Published online Jun 29, 2022. doi: 10.5317/wjog.v11.i3.20
Peer-review started: January 17, 2022
First decision: March 16, 2022
Revised: March 30, 2022
Accepted: June 3, 2022
Article in press: June 3, 2022
Published online: June 29, 2022
Processing time: 162 Days and 11 Hours
One of the main difficulties faced in the prevention of the vertical transmission of syphilis is the inadequate treatment of pregnant women and their partners. The disease causes serious repercussions in infected newborns.
To evaluate the prevalence and factors associated with the therapeutic adhesion among partners of pregnant women with syphilis in a county in Northeastern Brazil.
This is a descriptive, analytic, quantitative, cross-sectional study that was carried out through interviews with 46 pregnant women diagnosed with syphilis between 2017 and 2018 as well as with their partners. The interviews aimed at collecting data regarding sociodemographic characteristics, obstetric variables and information about syphilis, and partners’ related variables.
Our results showed that 73.91% of the partners did not undergo appropriate treatments, and obtaining negative results in syphilis tests was the main reason for the absence of therapies. The following factors were significantly associated with the lack of treatment among partners: Being a partner that is not the current mate of the pregnant woman, having a level of schooling inferior to 8 years [odds ratio (OR) = 10.28], and the pregnant woman undergoing up to two syphilis tests during the prenatal care (OR = 8.6). The study found a higher odds of absent treatment among partners if the pregnant woman is not white (OR = 13.88) or if the partner has less than 8 years of schooling (OR = 21.00) or has a monthly income of less than half the minimum wage (OR = 13.93).
The findings of this study show a high prevalence of partners that are not adequately treated for syphilis, a phenomenon that is strongly associated with socioeconomic factors.
Core Tip: Treating infected pregnant women and their partners is a challenging step in the prevention of syphilis vertical transmission. This study evaluated the prevalence and factors associated with the therapeutic adhesion among partners of pregnant women with syphilis in a county of northeastern Brazil. Here we demonstrated an important lack of treatment among the study partners, which was associated with various socioeconomic factors.
- Citation: Fernandes LPMR, Oliveira CNT, de Brito BB, Freire de Melo F, Souza CL, Oliveira MV. Prevalence and factors associated with non-adherence to therapy among partners of pregnant women with syphilis in a city of northeastern Brazil. World J Obstet Gynecol 2022; 11(3): 20-32
- URL: https://www.wjgnet.com/2218-6220/full/v11/i3/20.htm
- DOI: https://dx.doi.org/10.5317/wjog.v11.i3.20
Syphilis is a systemic infectious disease with chronic evolution, having the Treponema pallidum as a causative agent. The disease can be transmitted through multiple routes, and the contagion mostly occurs through sexual contact and vertical transmission, from the mother to the fetus[1]. Although it is considered an easily diagnosed and treated disease, syphilis is still an important health issue worldwide[2,3]. The “acquired syphilis” is the form of the disease that can affect the sexually active adult population. When pregnant women are infected, the disease is classified as “syphilis in pregnancy” and, if not treated or inadequately treated, the infection is transmitted to the fetus, after the 16th week of pregnancy, leading to “congenital syphilis” (CS)[2,4,5]. Symptoms related to CS include early syphilis snuffles due to nasal ulceration, vesicular eruption, skeletal abnormalities, and hepatosplenomegaly[6].
The World Health Organization estimates that syphilis affects one million pregnant women each year around the world, leading to more than 300 thousand fetal and neonatal deaths, besides increasing the risk of premature death in more than 200 thousand children. In addition, it is considered a reemerging disease with a growing incidence even in developed countries[7,8]. Among the main difficulties faced in the prevention of the vertical transmission of syphilis, the inadequate treatment of pregnant women and their partners stands out. Even after appropriate treatment during prenatal care, pregnant women often experience reinfections by their partners, which can lead to the transmission of the disease to their children[9,10].
Therefore, the men's health is a crucial factor to be taken into account when considering the prevention of CS; however, sociocultural factors and institutional barriers seem to impair the achievement of satisfactory rates of adhesion to healthcare measures targeting the male population. Throughout the last few years, the number of non-treated partners has overcome the number of treated partners in Brazil[10-14]. From 2012 to 2017, 62% of the partners of pregnant women with syphilis were not treated in this country[15].
The impacts caused by syphilis go far beyond the health aspects. Important financial losses to the health economy have been associated with that disease. The expenditures demanded by a CS-affected newborn (NB) are three-fold higher than those required for the healthcare of NBs without syphilis, besides the permanent costs to individuals with neurological damage who require specialized and continuous attention from the health systems[16]. In 2018, the Brazilian Unified Health System spent approximately 2.8 million dollars on hospital procedures directly related to syphilis[17].
Given the scenario of growing cases of acquired syphilis, syphilis in pregnancy, and CS, and considering the existence of difficulties in the implementation of healthcare measures for male populations, this study aimed to describe the prevalence of syphilis among pregnant women in the city of Itapetinga in northeastern Brazil, as well as to identify factors associated with the therapeutic adhesion of partners whose women tested positive for the disease during pregnancy.
This descriptive, analytic, quantitative, cross-sectional study was carried out with pregnant women diagnosed with syphilis between 2017 and 2018 as well as with their partners. The data collection occurred between January and June 2019.
The initial projection of the study was to analyze 56 couples (pregnant women with syphilis/partners) based on the mean number of syphilis cases that occur in the study city according to the Brazilian System of Information for Notifiable Diseases (SINAN). However, the notification of cases overcame the aforementioned mean in 2018, reaching 69 cases and showing an increase in the occurrence of syphilis in pregnant women in the study city.
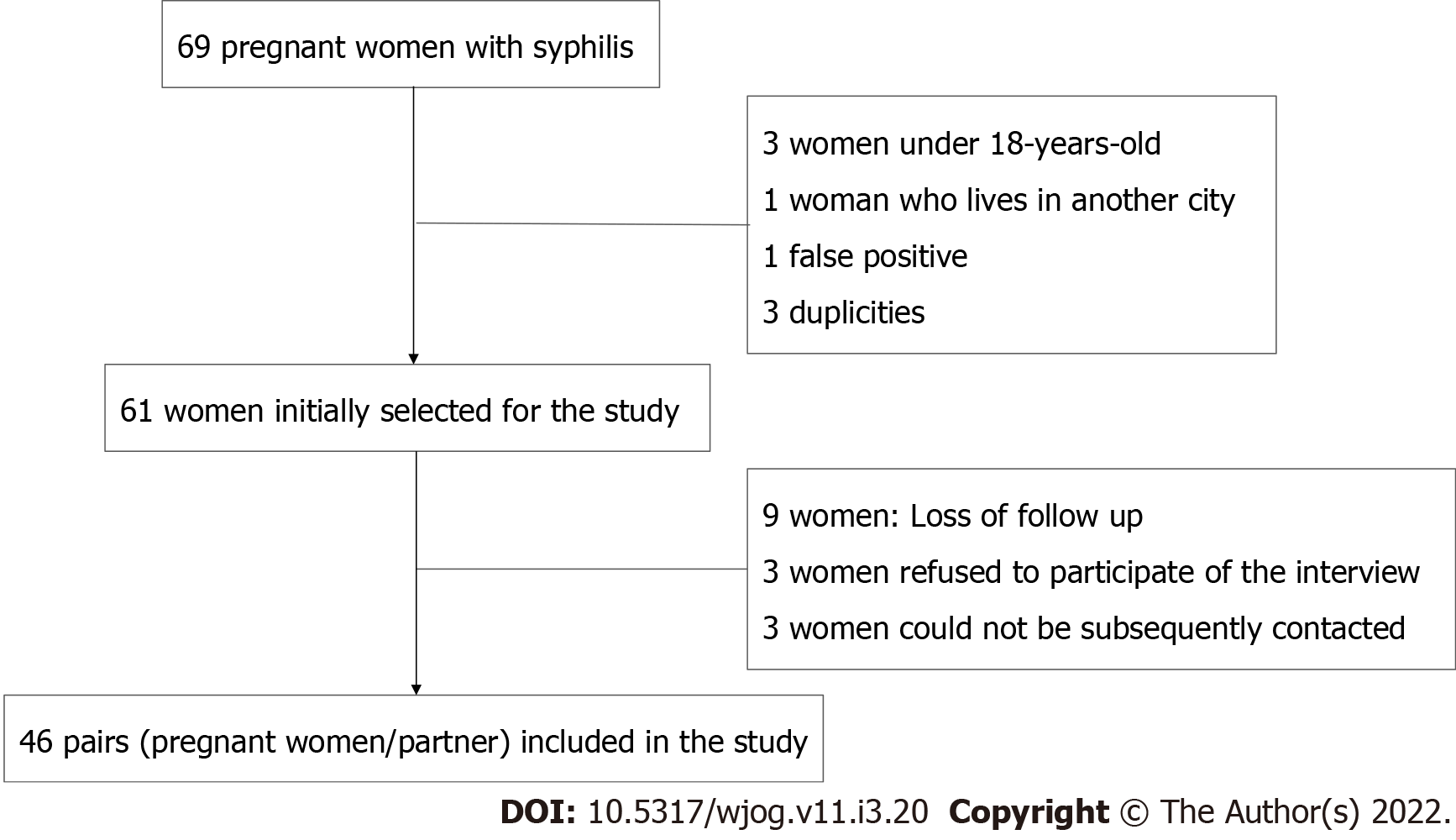
Cases of syphilis in pregnancy were defined as pregnant women who had at least one positive syphilis test, in accordance with the classification of the Brazilian Ministry of Health. Three pregnant women under 18 years old, one who lives in another city, one with a negative confirmatory test (false positive), and three duplicities in SINAN were excluded from the study. Loss to follow-up occurred with nine pregnant women who moved to another city, three who refused to participate in the interview, and three who could not be subsequently contacted. Finally, 46 pairs (pregnant women/ partners) were included in the study (Figure 1).
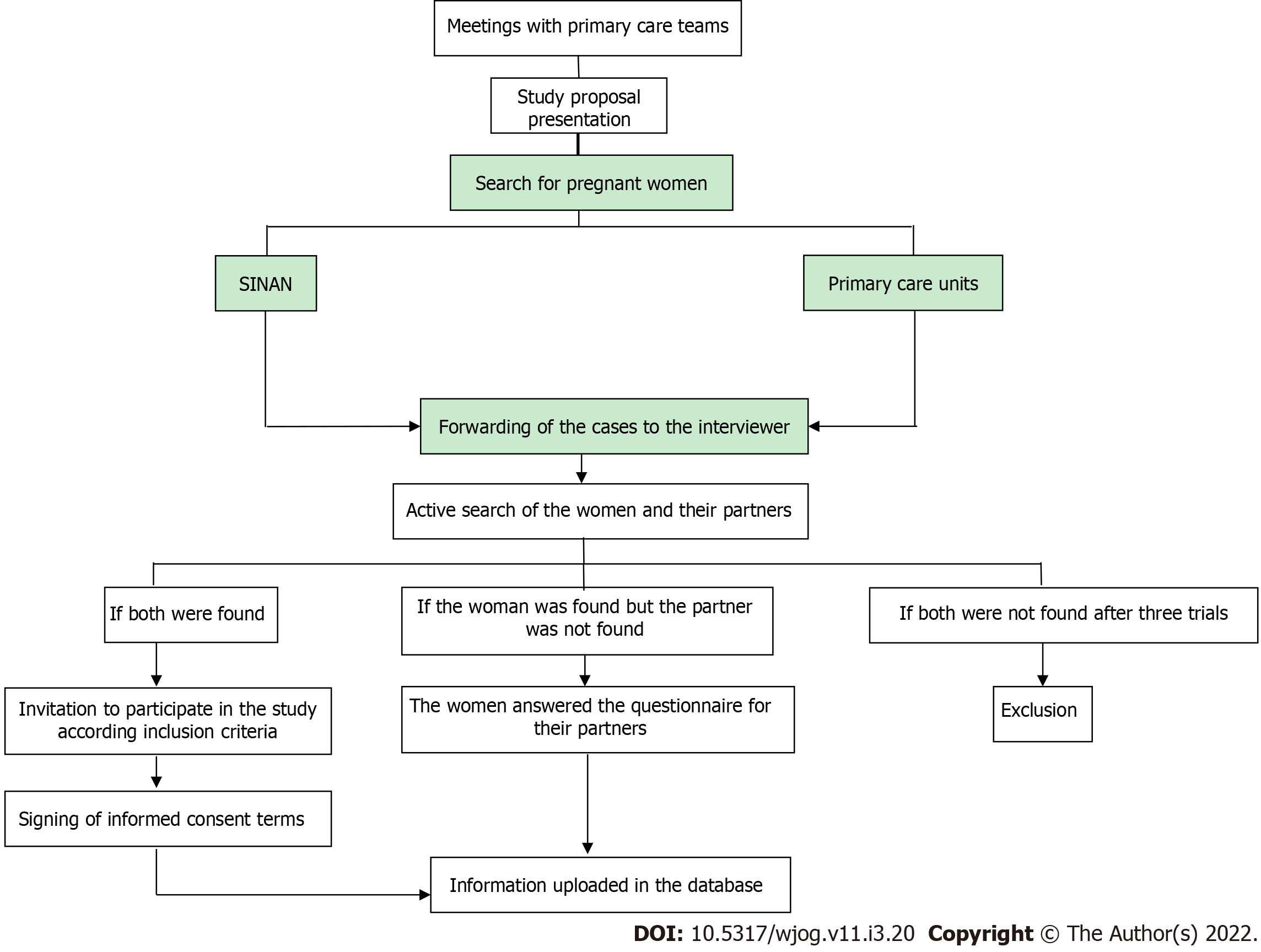
In order to contact the patients, epidemiological surveillance professionals and contributors of this study performed an active search. Informed consent was obtained from the pregnant women who accepted to participate in the study and, then, the interviews were conducted in their homes. If their partners lived in the same residence, they were immediately invited to participate in the study as well and, if they accepted, signed informed consent was also obtained. Otherwise, partners who did not live with the correspondent pregnant women were searched according to the addresses informed by the pregnant women. Finally, if the partners could not be contacted, the pregnant women provided the partners’ information required in the study. The steps of data collection are described in Figure 2.
The data collection tool was adapted from the questionnaire used in the Born in Brazil Program (2003) and National Health Survey (2017), epidemiological surveillance research performed by Brazilian governmental health agencies. The questionnaire was organized into four sections (A, B, C, and D). Sections A (sociodemographic characteristics) and B (obstetric variables and information about syphilis) were conducted with pregnant women, whereas C (partner’s identification variables) and D (variables regarding treatment and complementary information) were used to obtain information from partners. In order to adapt the questionnaire language, a pilot study was performed with pregnant women without a syphilis diagnosis. In this stage, a number of participants corresponding to 20% of the study sample were included and the data collection occurred in a single moment, in an individual and presential way, with pregnant women who were waiting for their prenatal consultation in a basic health unit in the study city. The questionnaire showed to be suitable, and it was well accepted by the participants in this pilot study.
The information regarding the number of prenatal consultations, results of syphilis tests, and drugs used in pregnancy, as well as their doses, were collected from the Brazilian pregnant women card or from the medical records from primary care units.
A database was elaborated in Microsoft Office Excel and analyzed through the EPI-INFO statistical pack (version 7.1.5.2). The Pearson’s chi-square test was performed with a 5% significance level and 95% confidence interval to compare frequencies. The association measures were done through the odds ratio (OR) calculation in the univariate analysis. Subsequently, a multivariate analysis using the Statistical Package for the Social Sciences (SPSS, Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp. IBM Corp.) was performed through logistic regression with all the variables for which a P-value was inferior to 0.20 was obtained in the univariate analysis. For the final model, the variables with P < 0.05 were taken into consideration in the block with the best adjustment through the Homer-Lemeshow method.
The study was put into practice after the approval by the Research Ethics Committee of the Multidisciplinary Institute of Health of the Federal University of Bahia, under protocol number 2.995.408 and the certificate of presentation of ethical appreciation number 97664818.3.0000.5556.
Tables 1 and 2 show the descriptive analysis performed on the pregnant women included in the study and their partners. With regard to the pregnant women's socioeconomic profile, 63% (n = 29) were aged between 18 and 24 years, and most of them did not have mates, were not white, and had less than 8 years of schooling, and a monthly income higher than half the minimum wage. Regarding obstetric antecedents, half of the women did not use any contraceptive method, 30% have had at least one spontaneous abortion, and most of them had their prenatal care started up to the third month of gestation, attending to more than six consultations before the delivery.
| Variable | n | % |
| Pregnant women | ||
| Age (yr) | ||
| 25 or older | 17 | 36.96 |
| 18 to 24 | 29 | 63.04 |
| Marital status | ||
| With a mate | 21 | 45.65 |
| Without a mate | 25 | 54.35 |
| Ethnicity | ||
| White | 10 | 21.74 |
| Not white | 36 | 78.26 |
| Schooling level | ||
| 8 yr or more | 20 | 43.48 |
| Less than 8 yr | 26 | 56.52 |
| Monthly income | ||
| Higher than half a MW | 30 | 65.22 |
| Less than half a MW | 16 | 34.78 |
| Contraceptive use | ||
| No | 23 | 50.00 |
| Yes | 23 | 50.00 |
| Number of syphilis tests | ||
| Up to 2 tests | 16 | 34.78 |
| 3 or more tests | 30 | 65.22 |
| Beginning of the prenatal care | ||
| Until the 3rd month of gestation | 32 | 71.11 |
| After the 3rd month of gestation | 13 | 28.26 |
| Number of prenatal consultations | ||
| At least 6 consultations | 27 | 58.70 |
| Less than 6 consultations | 19 | 41.30 |
| Variable | n | % |
| Partners | ||
| Age (yr) | ||
| 18 to 24 | 21 | 45.65 |
| 25 or older | 25 | 54.35 |
| Ethnicity | ||
| White | 14 | 30.43 |
| Not White | 32 | 69.57 |
| Schooling level | ||
| 8 yr or more | 16 | 37.21 |
| Less than 8 yr | 27 | 62.79 |
| Monthly income | ||
| More than half a MW | 26 | 56.52 |
| Up to half a MW | 20 | 43.48 |
| Occupation | ||
| Commerce, industry, or freelance | 34 | 73.91 |
| Not working | 12 | 26.09 |
| Formal work | ||
| Yes | 15 | 32.61 |
| No | 31 | 67.39 |
| Last attendance to a medical consultation | ||
| Less than 1 yr ago | 18 | 41.86 |
| More than 1 yr ago | 25 | 58.14 |
| Health status | ||
| Regular | 13 | 28.26 |
| Good/Very good | 33 | 71.74 |
| Appropriate treatment | ||
| Yes | 12 | 26.09 |
| No | 34 | 73.91 |
| Reasons for absent treatment | ||
| Negative syphilis tests | 13 | 38.23 |
| The partner was communicated but refused treatment or did not attend the primary care unit | 09 | 26.47 |
| The partner was not communicated | 06 | 17.65 |
| Others | 06 | 17.65 |
Concerning the syphilis-related variables, most individuals were diagnosed by a nurse, had no previous information about syphilis, and received information about the disease from the health professionals. Moreover, 80% of the participants had Venereal Disease Research Laboratory (VDRL) test titers higher than 1:4, and no information about the titers observed in the second VDRL test was found for 48% of the pregnant women. In 99% of the pregnant women, benzathine penicillin was the drug of choice for the treatment of syphilis, and 56.5% of the doses were administered in a hospital or in an emergency care unit.
In this study, ten pregnant women (22%) had syphilis in previous pregnancies and most women (percentage) have already undergone at least one previous treatment for the disease, which suggests the occurrence of reinfections. A pregnant woman was diagnosed with syphilis only during the delivery and five NBs had congenital syphilis, from which one died due to this condition.
With respect to the partners, most of them were 25 years or older, were not white, had less than 8 years of schooling and a monthly income higher than half the minimum wage, and had no formal work. In addition, 26% of them were unemployed. Regarding their health condition, most partners qualified their health status as good, did not attend a medical consultation in the last year, and consumed alcoholic beverages more than once a month. Complementarily, 23% of them reported the use of other drugs. Among the illicit drugs mentioned, marijuana was the most prevalent (82%), followed by cocaine (8%).
Appropriate treatment was not performed in 73.91% (n = 34) of the partners. Among the individuals who did not undergo treatment, 38.23% (n = 13) were informed that the therapy would not be necessary since they had negative syphilis tests. On the other hand, 26.47% (n = 9) of them told that they were communicated about the need for treatment, but refused to go to the health unit. Moreover, 23.52% (n = 8) told that they were not informed about the need for treatment or did not have further contact with the women. Some untreated individuals told that they did not have available time for the therapy, were afraid of injections, or had a work schedule incompatible with the health unit opening time.
The univariate analysis evidenced that the absence of treatment among partners was significantly associated with some women-related factors, namely, not having a current mate (OR = 5.50), having less than 8 years of schooling (OR = 6.27), and undergoing up to two syphilis tests during pregnancy (OR = 8.6). The analysis with partner-related variables showed that not treating for syphilis was associated with having less than 8 years of schooling (OR = 10.28) and a monthly income of up to half the minimum wage (OR = 13.93).
Multivariate analysis (Table 3) of pregnant women-related variables showed that identifying themselves with an ethnicity other than white is an important characteristic for the occurrence of non-treated partners (OR = 13.88). Among partners, such analysis revealed that having less than 8 years of schooling (OR = 21.00) and a monthly income lower than half the minimum wage (OR = 12.23) were correlated with the absence of syphilis treatment.
| Variable | OR (95%CI) | P value |
| Pregnant women | ||
| Ethnicity other than white | 13.88 (1.38-14.1) | 0.02 |
| Partners | ||
| Less than 8 yr of schooling | 21.00 (2.70-177.47) | 0.00 |
| Monthly income of less than a half MW | 12.23 (1.39-107.44) | 0.02 |
Some studies show a high prevalence of non-treated partners of pregnant women with syphilis in multiple regions of Brazil[9,14,15]. However, studies on syphilis in pregnancy including direct interviews with partners are rare, since most published data on this issue only contain information provided by pregnant women. Of note, the importance of the concomitant treatment of pregnant women and partners is well established in the scientific field and recommended by governmental agencies, which is the most suitable approach in order to reduce the risk of recontamination as well as the prevalence of the disease and the occurrence of CS[18-21].
The characteristics of pregnant women observed in this study corroborate the findings of other Brazilian studies showing a higher prevalence of the disease among women between 18 and 24 years old, which represents a higher rate of infection among young women of reproductive age, mainly teenagers[22-24]. This study showed that when pregnant women do not have a current mate, the odds of the absence of treatment among partners is higher than if the pregnant woman is married, corroborating the findings by Lafetá and colleagues[25]. According to Figueiredo et al[26], the type of relationship of a couple (a stable relationship or not) should be carefully taken into consideration by health professionals since it will determine the most suitable strategy to reach a higher therapeutic adherence among partners.
In this study, most pregnant women and partners had less than 8 years of schooling. In addition, partners with that level of schooling had a 21-fold higher odds of not being treated than individuals with more years of schooling. The association between the occurrence of syphilis and low educational level was described by previous studies as well[23,27,28]. Of note, the schooling level is often used as an indicator of the socio-economic conditions of a population, since low-educated people who have a limited understanding of the importance of healthcare and preventive measures are considered more vulnerable individuals[28].
The odds of lacking treatment among partners was 13.88-fold higher if the pregnant women and partners identified themselves with an ethnicity other than white. According to the Brazilian Institute of Geography and Statistics, 64.35% of the population of the study city is not white, which matches the ethnical profile of the patients included in this study[29]. A study including 110 pregnant women from another Brazilian city observed that being a white woman was significantly associated with carrying out the appropriate treatment for syphilis in partners[10]. Complementarily, other reports show a higher prevalence of syphilis in pregnancy and CS among women who identify themselves with a race other than white[7,20,22].
It has to be emphasized that there was a high proportion of pregnant women who reported previous spontaneous abortions in this study (30.4%), and a possible relationship between this data and the presence of syphilis. According to the Brazillian Ministry of Health, 40% of the pregnancies in women with non-treated syphilis results in spontaneous abortion[21,30]. Another Brazilian study identified a rate of 18% of abortions and high syphilis rates among pregnant women, suggesting that the infection may be a factor associated with that outcome. Although the present study was not designed to verify this association, these data attract attention and should be further investigated in future studies.
The data regarding the beginning of prenatal care and the number of consultations observed in this study corroborate previous investigations in which a higher prevalence of partners’ treatment was associated with starting prenatal care before the third month of pregnancy and attending to at least six consultations before delivery[12,30]. These results reinforce the need for a higher adhesion to prenatal care. However, the assurance of access to prenatal care and diagnostic tests alone is not enough to ensure a meaningful improvement in health assistance since strategical and educative actions to qualify professionals for the management of syphilis as well as well-organized health services aiming to control that disease may be lacking[13,15,31].
Moreover, there was a significant association in the univariate analysis between performing not more than two syphilis tests in pregnant women and the lack of treatment among partners, which corroborates the study by Silva and colleagues[32]. The authors identified that women who underwent less than five diagnostic tests during prenatal care experienced a higher number of failures in the syphilis-related diagnosis and treatment, and it was supposed to be due to the low access to consultations and diagnostic tests as well as to the lack of knowledge about the outcomes associated with the disease. In addition, the necessity for constant monitoring of syphilis cases by health professionals including the performance of diagnostic tests has to be considered in order to reduce the occurrence of failures in the prevention of the disease[13].
Nurses diagnosed most of the pregnant women in this study and 89% of the patients reported that they received explanations about the disease. Nonetheless, 73.91% of the partners were not adequately treated. However, Campos and colleagues verified an increase in the partners’ therapeutic adhesion when information about syphilis was provided to pregnant women after the diagnosis, highlighting the importance of the quality of the counseling[9]. Our study points towards the necessity of evaluating the quality of the explanations provided by the health professionals to patients as well as the frailties of the health service when calling up the partners to undergo the treatment[13]. Therefore, it is important to promote a permanent education of the professionals involved in prenatal care, which may allow the magnification of the capturing and reception of sexual partners of pregnant women in order to perform an appropriate treatment and to improve the quality of the prenatal assistance[15,27].
With regard to the environment in which the benzathine penicillin was administered, more than half of the pregnant women and partners were referred to a hospital or an emergency care unit, probably because of the fear of potential penicillin-related side effects by health professionals from the primary care units in which these patients were accompanied. However, the reference of pregnant women and partners to tertiary care units may be followed by a delay in attendance, impossibility to confirm if the patient underwent the treatment, and loss of continuity of the patients’ care in primary care units[26]. Health agencies have highlighted the importance of administering penicillin in the primary care units, mainly in pregnant women and partners, due to the risk of vertical transmission. Moreover, the prevalence of allergic reactions among patients treated with penicillin ranges from 0.01% and 0.05%[33]. Finally, it has to be emphasized that the need to move to hospitals or emergency care units may influence the therapy adhesion of the partners since their transport depends on financial sources, which can be unavailable.
Of note, most partners of pregnant women diagnosed with syphilis were 25 years or older, and the rate of absent treatment was higher in the group of individuals aged 18 to 24 years. However, no statistical significance was observed with that association, which was probably due to the small sample (Tables 4 and 5). Previous studies point toward a higher syphilis prevalence among partners aged 21 to 30 years[9] and a higher odds to undergo treatment among those aged between 20 and 29 years[10].
| Variable | OR (95%CI) | χ2 | P value |
| Pregnant Women | |||
| Age (yr) | |||
| 25 or older | 1 | ||
| 18 to 24 | 3.36 (0.85-13.14) | 3.18 | 0.07 |
| Marital status | |||
| With a mate | 1 | ||
| Without a mate | 5.50 (1.24-24.25) | 5.63 | 0.02 |
| Ethnicity | |||
| White | 1 | ||
| Not white | 4.14 (0.9-18.36) | 3.78 | 0.06 |
| Schooling level | |||
| 8 yr or more | 1 | ||
| Less than 8 yr | 6.27 (1.41-27.86) | 6.56 | 0.01 |
| Monthly income | |||
| More than half a MW | 1 | ||
| Up to half a MW | 3.50 (0.66-18.49) | 2.34 | 0.11 |
| Contraceptive use | |||
| No | 1 | ||
| Yes | 1.57 (0.41-5.95) | 0.45 | 0.36 |
| Spontaneous abortion | |||
| No | 1 | ||
| Yes | 2.72 ( 0.51-14.53) | 1.45 | 0.20 |
| Beginning of the prenatal care | |||
| Until the 3rd month of gestation | 1 | ||
| After the 3rd month of gestation | 1.30 ( 0.29-5.86) | 0.12 | 0.52 |
| Number of prenatal consultations | |||
| At least 6 consultations | 1 | ||
| Less than 6 consultations | 1.77 ( 0.45-6.91) | 0.69 | 0.31 |
| Number of syphilis tests | |||
| At least 3 tests | 1 | ||
| Up to 2 tests | 8.68 (1.00-75.01) | 5.00 | 0.02 |
| Variable | OR (95%CI) | χ2 | P value |
| Partners | |||
| Age (yr) | |||
| 25 or older | 1 | ||
| 18 to 24 | 2.00 (0.50-7.91) | 0.99 | 0.25 |
| Ethnicity | |||
| White | 1 | ||
| Not white | 1.20 (0.29-4.9) | 0.06 | 0.53 |
| Schooling | |||
| 8 or more years | 1 | ||
| Less than 8 years | 10.28 (2.17-48.67) | 10.17 | 0.00a |
| Monthly income | |||
| More than half a MW | 1 | ||
| Up to half a MW | 13.93(1.61-120.35) | 8.16 | 0.00a |
| Occupation | |||
| Commerce, industry, or freelance | 1 | ||
| Not working | 5.26 (0.60-46.05) | 2.65 | 0.10 |
| Formal work | |||
| Yes | 1 | ||
| No | 2.77 (0.71-10.86) | 2.23 | 0.12 |
| Last attendance to a medical consultation | |||
| Less than 1 yr ago | 1 | ||
| More than 1 yr ago | 2.54 ( 0.65-9.94) | 1.85 | 0.15 |
| Health status | |||
| Regular | 1 | ||
| Good/Very good | 1.38 (0.33-5.75) | 0.20 | 0.45 |
In both univariate and multivariate analyzes, statistically significant associations were verified between the lack of syphilis treatment for the partner and a monthly income of less than half the minimum wage. This data corroborates other studies that attribute the absence of syphilis treatment for pregnant women and partners to unfavorable socioeconomic factors[10,28,34]. Although it does not occur only in people from lower social classes, syphilis is often associated with low income, a variable that hinders the appropriate diagnosis and treatment of diseases since it is considered an important predictor of limited access to health services[16]. Complementarily, 67% of the partners did not have formal work, another data that highlights the vulnerabilities of the population studied.
With respect to the consumption of alcoholic beverages, 54% of the partners told that they drink more than once a month and 23% reported the use of other illicit drugs, with marijuana being the most prevalent, followed by cocaine. No statistically significant association was observed between the use of drugs and the lack of treatment of the partners. However, it has to be emphasized that such associations have been verified by previous studies[9,10,16].
Among the partners of this study, 71.7% considered themselves as having a “good” or “very good” health status, and most of them did not attend a medical consultation in the last year. Levorato et al[35] observed that men who say that they have no disease have a 2.89-fold higher odds of not seeking health services for preventive care. In the present study, that association was not verified probably due to the limited statistical power of the sample.
The image of the man built through history is an omnipotent identity that does not get sick, and male individuals tend not to take health care seriously. In that context, women seek health services 1.9 times more than men[36]. Associated with that, if health policies do not include special strategies targeting men's health, such a population is not attracted to health services[9]. The carelessness of healthcare services regarding men's health becomes evident with the high number of partners that do not undergo syphilis treatment and with the lack of inclusion of partners in prenatal care, which should be a priority in aiming for an effective cure for pregnant women and reduction of the incidence of syphilis[36].
In this study, 73.91% of the partners were not adequately treated, and similar results were reported in other papers[12,18,32,37]. The lack of treatment among partners has been considered the main fault in the treatment of pregnant women. Worryingly, the rate observed here is higher than the prevalence observed in Brazil in 2018 (53%)[21].
The main reasons for the absence of treatment were getting negative results in syphilis tests (38.23%) and refusal of the call-up by the primary care units (26.47%). A similar result was observed in the study by Hildebrand et al[10]. Of note, the treatment of partners of pregnant women with syphilis with a dose of benzathine penicillin (2.4 million international units) is recommended even if the serological results are negative[38].
Performing an active search to contact patients was a limiting factor of this research. Sometimes, it was necessary to do more than one visit to a single residence, mainly to find the partners. Among 46 women, 22 (47.8%) responded with the information about the partners, which resulted in the ignoring of some information and in a possible information bias. Among the reasons for the women who respond to their partners are: Some pregnant women did not allow the study contributors to interview their partners, other women did not live with their partners anymore, some partners refused to provide informed consent, some potential participants moved to another city, five women did not communicate their partners about the syphilis diagnosis, and one partner was arrested due to drug traffic.
The analyses performed here have never been evaluated in the study region before. The results obtained by this study provided a view on an important aspect of fighting syphilis-the treatment of sexual partners-and contribute to the knowledge about the theme. This study also reveals important information that may potentially aid in the improvement of the strategies of therapeutic follow-up for the disease and stimulate the conduction of studies with a bigger sample on this theme, since the low availability of financial sources limited the extension of the study region.
Factors associated with the treatment of the partners of pregnant women with syphilis represent a challenge to be overcome by the public health agencies. This study faced various difficulties given the nature of the investigation, and the important obstacles found when working in such a vulnerable social context. The research allowed the identification of factors related to the treatment of partners of pregnant women with syphilis, which was associated with socioeconomic variables and prenatal assistance, evidencing frailties in care practices that hinder the interruption of the disease’s transmission chain. The findings highlight the need for greater attention from health managers and other professionals to populations with unfavorable socioeconomic conditions, low schooling level, low income, single women, and women who underwent not more than two syphilis tests during prenatal care. In that context, it is necessary for the inclusion of partners in prenatal assistance as well as investments in educative and strategic actions for the qualification of health professionals for the management of syphilis. Finally, further studies are needed for a better understanding of the factors associated with the inappropriate management of syphilis.
It is not new that syphilis is a major health concern worldwide. The disease can be transmitted through multiple routes, and the contagion mostly occurs through sexual contact and vertical transmission, from the mother to the fetus. Although it is considered an easily diagnosed and treated disease, syphilis is still an important health issue worldwide.
Worryingly, the congenital form of the Treponema pallidum infection is still a big concern, mainly in underdeveloped countries, although it is an avoidable condition. The prevention is mainly based on the proper diagnosis of the disease during pregnancy and the subsequent treatment of the pregnant women and their partners. In this sense, the adherence of partners to the treatment has to be highlighted as a key step in the prevention of such a devastating disease.
To evaluate the prevalence and factors associated with the therapeutic adhesion among partners of pregnant women with syphilis in a county of northeastern Brazil.
This is a descriptive, analytic, quantitative, cross-sectional study that was carried out through interviews with 46 pregnant women diagnosed with syphilis between 2017 and 2018 as well as with their partners. The interviews aimed at collecting data regarding sociodemographic characteristics, obstetric variables and information about syphilis, and partners’ related variables.
Our results showed that 73.91% of the partners did not undergo appropriate treatments, and obtaining negative results in syphilis tests was the main reason for the absence of therapies. The following factors were significantly associated with the lack of treatment among partners: Being a partner that is not the current mate of the pregnant woman, having a level of schooling inferior to 8 years (odds ratio [OR] = 10.28), and the pregnant woman undergoing up to two syphilis tests during the prenatal care (OR = 8.6). The study found a higher odds of absent treatment among partners if the pregnant woman is not white (OR = 13.88) or if the partner has less than 8 years of schooling (OR = 21.00) or has a monthly income of less than half the minimum wage (OR = 13.93).
The findings of this study show a high prevalence of partners that are not adequately treated for syphilis, a phenomenon that is strongly associated with socioeconomic factors.
We expect that this study may aid public health managers in the identification of factors associated with the non-adhesion to syphilis treatment by pregnant women's partners, which can help in the elaboration of effective health campaigns aiming at reducing the prevalence of the disease. Moreover, further research should be performed in order to better understand the persistence of congenital syphilis, mainly in underdeveloped countries.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Al-Ani RM, Iraq; Plagens-Rotman K, Poland A-Editor: Zhu JQ, United States S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Milanez H, Amaral E. Why are we still unable to control the problem of syphilis in pregnant women and their newborns? Rev Bras Ginecol Obstet. 2008;30:325-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | World Health Organization. World Elimination of Congenital Syphilis: Logical Statement and strategy for action. [cited 20 January 2022]. Available from: http://apps.who.int/iris/bitstream/10665/43782/4/9789248595851_por.pdf. |
| 3. | Campos AL, Araújo MA, Melo SP, Gonçalves ML. Epidemiology of gestational syphilis in Fortaleza, Ceará State, Brazil: an uncontrolled disease. Cad Saude Publica. 2010;26:1747-1755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Souza BSO, Rodrigues RM, Gomes RML. Análise epidemiológica de casos notificados de sífilis. Revista da sociedade brasileira de clínica médica. 2018;22:94-98. [DOI] [Full Text] |
| 5. | Plagens-Rotman K, Jarząbek-Bielecka G, Merks P, Kêdzia W, Czarnecka-Operacz M. Syphilis: then and now. Postepy Dermatol Alergol. 2021;38:550-554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. |
Plagens-Rotman K, Przybylska R, Gerke K, et al Syphilis and a pregnant woman: a real danger for the woman and the child.
|
| 7. | Dias APSL, Wanzeller RCM, Vital RSS, Silveira APS. A sífilis no atual cenário brasileiro : Uma análise de literatura. Scientific Journal. 2018;1:1-21. [DOI] [Full Text] |
| 8. | Brazil. Ministry of Health. Secretaria de vigilância a saúde. Boletim epidemiológico-Sífilis. 2017;48:44. |
| 9. | Campos AL, Araújo MA, Melo SP, Andrade RF, Gonçalves ML. [Syphilis in parturients: aspects related to the sex partner]. Rev Bras Ginecol Obstet. 2012;34:397-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Hildebrand VLPC. Sífilis congênita: Fatores associados ao tratamento de parceiros. Dissertação apresentada com vistas a obtenção do título de Mestre modalidade profissional em saúde pública. Rio de Janeiro. 2010;1:85. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Secretaria de Estado da Saúde Coordenadoria de Controle de Doenças. CCD/SES-SP Centro de Referência e Treinamento DST/Aids-Programa Estadual de DST/Aids-CRT/DST/Aids-SP/CCD/SES-SP Área Técnica de Saúde da Criança-CRS/SES-SP Sociedade de Pediatria de São Paulo-SPSP Sociedade Brasileira de Infectologia-SBI. Nota Técnica Conjunta Nº 001/2016/SPSP/SBI/ATSM/ATSC/CRT-PE-DST/AIDS/SES-SP-São Paulo, 2016. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Toldo MKS, Menegazzo LS, Souto AS. A recrudescência da sífilis congênita. Arquivo Catarinense Medicina. 2018;47:2-10. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Souza MHT, Beck EQ. Compreendendo a sífilis congênita a partir do olhar materno. Revista Enfermagem da UFSM. 2019;9:1-13. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Delaunay M, Cadranel J, Lusque A, Meyer N, Gounant V, Moro-Sibilot D, Michot JM, Raimbourg J, Girard N, Guisier F, Planchard D, Metivier AC, Tomasini P, Dansin E, Pérol M, Campana M, Gautschi O, Früh M, Fumet JD, Audigier-Valette C, Couraud S, Dalle S, Leccia MT, Jaffro M, Collot S, Prévot G, Milia J, Mazieres J. Immune-checkpoint inhibitors associated with interstitial lung disease in cancer patients. Eur Respir J. 2017;50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 282] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 15. | Holztrattner JS, Linch GFC, Paz PAA, Gouveia HG, Coelho DF. Sífilis congênita: realização do pré-natal e tratamento da gestante e de seu parceiro. Cogitare enfermagem. , 2019. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Magalhães DM, Kawaguchi IA, Dias A, Calderon Ide M. Maternal and congenital syphilis: a persistent challenge. Cad Saude Publica. 2013;29:1109-1120. [PubMed] |
| 17. | Brazil. Ministry of Health. DATASUS. [cited 20 January 2022]. Available from: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cn. |
| 18. |
Araújo SR, Farias AL, Alcântara DS, Marroni SN, Buges NM, Magalhães CCCRGN, et al Mother's experience against congenital syphilis occurrence in their children.
|
| 19. | Bassani F, Smaniotto M, Wink DR. Sífilis congênita. Anuário Pesquisa e Extensão Unoesc Videira. Santa Catarina, 2017. [DOI] [Full Text] |
| 20. | Godoi LN, Gomes LM, Rocha HMS. Epidemiologia da sífilis gestacional e congênita no estado de Goiás no período de 2013 a 2018. Revista Brasileira Mil Ciências. 2019;5:8. [DOI] [Full Text] |
| 21. | Brazil. Ministry of Health. Secretaria de Vigilância em Saúde. Departamento de doenças de condição crônica e Infecções Sexualmente Transmissíveis. Protocolo clínico e diretrizes terapêuticas para atenção integral às pessoas com infecções sexualmente transmissiveis (IST). Brasilia-DF, 2019: 248. |
| 22. | Silva MJN, Barreto FR, Costa MCN, Carvalho MSI, Teixeira MG. Distribuição da sífilis congênita no estado do Tocantins, 2007-2015. Epidemiol Serv Saude. 2020;29:e2018477. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Santos RRE, Cunha BO, Silva CVC, Silva EB, Parente FS, Campos RALS, et al Análise da ocorrência da sífilis gestacional no estado do Pará em dez anos. Atena editor, 2020: 12. [DOI] [Full Text] |
| 24. | Morais MB, Costa EG, Dutra, Silva JS. Análise dos casos de sífilis congênita no município de Manhuaçu/MG. Pensar Acadêmico. 2019;17:50-59. [DOI] [Full Text] |
| 25. | Lafetá KRG, Martelli Júnior H, Silveira MF, Paranaíba LMR. Maternal and congenital syphilis, underreported and difficult to control Sífilis. Rev Bras Epidemiol. 2016;19:63-74. [RCA] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 26. | Figueiredo MSN, Cavalcante EGR, Oliveira CJ, Monteiro MDFV, Quirino GDS, Oliveira DR. Perception of nurses on the adhesion of partners of pregnant women with syphilis to the treatment. Revista da Rede Enfermagem do Nordeste. 2015;16:345-354. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Favero MLDC, Ribas KAW, Costa MCD, Bonafé SM. Sífilis congênita e gestacional : notificação e assistência pré-natal. Arch Heal Sci. 2019;26:2-8. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Felix ICG, Oliveira TF, Souza CDF, Machado MF. Análise de tendência da sífilis congênita no estado da Bahia de 2008 a 2017. Revista Ciência e Saúde, 2020. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Brazil. Brazilian Institute of Geography and Statistics. [cited 20 January 2022]. Available from: https://cidades.ibge.gov.br/brasil/ba/itapetinga/panorama.acesso em 24 de julho de 2020. 2010. |
| 30. | Araújo EC, Monte PCB, Haber ANCA. Evaluation of prenatal care for syphilis and HIV detection in pregnant women attended in a rural area of Pará State, Brazil. Revista Pan-Amazônica Saúde. 2018;9:33-39. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Saab, F. Prevalência de sífilis em gestantes que abortaram atendidas pelo programa de proteção à gestante-PPG do estado de Sergipe, de 2005 à 2007-Dissertação de Mestrado apresentada ao Programa de Pós-Graduação em Ciências da Saúde da Faculdade de Ciências da Saúde. Brasilia-DF, 2009. [DOI] [Full Text] |
| 32. | Silva DAM, Bois F, Duro E. Factores associados con falla en el diagnostico y tratamiento de sifilis materna. Medicina Infantil. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 33. | Brazilian Federal Council of Nursery. Nota Técnica-N° 03-2017. Brasilia-DF, 2017: 4. [DOI] [Full Text] |
| 34. | Cardoso ARP, Araújo MAL, Cavalcante MS, Frota MA, Melo SP. Análise dos casos de sífilis gestacional e congênita nos anos de 2008 a 2010 em Fortaleza-Ceará, Brasil. Ciência e Saúde Coletiva. 2018;23:563-574. [RCA] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 35. | Levorato CD, de Mello LM, da Silva AS, Nunes AA. Factors associated with the demand for health services from a gender-relational perspective. Cien Saude Colet. 2014;19:1263-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 36. | Siepierski SF, Rosa CCN, Nascimento BA. Incidência de sífilis em gestantes atendidas nas unidades de saúde no município de Teixeira de Freitas, Bahia. Revista Mosaicum. 2018;180-196. [DOI] [Full Text] |
| 37. | Heringer ALDS, Kawa H, Fonseca SC, Brignol SMS, Zarpellon LA, Reis AC. [Inequalities in congenital syphilis trends in the city of Niterói, Brazil, 2007-2016Desigualdades en la tendencia de sífilis congénita en la ciudad de Niterói, Brasil, 2007-2016]. Rev Panam Salud Publica. 2020;44:e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 38. | Brazil. Ministry of Health. Secretaria de vigilância em Saúde. Departamento de Vigilância epidemiológica. Nota Informativa No 2-sei/2017-DIAHV/SVS/MS. Brasília-DF, 2017. |