions on resident work hours creates further challenges to garnering the necessary skills in operative delivery. The power of simulation has been harnessed by varies surgical specialties to provide residents with a foundation of skills prior to performing procedures on live patients.
Simulation training is particularly important for emergency situations and high stress surgical scenarios. General surgeons have developed simulation courses based on proven techniques for teaching fundamental laparoscopic skills. The strength of these courses is in providing residents experience performing skills in the safety of the simulation lab where failures of efficiency can be overcome without effecting patient care. Furthermore, simulation training provides equality in resident training as it is not dependent on the chance of exposure to surgical emergencies.
This study suggests that simulation training may provide the needed training in forceps deliveries that are required for residents in obstetrics and gynecology to be proficient in these skills.
Forceps are tools used to assist in the second stage of labor for a variety of indications, such as: arrest of descent, prolonged second stage, maternal exhaustion, pr concerning fetal heart tracings. The second stage of labor is defined as the periods of labor after complete cervical dilation during which time the fetus passes through the pelvis, but prior to expulsion.
This is a well-designed observational study in which resident physicians participated in a simulation course on operative forceps deliveries, before and after assessment were performed. The findings demonstrate the potential utility of simulation training to provide experience and technical skills that are not readily available in real life settings. These methods may be beneficial for teaching a variety of obstetrical skills that may in the future improve the health of mothers and children.
P- Reviewers: da Rosa MI, Marjan K, Zeev B S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
| 1. | Accreditation Council for Graduate Medical Education. Obstetrics and Gynecology Case Logs National Data Report. Department of Applications and Data Analysis. 2010;. |
| 2. | American College of Obstetricians and Gynecologists. Operative vaginal delivery. ACOG Practice Bulletin number 17, Washington, DC: American College of Obstetricians and Gynecologists 2000; . |
| 3. | Hamilton BE, Martin JA, Ventura SJ. Births: Prelimimary data for 2007. National vital statistics reports. Hyattsville, MD: National Center for Health Statistics 2009; 12. |
| 4. | Yang Q, Wen SW, Oppenheimer L, Chen XK, Black D, Gao J, Walker MC. Association of caesarean delivery for first birth with placenta praevia and placental abruption in second pregnancy. BJOG. 2007;114:609-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Liston FA, Allen VM, O’Connell CM, Jangaard KA. Neonatal outcomes with caesarean delivery at term. Arch Dis Child Fetal Neonatal Ed. 2008;93:F176-F182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Sinha P, Langford K. Forceps delivery in 21st century obstetrics. J Gynecol Obstet. 2009;11:2. |
| 7. | Brindley PG, Jones DB, Grantcharov T, de Gara C. Canadian Association of University Surgeons’ Annual Symposium. Surgical simulation: the solution to safe training or a promise unfulfilled? Can J Surg. 2012;55:S200-S206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Maschuw K, Schlosser K, Kupietz E, Slater EP, Weyers P, Hassan I. Do soft skills predict surgical performance?: a single-center randomized controlled trial evaluating predictors of skill acquisition in virtual reality laparoscopy. World J Surg. 2011;35:480-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Hale RW, Dennen EH. Dennen’s Forceps Deliveries. Washington: American College of Obstetricians and Gynecologists 2001; Available from: http://vufind.carli.illinois.edu/vf-uic/Record/uic_1600186. |