Peer-review started: September 1, 2016
First decision: October 26, 2016
Revised: November 12, 2016
Accepted: December 16, 2016
Article in press: December 19, 2016
Published online: March 28, 2017
Processing time: 205 Days and 23.7 Hours
Alcohol is a well-recognized teratogen that can cause variable physical and behavioral effects on the fetus. Alcohol use and abuse during pregnancy is one of the major health and societal problems and has been linked to a wide range of birth defects in the offspring collectively termed as fetal alcohol spectrum disorder (FASD). The severity of abnormalities may depend on a number of factors that include the amount, the frequency, the period during gestation and the route of alcohol administration. The current knowledge about the neurobiological basis of FASD is limited. However, recent studies have suggested that the membrane-derived lipids especially bioactive endogenous cannabinoids (eCB) such as arachidonyl ethanolamide and 2-arachidonyl glycerol resulting from alcohol exposure, may play a significant role in modulating neurophysiological and neurobehavioral effects in chronic alcohol exposed adult animals. Based on these findings and on reported studies on the role of eCB signaling in neurodevelopment and behavior, it is speculated that the eCB signaling may play a critical role in fetal alcohol syndrome and FASD-related behavioral effects. The current discussion will touch upon some of the mechanistic explanations about the role of eCB signaling system in FASD and provide further guidance for future direction.
Core tip: Drinking during pregnancy leads to severe neurobiological consequences in the fetus and results in a variety of morphological and neurobehavioral abnormalities including mental retardation. One of the promising neurobiological mechanisms that can explain fetal alcohol spectrum disorder as discussed in this editorial is that of the possible role of alcohol-induced alteration in the levels of bioactive endogenous cannabinoids (eCBs) that are derived from membrane lipids and eCB signaling. Further studies exploring dietary supplementation with unsaturated fatty acids that can regulate the levels of the eCBs and testing of the drugs targeted against the eCB signaling, may have significant therapeutic value.
- Citation: Hungund BL. Drinking during pregnancy: Potential role of endocannabinoid signaling in fetal alcohol effects. World J Neurol 2017; 7(1): 1-5
- URL: https://www.wjgnet.com/2218-6212/full/v7/i1/1.htm
- DOI: https://dx.doi.org/10.5316/wjn.v7.i1.1
Alcohol use and abuse during pregnancy has been linked to a wide range of birth defects that include anatomical, physiological and behavioral abnormalities in the offspring collectively termed as fetal alcohol spectrum disorder (FASD)[1-3]. Although the risk is much greater with heavy and binge drinking, exposure even to a small amount of alcohol for a shorter period during critical periods of gestation has been shown to be sufficient to produce birth defects in animal models[3-9]. Mental retardation, learning disabilities and craniofacial defects are some of the reported abnormalities that result from alcohol-induced impairment of central nervous system (CNS) development[2]. A key question has been; whether there is a threshold for vulnerability below which alcohol can be consumed safely without harming the developing fetus? What is also not clear is that of molecular mechanisms underlying FASD-related neurophysiological, neuroanatomical and neurobehavioral abnormalities and neurodegeneration. In this editorial I will present evidence for a potential role, the eCB signaling system may play during fetal growth and development and attempt to provide mechanistic explanation, for involvement of the endocannabinoid (eCB) signaling system in FASD resulting from maternal drinking during pregnancy.
Alcohol can cause alterations in normal growth and development beginning from embryonic stage through fetal stage leading to a range of birth defects. Between third and six weeks of fertilization the CNS begins to form[10]. During this critical period of fetal growth, any insult such as alcohol, may result in accumulation of significant amount of alcohol in maternal placenta and in fetal tissue longer than the maternal tissue because of lack of alcohol metabolizing enzyme in fetal tissue[11]. This may cause disruption in normal development of nervous system machinery. The documented studies suggest that exposure to alcohol during first trimester leads to facial deformations, while exposure during second trimester can disrupt neuronal formation and neuronal connectivity and third trimester exposure interferes with CNS development[10,12-15]. It has also been reported that children of binge drinking pregnant women exhibited rather severe cognitive and behavioral deficits[13]. Adolescence is a critical stage during brain development, which is characterized by neuronal maturation, myelination and synaptic plasticity and any interference by alcohol during this critical period of fetal growth may hamper proper nervous system development[14]. These changes in the brain affect every developmental events that include emerging sexuality, emotionality and judgment in the offspring.
Although much remains to be understood with regard to neurobiological changes in the offspring due to maternal alcohol use and abuse during pregnancy, recent studies with pre-clinical models provide some intriguing information regarding possible neurobiological mechanisms underlying deleterious effects of in utero alcohol exposure in the offspring. The primary focus of studies aimed at defining mechanisms have been placental dysfunction, nutritional deficiency, acetaldehyde toxicity, fetal hypoxia and the role of prostaglandins[12,15]. Other mechanisms discussed in the literature are; alterations in regulation of gene expression, enhancement of free radical formation and excitotoxic neuroinflammatory microglial activation[8,9,16]. Recent studies also suggest that alcohol’s effect is mediated via several intracellular signal transduction pathways involving many classical transmitters[16]. Alcohol may cause FASD effects by disrupting membrane proteins such as neurotransmitter receptors (e.g., NMDA, GABA and glutamate and ion channels)[17]. However, significant new developments have emerged in recent years, which can provide better mechanistic explanation of the FASD. Major focus of the current discussion will be on one of the alternate mechanisms namely, on the role of membrane-derived bioactive lipids specifically eCBs that act through central cannabinoid (CB) receptors.
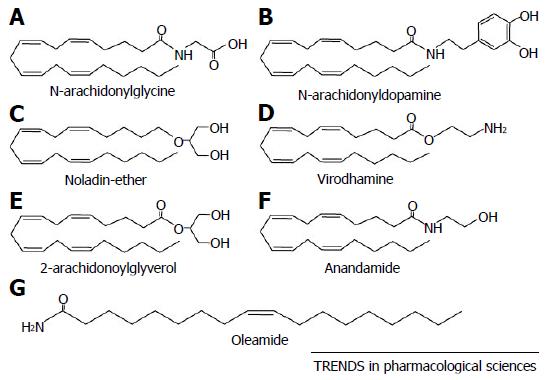
The eCB system consists of CB1 and 2 receptors, their endogenous ligands, the eCBs, arachidonyl ethanolamide (AEA), 2-Arachidonyl glycerol (2-AG), and the enzymes involved in their synthesis, degradation and transport[18-20]. Besides the well characterized eCBs, AEA and 2-AG, much remains to be understood about the lesser known eCBs such as palmitoyl and oleoyl ethanolamides, which may also have some physiological roles (Figure 1). The eCBs are considered as a new class of neuromodulator and are found abundantly in cerebral cortex, basal ganglia and limbic structures, and exert their effects mainly through the CB receptors[21,22]. Since their discovery, the eCBs and their signaling have gained prominence in recent years and have been implicated in a variety of health and diseases. The CB1 receptor has been found to be the most abundant presynaptic G-protein coupled receptor[23].
The role of the eCB system in alcohol-induced neurotoxicity is complex and much remains to be understood. The eCB system is suggested to play an important role during brain development and is implicated in prenatal wiring of the brain during developmental processes such as neuronal cell proliferation, cell migration and differentiation and stem cell proliferation[24,25]. It has been demonstrated in earlier studies that the eCB system is present in early embryo before neurogenesis suggesting its role in early embryogenesis[26]. It is also of significance to note that the eCBs are reported to be present in placenta and possibly in peripheral fetal tissue[27].
It has also been reported that eCBs and CB1 receptors play critical roles in directional migration of neuroblasts and subsequent synaptogenesis and neuron to neuron communication[28]. The levels of the two eCBs, AEA and 2-AG significantly fluctuate during CNS development[29]. The levels of eCB, AEA increases during embryo implantation and during early phase of organogenesis. On the other hand, 2-AG levels increase gradually and reach peak levels during synaptogenesis[29]. Thus any disruption in eCB signaling due to circumstances such as alcohol exposure may result in a broad array of neurodevelopmental abnormalities. The eCB system plays a crucial role during brain development by modulating neuronal function and neurogenesis[24]. It is demonstrated that the activation of CB1 and CB2 receptors modulates the rate of neurogenesis[24]. The significance of the eCB system during fetal development and growth is further supported by the observation that pharmacological blockade of CB1 receptors in mid-to-late gestational periods adversely affects the progenitor proliferation in subventricle zone, disrupts axonal path finding and results in cortical delamination[30]. Furthermore, in utero exposure to tetrahydrocannabinol led to inappropriate interneuron positioning during corticogenesis[31]. The CB1 receptor expression is found to increase dramatically from infancy to young adulthood in regions such as prefrontal cortex (PFC), striatum, and hippocampus[32]. These changes in receptor expression may be both regionally and temporally specific as demonstrated in some specific brain regions such as shell and core, and PFC during adolescence[31]. Similar to CB receptors, developmental changes in eCBs, AEA and 2-AG during adolescence have also been reported[33,34]. The eCB system is one of the major neuromodulatory system and plays a critical role in mediating release of neurotransmitters in the CNS[35,36]. CB1 receptors are present on cells such as astrocytes, microglia and oligodendrocytes[37,38], which may affect the white matter development because of the exposure to teratogen like alcohol[39]. Similarly, effect on grey matter development may result in hippocampal and amygdala volume changes[40-42]. Furthermore, PFC neurons during adolescence may also be affected by in utero alcohol exposure and results in functional effect on GABA release by CB1 receptor activation that are co-expressed on GABAergic neurons in PFC. Consequently, this may affect inhibitory inputs to pyramidal neurons in the PFC resulting in impaired cognitive function[43]. Activation of CB1 receptors also results in increased extracellular dopamine thereby enhancing the dopaminergic activity[43].
Further support for a role for eCB signaling system is derived from recent reports, which suggest that pharmacological or genetic manipulation of CB1 receptors reverses alcohol-induced learning and memory, emotion and anxiety, reward, eating, nociception and motor systems, among others in a neonatal alcohol exposure model[16].
Although there is considerable amount of literature on the role of eCB signaling system in sensitivity to, tolerance and dependence on alcohol in adult animals[18,19], there have not been any studies directly implicating eCB system in FASD. Except for a handful of studies, where a neonatal model for alcohol exposure on post-natal days 4-10, a period equivalent to third trimester in humans when significant brain development and rapid synaptic growth occurs, a significant effect of alcohol on the eCB system[16,44] and subsequent neurobehavioral deficits, have been demonstrated (for details see the review[16]). The current hypothesis/speculation is based on the existing knowledge of the association of developmental changes in the components of the eCB system with neurophysiological and neurobehavioral status and observed teratogenic effect of alcohol in the developing fetus. Therefore, I believe that there indeed is sufficient supporting evidence that directly links eCB system to FASD-related neurophysiological and neurobehavioral deficits in the offspring exposed to alcohol in utero. However further studies as suggested here will enhance further understanding of the role eCB signaling plays in FASD and future development of therapeutic strategies to treat FASD-related neuroanatomical, neurobehavioral and other neurophysiological deficiencies.
As presented here, the existence of eCB synthesizing and metabolizing machinery in placenta and throughout various stages of neurodevelopment beginning from embryogenesis to adolescence and adulthood, strongly support a role for bioactive eCBs in FASD. Furthermore, alcohol-induced production of bioactive lipids may also contribute to dysfunctional/abnormal functioning of the eCB signaling leading to disrupted neuronal wiring, neuronal communication mechanisms and neurotransmitter function. This is evidenced by fluctuating levels of eCBs throughout fetal development and growth. As an example, it is reported that diacyl glycerol lipase, that synthesizes 2-AG, and CB1 receptors are a requirement for axonal growth and guidance and for retrograde synaptic signaling during early development. However, the expression of 2-AG changes from axonal tracts in the embryo to dendritic fields in the adult. This is highlighted in developmental changes in requirement from pre to post - synaptic compartment[45]. Alterations in eCB signaling may lead to improper neuronal connections and communication and thus may lead to many of the neurobehavioral deficits observed in the offspring exposed alcohol in utero. It is of great value to explore further and understand the contribution of eCB signaling towards FASD and investigate whether manipulation of the components of the eCB signaling system pharmacologically or genetically could produce beneficial effects in alleviating the alcohol-induced FASD.
The following important conclusions can be drawn based on the evidence presented here that: (1) maternal alcohol use during pregnancy leads to a variety of neuroanatomical, neurobehavioral and neurophysiological abnormalities (FASD), severity of which may depend on the amount and duration of alcohol consumed, route of alcohol administration and gestational period during pregnancy; (2) the abnormalities may be the result of alcohol’s interference with normal developmental processes, especially the nervous system development. The alcohol’s effect may last longer or even irreversible in the offspring and may translate into neurocognitive, neurobehavioral and neuropsychiatric disorders; and (3) one among the many speculative mechanistic explanations, the proposed role for eCB signaling, may be well equipped to explain many aspects of the consequential events due to alcohol exposure that lead to FASD. Further studies exploring the manipulation of eCB signaling using pharmacological or genetic tools may yield valuable information regarding the neurobiological processes underlying FASD. The investigation of pharmacological agents targeting eCB signaling system may be a worthwhile proposition to find a therapeutic solution to the deleterious effect of in utero alcohol exposure that leads to FASD and related abnormalities in the offspring.
The author would like to thank Professor Christopher Evans for his critique and Dr. Vinod Yaragdri for his critical reading and for his help in preparation of the manuscript.
Manuscript source: Invited manuscript
Specialty type: Clinical neurology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gibert Y, May PA, Pan HC, Sotelo J S- Editor: Qiu S L- Editor: A E- Editor: Li D
| 1. | Jones KL, Smith DW, Ulleland CN, Streissguth P. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;1:1267-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1594] [Cited by in RCA: 1283] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 2. | Streissguth AP, Landesman-Dwyer S, Martin JC, Smith DW. Teratogenic effects of alcohol in humans and laboratory animals. Science. 1980;209:353-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 534] [Cited by in RCA: 462] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 3. | Webster WS, Walsh DA, McEwen SE, Lipson AH. Some teratogenic properties of ethanol and acetaldehyde in C57BL/6J mice: implications for the study of the fetal alcohol syndrome. Teratology. 1983;27:231-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 232] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Sulik KK, Johnston MC. Sequence of developmental alterations following acute ethanol exposure in mice: craniofacial features of the fetal alcohol syndrome. Am J Anat. 1983;166:257-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 177] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Randall CL. Alcohol as a teratogen: a decade of research in review. Alcohol Alcohol Suppl. 1987;1:125-132. [PubMed] |
| 6. | Hungund BL, Gokhale VS, Cooper T, Mahadik SP. Prenatal Ganglioside GM1 Treatment Protects Ethanol-Induced Sleep Time in Rats Exposed to Ethanol In Utero During Gestation Days 7 and 8. Drug Devel Res. 1991;24:261-267. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Hungund BL, Ross DC, Gokhale VS. Ganglioside GM1 reduces fetal alcohol effects in rat pups exposed to ethanol in utero. Alcohol Clin Exp Res. 1994;18:1248-1251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Riley EP, Thomas JD, Goodlett CR, Klintsova AY, Greenough WT, Hungund BL, Zhou F, Sari Y, Powrozek T, Li TK. Fetal alcohol effects: mechanisms and treatment. Alcohol Clin Exp Res. 2001;25:110S-116S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Charness ME, Riley EP, Sowell ER. Drinking During Pregnancy and the Developing Brain: Is Any Amount Safe? Trends Cogn Sci. 2016;20:80-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | O’Neil E. Developmental Timeline of Alcohol-Induced Birth Defects. Embryo Project Encyclopedia. [updated 2011 Apr 24]. Available from: http://embryo.asu.edu/handle/10776/2101. |
| 11. | Zorzano A, Herrera E. Disposition of ethanol and acetaldehyde in late pregnant rats and their fetuses. Pediatr Res. 1989;25:102-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Chen SY, Periasamy A, Yang B, Herman B, Jacobson K, Sulik KK. Differential sensitivity of mouse neural crest cells to ethanol-induced toxicity. Alcohol. 2000;20:75-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Mattson SN, Riley EP. A review of the neurobehavioral deficits in children with fetal alcohol syndrome or prenatal exposure to alcohol. Alcohol Clin Exp Res. 1998;22:279-294. [PubMed] |
| 14. | Streissguth AP, Aase JM, Clarren SK, Randels SP, LaDue RA, Smith DF. Fetal alcohol syndrome in adolescents and adults. JAMA. 1991;265:1961-1967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 479] [Cited by in RCA: 364] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 15. | Randall CL, Ekblad U, Anton RF. Perspectives on the pathophysiology of fetal alcohol syndrome. Alcohol Clin Exp Res. 1990;14:807-812. [PubMed] |
| 16. | Basavarajappa BS. Fetal Alcohol Spectrum Disorder: Potential Role of Endocannabinoids Signaling. Brain Sci. 2015;5:456-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 17. | Alfonso-Loeches S, Guerri C. Molecular and behavioral aspects of the actions of alcohol on the adult and developing brain. Crit Rev Clin Lab Sci. 2011;48:19-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 172] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 18. | Hungund BL, Vinod KY. Roles of the Endocannabinoid System in Alcohol-Related Behaviors. Open Neurop. 2009;2:31-39. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Vinod KY, Hungund BL. Endocannabinoid lipids and mediated system: implications for alcoholism and neuropsychiatric disorders. Life Sci. 2005;77:1569-1583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Vinod KY, Hungund BL. Role of the endocannabinoid system in depression and suicide. Trends Pharmacol Sci. 2006;27:539-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 92] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Devane WA, Hanus L, Breuer A, Pertwee RG, Stevenson LA, Griffin G, Gibson D, Mandelbaum A, Etinger A, Mechoulam R. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science. 1992;258:1946-1949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3980] [Cited by in RCA: 3982] [Article Influence: 120.7] [Reference Citation Analysis (0)] |
| 22. | Mechoulam R, Hanuš LO, Pertwee R, Howlett AC. Early phytocannabinoid chemistry to endocannabinoids and beyond. Nat Rev Neurosci. 2014;15:757-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 247] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 23. | Herkenham M, Lynn AB, Little MD, Johnson MR, Melvin LS, de Costa BR, Rice KC. Cannabinoid receptor localization in brain. Proc Natl Acad Sci USA. 1990;87:1932-1936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1558] [Cited by in RCA: 1638] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 24. | Maccarrone M, Guzmán M, Mackie K, Doherty P, Harkany T. Programming of neural cells by (endo)cannabinoids: from physiological rules to emerging therapies. Nat Rev Neurosci. 2014;15:786-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 217] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 25. | Aguado T, Palazuelos J, Monory K, Stella N, Cravatt B, Lutz B, Marsicano G, Kokaia Z, Guzmán M, Galve-Roperh I. The endocannabinoid system promotes astroglial differentiation by acting on neural progenitor cells. J Neurosci. 2006;26:1551-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 197] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 26. | Psychoyos D, Vinod KY, Cao J, Xie S, Hyson RL, Wlodarczyk B, He W, Cooper TB, Hungund BL, Finnell RH. Cannabinoid receptor 1 signaling in embryo neurodevelopment. Birth Defects Res B Dev Reprod Toxicol. 2012;95:137-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 27. | Fonseca BM, Correia-da-Silva G, Taylor AH, Lam PM, Marczylo TH, Bell SC, Konje JC, Teixeira NA. The endocannabinoid 2-arachidonoylglycerol (2-AG) and metabolizing enzymes during rat fetoplacental development: a role in uterine remodelling. Int J Biochem Cell Biol. 2010;42:1884-1892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Berghuis P, Rajnicek AM, Morozov YM, Ross RA, Mulder J, Urbán GM, Monory K, Marsicano G, Matteoli M, Canty A. Hardwiring the brain: endocannabinoids shape neuronal connectivity. Science. 2007;316:1212-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 405] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 29. | Fernández-Ruiz JJ, Berrendero F, Hernández ML, Romero J, Ramos JA. Role of endocannabinoids in brain development. Life Sci. 1999;65:725-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 83] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 30. | Mulder J, Aguado T, Keimpema E, Barabás K, Ballester Rosado CJ, Nguyen L, Monory K, Marsicano G, Di Marzo V, Hurd YL. Endocannabinoid signaling controls pyramidal cell specification and long-range axon patterning. Proc Natl Acad Sci USA. 2008;105:8760-8765. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 263] [Cited by in RCA: 243] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 31. | Berghuis P, Dobszay MB, Wang X, Spano S, Ledda F, Sousa KM, Schulte G, Ernfors P, Mackie K, Paratcha G. Endocannabinoids regulate interneuron migration and morphogenesis by transactivating the TrkB receptor. Proc Natl Acad Sci USA. 2005;102:19115-19120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 207] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 32. | Mato S, Del Olmo E, Pazos A. Ontogenetic development of cannabinoid receptor expression and signal transduction functionality in the human brain. Eur J Neurosci. 2003;17:1747-1754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 164] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 33. | Wenger T, Gerendai I, Fezza F, González S, Bisogno T, Fernandez-Ruiz J, Di Marzo V. The hypothalamic levels of the endocannabinoid, anandamide, peak immediately before the onset of puberty in female rats. Life Sci. 2002;70:1407-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 34. | Ellgren M, Artmann A, Tkalych O, Gupta A, Hansen HS, Hansen SH, Devi LA, Hurd YL. Dynamic changes of the endogenous cannabinoid and opioid mesocorticolimbic systems during adolescence: THC effects. Eur Neuropsychopharmacol. 2008;18:826-834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 186] [Cited by in RCA: 173] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 35. | Wilson RI, Nicoll RA. Endogenous cannabinoids mediate retrograde signalling at hippocampal synapses. Nature. 2001;410:588-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1070] [Cited by in RCA: 1191] [Article Influence: 49.6] [Reference Citation Analysis (0)] |
| 36. | Hillard CJ. The Endocannabinoid Signaling System in the CNS: A Primer. Int Rev Neurobiol. 2015;125:1-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 90] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 37. | Bouaboula M, Bourrié B, Rinaldi-Carmona M, Shire D, Le Fur G, Casellas P. Stimulation of cannabinoid receptor CB1 induces krox-24 expression in human astrocytoma cells. J Biol Chem. 1995;270:13973-13980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 133] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 38. | Sánchez C, Galve-Roperh I, Canova C, Brachet P, Guzmán M. Delta9-tetrahydrocannabinol induces apoptosis in C6 glioma cells. FEBS Lett. 1998;436:6-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 211] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 39. | Bava S, Frank LR, McQueeny T, Schweinsburg BC, Schweinsburg AD, Tapert SF. Altered white matter microstructure in adolescent substance users. Psychiatry Res. 2009;173:228-237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 143] [Cited by in RCA: 132] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 40. | Bangalore SS, Prasad KM, Montrose DM, Goradia DD, Diwadkar VA, Keshavan MS. Cannabis use and brain structural alterations in first episode schizophrenia--a region of interest, voxel based morphometric study. Schizophr Res. 2008;99:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 41. | Yücel M, Solowij N, Respondek C, Whittle S, Fornito A, Pantelis C, Lubman DI. Regional brain abnormalities associated with long-term heavy cannabis use. Arch Gen Psychiatry. 2008;65:694-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 314] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 42. | Eggan SM, Hashimoto T, Lewis DA. Reduced cortical cannabinoid 1 receptor messenger RNA and protein expression in schizophrenia. Arch Gen Psychiatry. 2008;65:772-784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 186] [Cited by in RCA: 176] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 43. | Malone DT, Hill MN, Rubino T. Adolescent cannabis use and psychosis: epidemiology and neurodevelopmental models. Br J Pharmacol. 2010;160:511-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 147] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 44. | Subbanna S, Psychoyos D, Xie S, Basavarajappa BS. Postnatal ethanol exposure alters levels of 2-arachidonylglycerol-metabolizing enzymes and pharmacological inhibition of monoacylglycerol lipase does not cause neurodegeneration in neonatal mice. J Neurochem. 2015;134:276-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 45. | Bisogno T, Howell F, Williams G, Minassi A, Cascio MG, Ligresti A, Matias I, Schiano-Moriello A, Paul P, Williams EJ. Cloning of the first sn1-DAG lipases points to the spatial and temporal regulation of endocannabinoid signaling in the brain. J Cell Biol. 2003;163:463-468. [PubMed] |