Peer-review started: September 10, 2022
First decision: October 24, 2022
Revised: October 25, 2022
Accepted: October 31, 2022
Article in press: October 31, 2022
Published online: November 15, 2022
Processing time: 64 Days and 12.7 Hours
Clarithromycin is a macrolide antibiotic commonly prescribed to patients with upper respiratory and otolaryngological infections. Neuropsychiatric adverse effects of clarithromycin include agitation, insomnia, delirium, psychosis, and seizure.
A 52-year-old man was admitted to our hospital with a convulsion. He had > 10-year history of clarithromycin intake for chronic sinusitis. One week before admission, he started to take diltiazem for angina pectoris. On admission, his convulsion subsided. His electroencephalography showed frontal intermittent rhythmic delta activity. One week after he ceased clarithromycin, his electroencephalographic abnormalities disappeared. We suggested that the patient developed convulsions due to increased blood levels of clarithromycin caused by oral administration of diltiazem, which is involved in CYP3A metabolism.
Clarithromycin has a relatively high safety profile and is a frequently prescribed drug. However, there are a few previous reports of clarithromycin-related convulsive disorders. Clinicians should be aware of the drug interaction and rare side effects of seizures.
Core Tip: Clarithromycin is a frequently used medication and has a long history of use. The rarity of reports of convulsions induced by clarithromycin suggests that the induction of convulsions by clarithromycin is a rare phenomenon or has been overlooked. Clarithromycin is a frequently prescribed drug but has many interactions. Therefore, we report this case as a cautionary statement for all neurologists. Also, the measurement of QT time may be a valuable method of assessing clarithromycin excess.
- Citation: Shiraishi W. Possible convulsion and electroencephalographic abnormality in a patient taking long-term oral clarithromycin: A case report. World J Neurol 2022; 8(2): 10-13
- URL: https://www.wjgnet.com/2218-6212/full/v8/i2/10.htm
- DOI: https://dx.doi.org/10.5316/wjn.v8.i2.10
Although many drugs are known to cause drug-induced seizures, there are very few reports of clarithromycin-induced seizures[1,2]. Clarithromycin is a macrolide antibiotic that is used frequently for upper respiratory tract infections and otolaryngological infections and is considered to be safe[3]. In this case report, we show a case of convulsions with electroencephalography (EEG) abnormalities in a patient who had been taking clarithromycin for over ten years. After the discontinuation of clarithromycin, the EEG abnormality disappeared, and there was no recurrence of convulsive seizures.
In this case, the QTc showed a prolonged tendency in the electrocardiography (ECG) during the convulsions, which may have reflected the excessive clarithromycin state. Thus, clarithromycin-induced epilepsy is sporadic, and we report this case based on a discussion of its pathophysiological mecha
Seizure.
A 52-year-old Japanese male with no past history of seizure was admitted to our hospital with generalized tonic-clonic seizure.
A detailed interview revealed that the patient had been taking clarithromycin (400 mg/d) for > 10 years to treat chronic sinusitis and had recently added diltiazem (100 mg/d) for hypertension, as prescribed by his family doctor.
Nothing particular.
On admission, his seizure subsided. His vital signs showed no remarkable abnormalities. He had bit his tongue, but no incontinence was observed. He was alert and showed no neurological deficits.
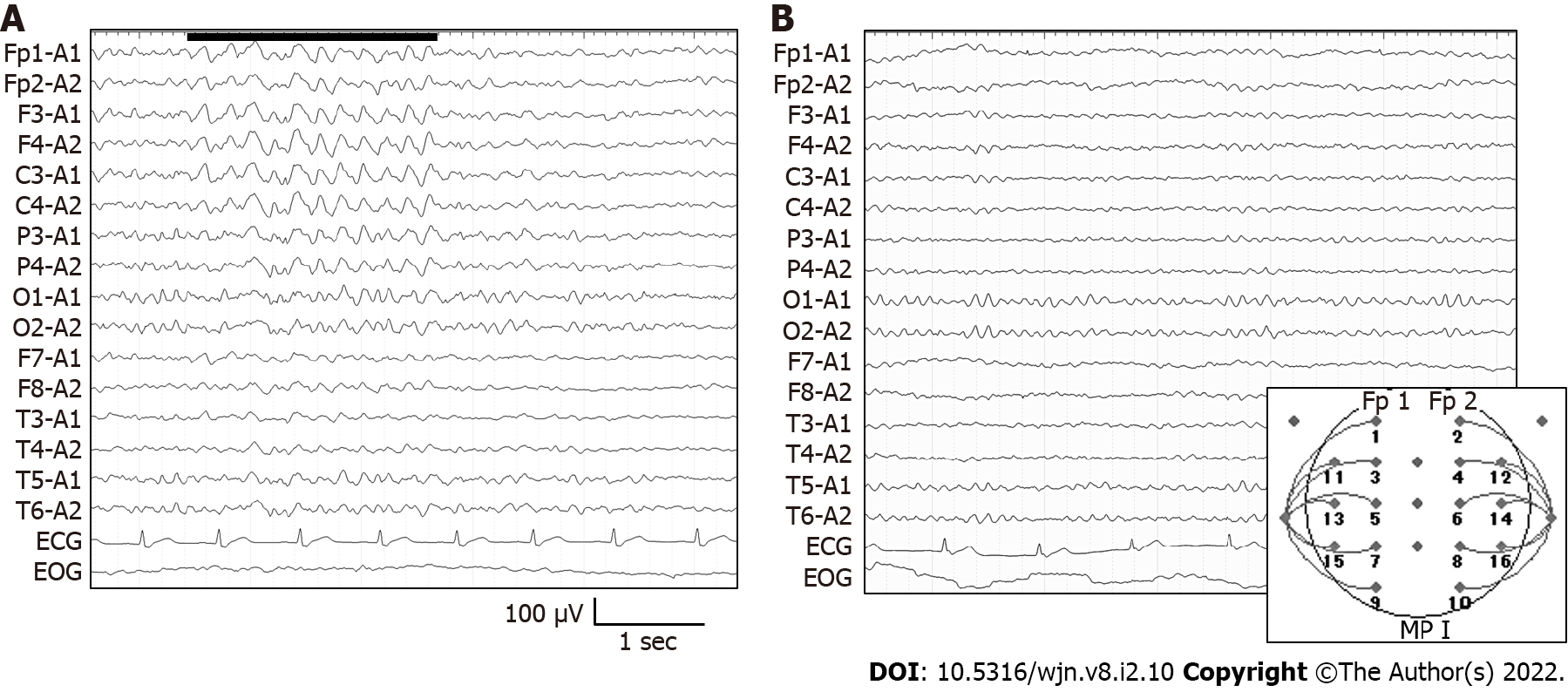
Laboratory examination showed a mild increase of HbA1c (6.6%; normal, 4.6%-6.2%). Since it was a night emergency, the blood concentration of clarithromycin could not be measured. No other abnormalities, including electrolytes, serum creatine phosphokinase, and lactate, were observed. Electroencephalography (EEG) showed frequent frontal intermittent rhythmic delta activities (FIRDA) (Figure 1A). On ECG, his QTc interval was 448 milliseconds (Bazett's formula[4]; normal, < 450 milliseconds[5]).
Head computed tomography, and magnetic resonance imaging revealed no brain abnormalities.
We diagnosed clarithromycin-induced seizures and determined that antiepileptic drugs were unnece
The cessation of clarithromycin ameliorated the EEG abnormalities. Also, he experienced no seizures to date.
His EEG showed a normal pattern without FIRDA (Figure 1B), and his QTc interval was 385 milli
Clarithromycin has often been reported to cause psychiatric symptoms such as delirium[6] and manic episodes[7], suggesting that clarithromycin may sometimes show central nervous system side effects. However, the clarithromycin-induced seizure is quite rare, with few previous reports[1,2]. Clarithromycin is reported to increase neuronal activity, stimulate CA3 pyramidal neurons of the hippocampus by reducing GABAergic signaling, and cause neuronal hyperexcitability[8]. However, the detailed mechanism of these effects is unknown, and further study is needed. Long-term macrolide usage is common for bronchiectasis, chronic obstructive pulmonary disease, and chronic rhinosinusitis[3]. Our patient had been prescribed clarithromycin for chronic sinusitis for > 10 years. Liver CYP3A4 has been reported to metabolize clarithromycin[2]. In the present case, diltiazem was added as an antihypertensive just before the seizure. Diltiazem is also reported to inhibit CYP3A[9]. Thus, in the present case, the introduction of diltiazem may have increased the blood concentration of clarithromycin. Administering azithromycin instead of clarithromycin may be an option. Clarithromycin also causes QT interval prolongation. Our case showed a QTc time of 448 milliseconds at admission, and after discontinuation of clarithromycin, his QTc time improved to 385 milliseconds. Measurement of QT time may be a valuable method of assessing clarithromycin excess. Clarithromycin is a frequently used medication and has a long history of use. The rarity of reports of convulsions induced by clarithromycin suggests that the induction of convulsions by clarithromycin is a rare phenomenon or has been overlooked. Clarithromycin is a frequently prescribed drug but has many interactions. Therefore, we report this case as a cautionary statement for all neurologists.
We thank all the neurophysiological department workers for obtaining excellent EEG and ECG.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Neurosciences
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bello AK, Nigeria; Liao JX, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Wanleenuwat P, Suntharampillai N, Iwanowski P. Antibiotic-induced epileptic seizures: mechanisms of action and clinical considerations. Seizure. 2020;81:167-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (2)] |
| 2. | Bandettini di Poggio M, Anfosso S, Audenino D, Primavera A. Clarithromycin-induced neurotoxicity in adults. J Clin Neurosci. 2011;18:313-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Smith D, Du Rand I, Addy CL, Collyns T, Hart SP, Mitchelmore PJ, Rahman NM, Saggu R. British Thoracic Society guideline for the use of long-term macrolides in adults with respiratory disease. Thorax. 2020;75:370-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 4. | HC B. An Analysis of the Time-Relations of Electrocardiograms. Heart. 1920;353. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Schwartz PJ, Crotti L, Insolia R. Long-QT syndrome: from genetics to management. Circ Arrhythm Electrophysiol. 2012;5:868-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 378] [Cited by in RCA: 455] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 6. | Pejčić AV. Delirium associated with the use of macrolide antibiotics: a review. Int J Psychiatry Clin Pract. 2022;26:29-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Neufeld NH, Mohamed NS, Grujich N, Shulman K. Acute Neuropsychiatric Symptoms Associated With Antibiotic Treatment of Helicobacter Pylori Infections: A Review. J Psychiatr Pract. 2017;23:25-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Bichler EK, Elder CC, García PS. Clarithromycin increases neuronal excitability in CA3 pyramidal neurons through a reduction in GABAergic signaling. J Neurophysiol. 2017;117:93-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Renton KW. Inhibition of hepatic microsomal drug metabolism by the calcium channel blockers diltiazem and verapamil. Biochem Pharmacol. 1985;34:2549-2553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 102] [Article Influence: 2.6] [Reference Citation Analysis (0)] |