Published online May 11, 2023. doi: 10.5317/wjog.v12.i3.28
Peer-review started: January 27, 2023
First decision: March 28, 2023
Revised: April 10, 2023
Accepted: April 24, 2023
Article in press: April 24, 2023
Published online: May 11, 2023
Processing time: 104 Days and 3.6 Hours
Vaginal stones are rare with current literature limited to case reports. Vaginal stones are classified as primary or secondary stones. Primary stones form in the vagina when there is urinary stasis. Secondary stones form in the presence of a vaginal foreign body that acts as a nidus for the deposition of urinary salts. Foreign bodies, such as surgical mesh, make vaginal stone formation more likely, particularly in patients with urinary incontinence and conditions that predispose them to urinary calculi formation.
A 71-year-old female with a history of sacrocolpopexy, hyperaldosteronism, and urgency urinary incontinence presented with vaginal stone accumulation overlying two areas of vaginal sacrocolpopexy mesh exposure. The vaginal stones were initially removed to permit examination, but the stones reaccumulated at the site of the exposed mesh, later requiring definitive surgical management.
Patients with vaginal mesh exposure and conditions that predispose them to kidney stones are not ideal candidates for expectant management of mesh exposure, particularly if they have coexisting urinary incontinence. These individuals should be counseled about possible vaginal stone accumulation, and surgical management should be considered.
Core Tip: Patients with vaginal mesh exposure that have underlying conditions that predispose them to urinary calculi formation may be at increased risk of vaginal stone accumulation at the site of mesh exposure. Expectant management of the mesh exposure likely allows vaginal stones to accumulate as urine is persistently in contact with the foreign body. Definitive surgical management in the form of complete excision of the entire area of exposed mesh should be recommended to patients to avoid vaginal stone accumulation.
- Citation: Leong KA, Husk KE. Stone accumulation overlying vaginal mesh exposure: A case report. World J Obstet Gynecol 2023; 12(3): 28-32
- URL: https://www.wjgnet.com/2218-6220/full/v12/i3/28.htm
- DOI: https://dx.doi.org/10.5317/wjog.v12.i3.28
Vaginal foreign bodies, such as surgical mesh, are risk factors for the formation of secondary vaginal stones. When urine has prolonged contact with an exposed foreign body, secondary vaginal stones can form due to crystallization of stagnant urine. Urinary incontinence is therefore thought to contribute to vaginal stone formation[1]. We propose that individuals with exposed vaginal mesh and underlying medical conditions that place them at increased risk of kidney stones are prone to forming secondary vaginal stones. Following the CARE Checklist (2016) and with signed patient consent, we present the unique case of a patient with hyperaldosteronism and urgency urinary incontinence who had vaginal stone formation and later reaccumulation at the site of sacrocolpopexy mesh exposure.
A 71-year-old G4P4004 Caucasian female with known vaginal sacrocolpopexy mesh exposure that she previously opted to expectantly manage presented to urogynecology clinic with complaints of overactive bladder and urgency urinary incontinence.
The patient’s symptoms of overactive bladder and urgency urinary incontinence had been worsening for about four years. Her urinary incontinence was nearly constant with dribbling throughout the day. Previous trials of oxybutynin, mirabegron, and solfenacin were ineffective.
In 2014, the patient underwent robotic-assisted supracervical hysterectomy, bilateral salpingo-oophrectomy, mesh sacrocolpopexy, posterior colporrhaphy, perineorrhaphy, retropubic midurethral sling insertion, and cystoscopy. One year after surgery, two areas of mesh exposure were identified at the anterior and posterior apices involving the sacrocolpopexy mesh. The patient was asymptomatic and opted to pursue expectant management. The patient was lost to follow-up until 2019 when she represented with the above chief complaint.
Relevant personal history includes hyperaldosteronism, overactive bladder, urgency urinary incontinence, and tobacco use.
There was stone formation overlying the sacrocolpopexy mesh exposure sites at the anterior and posterior vaginal apices adjacent to the cervix. Given the degree of apical support maintained, office examination was difficult. Evaluation in the operating room was recommended.
In 2020, the patient underwent examination under anesthesia, cystourethroscopy, and vaginoscopy. On vaginoscopy, a midline anterior mesh exposure measuring approximately 3 cm (vertical) × 2 cm (transverse) × 3 mm (height) was identified with a 4 cm × 3 cm stone intermixed with the mesh fibers. A midline posterior mesh exposure measuring approximately 2.5 cm (vertical) × 0.5 cm (transverse) × 0.5 cm (height) was also identified with a 4 cm × 2 cm stone intermixed within the mesh fibers. Cystourethroscopy did not demonstrate any evidence of mesh exposure in the bladder or urethra, and vesicovaginal and urethrovaginal fistulae were specifically excluded. The majority of the calcifications were removed intraoperatively, which permitted improved visualization of the exposed mesh sites.
Vaginal stone analysis was performed. The composition was noted to be 70% hydroxyapatite (calcium phosphate), 25% magnesium ammonium phosphate, and 5% ammonium acid urate.
None.
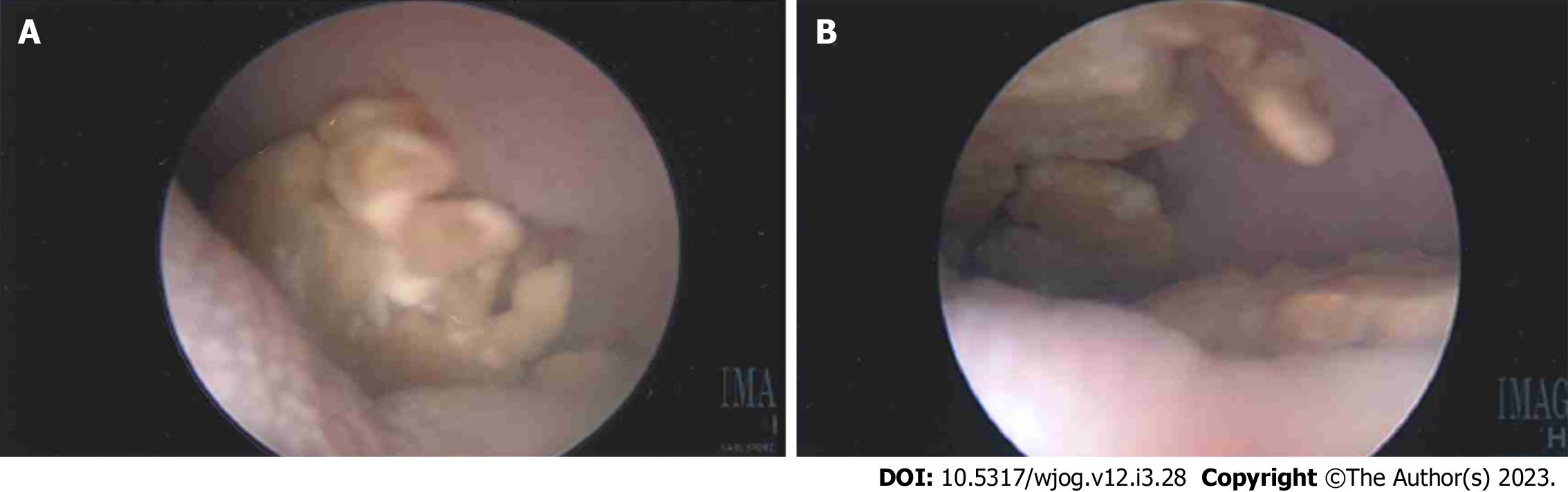
Following intraoperative evaluation, definitive surgical management with excision of the mesh exposure sites was planned. However, while awaiting surgery, the patient was in a motor vehicle accident requiring prolonged recovery. Additionally, factors related to coronavirus disease 2019 cases caused an approximately one-year delay in reevaluation. During this time, the vaginal stones reaccumulated at the exposed mesh sites. In 2021, mesh excision via a vaginal approach was performed. There was a 3 cm × 2 cm stone found anteriorly and a 2.5 cm × 0.5 cm stone found posteriorly. The stones were completely intermixed with the mesh strands (Figure 1). The patient was diagnosed with reaccumulation of vaginal stones at the site of exposed sacrocolpopexy mesh.
The patient underwent excision of the entirety of the exposed mesh areas, concomitant removal of the stone material, and unremarkable cystourethroscopy. The stone analysis revealed a 100% hydroxyapatite composition.
The patient had no perioperative complications and did well postoperatively. On six-week follow-up examination, there was no evidence of continued mesh exposure or reaccumluation of vaginal stone material. The patient began intravesical onabotulinum toxin A injections for management of urgency urinary incontinence.
Sacrocolpopexy is a reconstructive surgical procedure that is performed to correct apical prolapse. A synthetic mesh is used to support the vagina, with or without the cervix, by affixing it to the anterior longitudinal ligament overlying the sacrum. The prevalence of mesh exposure following sacrocolpopexy is estimated to be as high as 10.5%[2]. While patients with mesh exposure may be asymp
In general, data on vaginal stone formation are limited to case reports, and vaginal stones are therefore considered a rare phenomenon. Vaginal stones can be broadly categorized into primary or secondary stones. Primary stones typically result from urinary stasis within the vagina allowing for deposition of urinary salts. Some causes of primary stones include vaginal outlet obstruction, neurogenic bladder dysfunction, prolonged recumbent positioning such as in bedridden or paralyzed patients, and vesicovaginal, urethrovaginal, or ureterovaginal fistulae[4-7]. Secondary stones form in the vagina in the presence of a foreign body, such as contraceptive devices or exposed vaginal mesh, which acts as a nidus for urinary crystallization and subsequent stone formation[1].
Although limited data exist detailing the composition of vaginal stones, review of the current literature suggests that both primary and secondary vaginal stones are most commonly composed of struvite[1,4,5,8]. The proposed mechanism for struvite stone formation is that stasis of urine infected with urease-producing bacteria, such as Klebsiella, Proteus mirabilis, and Escherichia coli, causes the normally acidic environment of the vagina to become alkaline, which facilitates formation of struvite stones[9]. The first stone analysis for our patient revealed a predominantly hydroxyapatite composition (with a small struvite percentage), and the second stone analysis revealed 100% hydroxyapatite composition, which is a clear contrast to previously published cases of struvite vaginal stones. It is important to note that the composition of our patient’s vaginal stones is more typical of kidney stones. The most common composition of kidney stones is calcium oxalate with a frequency of 67%, followed by hydroxyapatite stones with a frequency of 16%. Struvite kidney stones are relatively uncommon with a frequency of 3%[10].
The predominantly hydroxyapatite composition of our patient’s vaginal stones is unusual since most published cases of vaginal stones report a struvite composition. Hydroxyapatite is more common for kidney stones. Our patient has no history of nephrolithiasis; but she does have hyperaldosteronism. We propose that this patient’s history of hyperaldosteronism is responsible for the atypical composition of the secondary vaginal stones. Hyperaldosteronism causes hypercalciuria, phosphaturia, and hypocitraturia. These urinary changes are risk factors associated with kidney stone formation and recurrence[11]. In our patient’s case, these urinary changes secondary to hyperaldosteronism likely contributed to the atypical composition of her vaginal stones, which more closely resemble that of the most common types of kidney stones rather than the typical struvite composition of vaginal stones. Therefore, it is prudent for clinicians to be aware of medical conditions that increase the risk of kidney stones because patients with such conditions may be at increased risk for forming vaginal stones.
In addition to the unusual hydroaxyapatite composition of this patient’s vaginal stones, this patient’s rapid reaccumulation of stone material overlying the mesh exposure after the initial stone removal is unique to this case. The reaccumulation suggests that patients with vaginal mesh exposure who are at increased risk of kidney stones may not be optimal candidates for expectant management, even if they have asymptomatic mesh exposure. This is particularly pertinent for individuals with risk factors for persistent contact of the mesh exposure to urine, such as significant urinary incontinence as with our patient. In addition, the short-interval reaccumulation of stones in this patient favors recommending excision of exposed mesh rather than temporizing measures, such as removal of the stone material only. Leaving exposed mesh is likely to result in reaccumulation of the vaginal stones.
Our patient’s case highlights an example of vaginal stone formation overlying a vaginal mesh exposure in the setting of a medical condition that increases the risk of kidney stones. The stone analyses from this case suggest that individuals with underlying conditions that predispose them to kidney stones may be at increased risk of forming secondary vaginal stones with compositions that more closely resemble kidney stones rather than vaginal stones. This patient’s case was also compounded by severe urgency urinary incontinence, which resulted in significant exposure of the mesh foreign body to urine. Individuals with a vaginal nidus, such as exposed mesh, that is in persistent contact with urine may be at higher risk of stone reaccumulation without definitive management. This case illustrates the importance of clinician awareness of conditions that increase the risk of kidney stones, as well as individualized patient counseling about the risk of developing stones overlying a mesh exposure. These patients are not optimal candidates for expectant management, and definitive surgical management with excision of the entire area of mesh exposure should be recommended.
Patients with vaginal mesh exposure and underlying conditions that predispose them to urinary calculi formation may not be ideal candidates for expectant management, especially if they have coexisting urinary incontinence. These individuals should be counseled about the possibility of stone accumulation, and surgical management should be considered. This unusual case adds to the current limited literature on vaginal stones. This case additionally helps to guide counseling of patients with vaginal mesh exposure that have concomitant risk factors for kidney stones and persistent contact of exposed mesh with urine.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aydin S, Turkey; Gupta SK, India S-Editor: Wang JJ L-Editor: A P-Editor: Zhang XD
| 1. | Griffiths KM, Towers GD, Yaklic JL. Vaginal Urinary Calculi Formation Secondary to Vaginal Mesh Exposure with Urinary Incontinence. Case Rep Obstet Gynecol. 2017;2017:8710315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, Fine P, Menefee S, Ridgeway B, Visco A, Warren LK, Zhang M, Meikle S. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309:2016-2024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 395] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 3. | Crosby EC, Abernethy M, Berger MB, DeLancey JO, Fenner DE, Morgan DM. Symptom resolution after operative management of complications from transvaginal mesh. Obstet Gynecol. 2014;123:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (2)] |
| 4. | Jo JY, Lee SM, Shin JK, Choi WJ, Cho IA. Huge vaginal stone: Case report and review of the literature. Front Surg. 2022;9:937371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Aronson SL, Hovius MC, Janszen EWM. Large primary vaginal stone in a woman with multiple sclerosis. BMJ Case Rep. 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Avsar AF, Keskin HL, Catma T, Kaya B, Sivaslioglu AA. A large primary vaginal calculus in a woman with paraplegia. J Low Genit Tract Dis. 2013;17:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Wei D, Xie Y, Niu X. Vaginal stones caused by urethrovaginal fistula: A case report. Medicine (Baltimore). 2019;98:e18003. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Raghavaiah NV, Devi AI. Primary vaginal stones. J Urol. 1980;123:771-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Malhotra N, Kumar S, Roy KK, Agarwal R, Verma V. Vaginal calculus secondary to vaginal outlet obstruction. J Clin Ultrasound. 2004;32:204-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Levy FL, Adams-Huet B, Pak CY. Ambulatory evaluation of nephrolithiasis: an update of a 1980 protocol. Am J Med. 1995;98:50-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 218] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Lieske JC, Rule AD, Krambeck AE, Williams JC, Bergstralh EJ, Mehta RA, Moyer TP. Stone composition as a function of age and sex. Clin J Am Soc Nephrol. 2014;9:2141-2146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 194] [Article Influence: 17.6] [Reference Citation Analysis (0)] |