Revised: August 1, 2013
Accepted: August 16, 2013
Published online: September 28, 2013
Processing time: 90 Days and 21.7 Hours
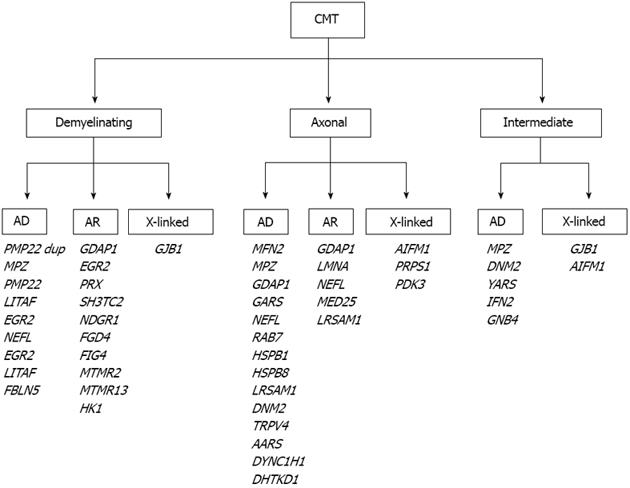
Charcot-Marie-Tooth (CMT) disease or hereditary motor and sensory neuropathy is the most common inherited neuromuscular disorder affecting at least 1 in 2500. CMT disease is pathologically and genetically heterogeneous and is characterized by a variable age of onset, slowly progressive weakness and muscle atrophy, starting in the lower limbs and subsequently affecting the upper extremities. Symptoms are usually slowly progressive, especially for the classic and late-onset phenotypes, but can be rather severe in early-onset forms. CMT is grouped into demyelinating, axonal and intermediate forms, based on electrophysiological and pathological findings. The demyelinating types are characterized by severely reduced motor nerve conduction velocities (MNCVs) and mainly by myelin abnormalities. The axonal types are characterized by normal or slightly reduced MNCVs and mainly axonal abnormalities. The intermediate types are characterized by MNCVs between 25 m/s and 45 m/s and they have features of both demyelination and axonopathy. Inheritance can be autosomal dominant, X-linked, or autosomal recessive. Mutations in more than 30 genes have been associated with the different forms of CMT, leading to major advancements in molecular diagnostics of the disease, as well as in the understanding of pathogenetic mechanisms. This editorial aims to provide an account that is practicable and efficient on the current molecular diagnostic procedures for CMT, in correlation with the clinical, pathological and electrophysiological findings. The most frequent causative mutations of CMT will also be outlined.
Core tip: Charcot-Marie-Tooth (CMT) disease is the most common neuromuscular disorder affecting at least 1 in 2500. CMT according to electrophysiological and pathological findings is categorised into demyelinating, axonal and intermediate forms and inheritance can be autosomal dominant, X-linked, or autosomal recessive. More than 30 causative genes have been identified. This editorial aims to present an efficient account of molecular diagnostic procedures for CMT, based on clinical, pathological and electrophysiological findings as well as summarize the most frequent causative mutations.
- Citation: Nicolaou P, Christodoulou K. Advances in the molecular diagnosis of Charcot-Marie-Tooth disease. World J Neurol 2013; 3(3): 42-55
- URL: https://www.wjgnet.com/2218-6212/full/v3/i3/42.htm
- DOI: https://dx.doi.org/10.5316/wjn.v3.i3.42
Charcot-Marie-Tooth (CMT) disease, also known as Charcot-Marie-Tooth neuropathy, hereditary motor and sensory neuropathy (HMSN) and Peroneal Muscular Atrophy was first described by Charcot et al[1] and Tooth[2] in 1886. CMT is the most common inherited neuromuscular disorder, with a prevalence of 17-40 per 100000 individuals[3,4]. Clinically, it is characterized by a variable age of onset and a variable phenotype. The main features of CMT comprise, a slowly progressive symmetric weakness and muscle atrophy of the peroneal and distal muscles of the lower limbs, sensory loss, foot deformities (pes cavus and hammer toes), and decreased or absent tendon reflexes. Hands and forearms are affected later in life. Bilateral pes cavus is almost invariably present with substantial variation in the level of sensory symptoms and signs[5]. According to electrophysiological and pathological findings CMT is classified into demyelinating, axonal and intermediate forms. The demyelinating types (CMT1 or HMSN I) are characterized by severely reduced motor nerve conduction velocities (MNCVs) (median nerve MNCV < 38 m/s) and mainly by myelin abnormalities on nerve biopsy including onion bulbs[6]. The axonal types (CMT2 or HMSN II) with primarily axonal degeneration are characterized by normal or slightly reduced motor nerve conduction velocities (median nerve MNCV > 38 m/s) but reduced amplitudes. Normal amplitudes are usually more than 4-6 μV, however this also differs between nerves[7-9]. Intermediate types include CMT patients that have features of both demyelination and axonopathy with median nerve MNCVs ranging from 25 to 45 m/s[10]. Inheritance in CMT can be autosomal dominant (AD)[11], X-linked[12,13], or autosomal recessive[14,15]. More than 50 loci and more than 30 CMT genes have thus far been identified (Table 1, http://neuromuscular.wustl.edu/time/hmsn.html).The majority of CMT patients worldwide have been characterized at the molecular genetic level. More than 70% of all CMT patients have mutations in one of four genes: PMP22, GJB1, MPZ, and MFN2. Approximately 25% of CMT patients are still pending molecular diagnosis, the great majority of them with CMT2[16]. Despite major advances in the identification of causative CMT genes, the related pathogenic mechanisms still remain to be clarified[17,18].
| Type | Locus | Gene | OMIM | Ref. |
| CMT1: Dominant demyelinating | ||||
| CMT1A | 17p12 | PMP22 | *601097 | [21,22] |
| CMT1B | 1q22 | MPZ | *159440 | [28] |
| CMT1C | 16p13 | LITAF (SIMPLE) | *603794 | [171] |
| CMT1D | 10q21.3 | EGR2 | *129009 | [37] |
| CMT1E | 17p12 | PMP22 | *601097 | [21,22] |
| CMT1F | 8p21 | NEFL | *162280 | [105] |
| CMT1 | 14q32 | FBLN5 | *604580 | [47] |
| CMT2: Dominant axonal | ||||
| CMT2A | 1p36.22 | MFN2 | *608507 | [51,52] |
| CMT2B | 3q21.3 | RAB7 | *602298 | [55] |
| CMT2C | 12q24.11 | TRPV4 | *605427 | [61] |
| CMT2D | 7p15 | GARS | *600287 | [64] |
| CMT2E | 8p21 | NEFL | *162280 | [66] |
| CMT2F | 7q11.23 | HSPB1 (HSP27) | *602195 | [69] |
| CMT2G | 12q12-13.3 | Unknown | ||
| CMT2H/2K | 8q21.11 | GDAP1 | *606598 | [76] |
| CMT 2I/2J | 1q22 | MPZ | *159440 | [80,81] |
| CMT2L | 12q24.3 | HSPB8 (HSP22) | *608014 | [83] |
| CMT2M | 19p13 | DNM2 | *602378 | [84] |
| CMT2N | 16q22.1 | AARS | *601065 | [89] |
| CMT2O | 14q32.31 | DYNC1H1 | *600112 | [93] |
| CMT2P | 9q33 | LRSAM1 | *610933 | [95,96] |
| CMT2Q | 10p14 | DHTKD1 | *614984 | [100] |
| DI-CMT: Dominant intermediate | ||||
| DI-CMTA | 10q24.1-q25.1 | Unknown | ||
| DI-CMTB | 19p13 | DNM2 | *602378 | [84] |
| DI-CMTC | 1p35.1 | YARS | *603623 | [106] |
| DI-CMTD | 1q22 | MPZ | *159440 | [10] |
| DI-CMTE | 14q32.33 | IFN2 | *610982 | [107] |
| DI-CMTF | 3q26.33 | GNB4 | *610863 | [108] |
| CMT4: Recessive demyelinating | ||||
| CMT 4A | 8q21.11 | GDAP1 | *606598 | [78] |
| CMT 4B-1 | 11q22 | MTMR2 | *603557 | [112] |
| CMT 4B-2 | 11p15 | MTMR13 (SBF2) | *607697 | [117] |
| CMT 4C | 5q23-33 | SH3TC2 | *608206 | [119] |
| CMT 4D | 8q24.3 | NDRG1 | *605262 | [125] |
| CMT 4E | 10q21.3 | EGR2 | *129010 | [37] |
| CMT 4F | 19q13.2 | PRX | *605725 | [43,129] |
| CMT 4G | 10q23.2 | HK1 | *142600 | [134] |
| CMT 4H | 12p11.21 | FGD4 | *611104 | [137,138] |
| CMT 4J | 6q21 | FIG4 | *609390 | [141] |
| AR-CMT2: Recessive axonal | ||||
| AR CMT 2A | 1q22 | LMNA | *150330 | [144] |
| AR CMT 2B | 19q13.3 | MED25 (ACID1) | *610197 | [146] |
| AR-CMT 2C | 8p21 | NEFL | *162280 | [66,150] |
| AR CMT2D | 8q21.11 | GDAP1 | *606598 | [76] |
| AR CMT2E | 9q33 | LRSAM1 | *610933 | [95,96] |
| CMTX: X-linked | ||||
| CMTX1 | Xq13.1 | GJB1 | *304040 | [153] |
| CMTX2 | Xp22.2 | Unknown | ||
| CMTX3 | Xq26.3-q27.1 | Unknown | ||
| CMTX4 | Xq26.1 | AIFM1 | *300169 | [161] |
| CMTX5 | Xq22.3 | PRPS1 | *311850 | [165] |
| CMTX6 | Xp22.11 | PDK3 | *602526 | [166] |
CMT is classified into the following 3 types, based on clinical and neurophysiological findings, the inheritance pattern and associated gene mutations.
CMT1 is the most common type of CMT and is divided into different subtypes based on molecular genetic findings.
CMT1A is the most common subtype (70% of demyelinating CMT and 40% of all CMT patients)[16,19,20]. CMT1A is caused by the duplication of a 1.4 Mb region on chromosome 17p12 that contains the peripheral myelin protein 22 (PMP22) gene[16,21-24]. De novo PMP22 duplication mutations occur in 6.5% of CMT1A patients. PMP22 protein is a hydrophobic 22 kDa glycoprotein that is expressed mainly in myelinating Schwann cells and plays an important role in myelination, proliferation and differentiation[25,26]. Overexpression of PMP22 gene dosage reduces the proliferation of Schwann cells and may affect the intracellular degradation of membrane components[3,27]. The onset of clinical symptoms is in the first or second decade of life, usually in childhood, characterized by a typical CMT phenotype, and usually a mild disease progress. However, disease severity is variable, even in individuals of the same family. In many cases there is also nerve hypertrophy (25%) and in some hearing loss (5%)[3]. The MNCVs are reduced (< 38 m/s) in the early stages of the disease.
CMT1B is caused by mutations in the myelin protein zero (MPZ or P0) gene, located on chromosome 1q22-q23 and account for about 5% of CMT1 cases[3,16,28]. MPZ protein is a 28 kDa glycoprotein that is located in Schwann cells. This protein is necessary for normal myelin structure and function and is found in abundance in the myelin of peripheral nerve tissues and is completely absent from the myelin of the central nervous system[27,29]. CMT1B is characterized by an early onset (usually first decade) and most MPZ mutations cause a classical CMT1 phenotype, however, some mutations cause a more severe Dejerine-Sottas syndrome (DSS-CMT3B) or congenital hypomyelination neuropathy (CHN)[30,31]. Patients with an early onset have reduced MNCVs and patients with a late onset have normal or slightly reduced MNCVs[32].
CMT1C is caused by mutations in the lipopolysaccharide-induced tumor necrosis factor (LITAF)/small integral membrane protein of lysosome late endosome (SIMPLE) gene. The gene is located on chromosome 16p13.1-p12.3 and plays an important role in protein degradation[33]. LITAF mutations account for less than 1% of CMT patients[34]. The first clinical symptoms in patients with CMT1C appear in the second decade with a typical CMT1 phenotype and conduction velocities around 16-25 m/s[3,33,35,36].
CMT1D accounts for less than 1% of CMT patients and is caused by mutations in the early growth response element 2 (EGR2) gene, that is located on chromosome 10q21.3[37]. EGR2 is a transcription factor that is involved in the regulation of myelin genes[38,39]. Most patients have very early onset CMT1 or the most severe DSS (DSS-EGR) or CHN phenotypes, however, patients with late onset and a milder phenotype have been described[37,40-43]. Patients with cranial nerve deficits, including diseases of the pulmonary system, respiratory failure, diplopia and vocal cord paresis have been reported[3,34]. Motor nerve conduction velocities are slightly to severely reduced (9-42 m/s)[3].
CMT1E is caused by point mutations in the PMP22 gene[21-23]. Patients with PMP22 point mutations have more severe symptoms than patients with CMT1A and usually have slower NCV[44]. Point mutations of PMP22 may cause various other phenotypes such as HNPP, DSS (CMT3A) or CHN[45].
CMT1F is caused by mutations in the neurofilament light chain (NEFL) gene located on chromosome 8q21. The encoded protein plays a role in intracellular transport of axons and dendrites[46]. The first symptoms of the disease appear in the first decade of life and are usually severe, with severely reduced MNCVs (15-38 m/s)[3]. NEFL mutations also cause CMT2E and CMT4C2.
CMT1G has been recently described and is caused by mutations in the fibulin-5 (FBLN5) gene on chromosome 14q32[47]. FBLN5 is located in an extracellular matrix and is a calcium-binding glycoprotein that plays an important role in elastic fiber assembly and in endothelial cell adhesion[48]. The age of onset, the phenotype and the MNCVs of the disease vary[47].
CMT2 accounts for 20% of all CMT patients and is characterized by normal or slightly reduced MNCVs[16,35].
CMT2A is the most common form of CMT2 and accounts for 20% of CMT2 patients[49,50]. It is caused by mutations in the mitofusin 2 (MFN2) gene, located on chromosome 1q36.22. A mutation in the kinesin motor protein 1B (KIF1B) gene has been reported in a Japanese family, but mutations in the KIF1B have not thus far been confirmed in any other family[51]. MFN2 is a large dynamin-like GTPase protein that plays an important role in the fusion of mitochondria. When this protein is modified as a result of gene mutations, it leads to an insufficient protein transfer between mitochondria and the axons of peripheral nerves[3]. Most patients (80%) have an early onset of symptoms (< 10 years old) with a severe phenotype and usually become wheelchair bound by 20 years of age. The remaining 20% of patients have a later onset of symptoms (10-50 years old) and a milder phenotype[52]. CMT2A patients with optic atrophy, hearing loss, cerebral white matter abnormalities and diabetes mellitus have been described[16,49,50,53,54]. Motor nerve conduction velocities are typically normal, however, the amplitudes are slightly to severely reduced or absent[54].
CMT2B is caused by mutations in the RAS-associated GTP-binding protein (RAB7) gene located on chromosome 3q21.3[55]. RAB7 is a GTPase protein that localizes to late endosomes and lysosomes and is involved in the regulation of late endocytic traffic[56,57]. Clinical symptoms appear between the second and fourth decades and include typical CMT phenotype and mild to moderate sensory loss, that often leads to foot ulcerations and subsequently infections and amputations[58,59]. MNCVs are normal to slightly reduced with usually reduced amplitude.
CMT2C is caused by mutations in the transient receptor potential vanilloid 4 (TRPV4) gene located on chromosome 12q24.11[60,61]. The TRPV4 protein is a cation channel (Ca2+ channel) that activates pathways leading to the regulation of systemic osmotic pressure[62]. CMT2C is characterized by weakness of proximal muscles, vocal cord, diaphragmatic paresis and occasionally a fatal outcome. Some other features have been reported including sensorineural hearing loss, raspy voice, bladder urgency and incontinence[7,61,62]. The age of onset is between the second and fifth decades of life and MNCVs are normal (> 50 m/s)[61,62].
CMT2D is caused by mutations in the glycyl-tRNA synthetase (GARS) gene located on chromosome 7p15[63,64]. The encoded protein plays an important role in translation processes and GARS gene mutations affect protein synthesis, which is important for the normal function of the motor nerve[3]. The first symptoms appear between first and forth decade and primarily affect the upper extremities and then to a lesser extent the lower extremities[64,65]. MNCVs are normal.
CMT2E is caused by mutations in the NEFL gene[66]. NEFL mutations also cause CMT1F and CMT4C2[66,67]. CMT2E is clinically similar to CMT1F, although typically it is less severe, with normal or slightly reduced MNCVs.
CMT2F is caused by mutations in the heat shock protein B1 (HSPB1, also known as HSP27) gene located on chromosome 7q11.23[68,69]. The HSPB1 protein protects the structure of other proteins (bind and prevent misfolding and aggregation of nascent proteins) and also interacts with the NEFL protein and protects motor neurons[57,70]. Symptoms progression is slow and they begin with symmetrical weakness of the lower extremities resulting in foot drop, foot deformities, and sensory dysfunctions and then progresses slowly to the upper extremities[71]. The age of onset of the disease is in the first or second decade of life and the MNCVs[72].
CMT2G maps to chromosome 12q12-q13.3 but associated gene mutations are still unknown[73,74]. The age of onset varies from the first to the eighth decade, although most patients developed symptoms in the second decade. Clinical symptoms include foot deformity and difficulty in walking, with very slow progression and absent ankle reflexes[73]. MNCVs are normal or mildly decreased.
CMT2H and CMT2K are caused by mutations in the ganglioside induced differentiation associated protein 1 (GDAP1) gene on chromosome 8q21.11[75,76]. GDAP1 mutations also cause axonal recessive CMT (CMT4C4) or demyelinating recessive CMT (CMT4A)[76-78]. The clinical symptoms in CMT2H/K appear in the second decade with a mild to moderate and slowly progressive phenotype with vocal cord paralysis and occasionally with optic nerve atrophy and normal or slightly reduced MNCVs[79].
CMT2I and CMT2J are caused by mutations in the MPZ gene[80,81]. The first symptoms appear very late (between 45 and 60) with a typical CMT2 phenotype, although there are some patients with pupillary abnormalities, deafness and sensory disturbances[16,81]. MNCVs are normal or slightly reduced (> 38 m/s), but during the progress of the disease they are decreased (< 38 m/s)[3].
CMT2L is caused by mutations in the heat shock 22 kDa protein 8 (HSPB8) gene, also known as heat shock protein 22 (HSP22) on chromosome 12q24[82,83]. HSPB8 is highly expressed in the spinal cord and in the motor and sensory neurons and is mainly localized to the plasma membrane. Also it possesses chaperone-like activity and inhibits protein aggregation and degrades misfolded proteins[57]. Clinical symptoms start between 15-35 years old and include distal muscle weakness and atrophy, mild sensory loss and scoliosis present in some patients. MNCVs are normal or near-normal.
CMT2M is caused by mutations in the dynamin 2 (DNM2) gene located on chromosome 19p13[84,85]. DNM2 is a large GTPase protein involved in membrane trafficking and endocytosis[86]. CMT2M is characterized by distal muscle weakness and atrophy of the lower extremities, mild weakness of upper extremities and foot deformities, including pes cavus and toe clawing[87,88]. The symptoms appear between the age of 20-55 years and the MNCVs are normal to slightly reduced.
CMT2N is caused by mutations in alanyl-tRNA synthetase (AARS) gene on chromosome 16q22.1[89]. AARS protein is an aminoacyl-tRNA synthetase (ARS). ARSs are ubiquitously expressed, essential enzymes that ligate amino acids to produce tRNAs needed for global protein synthesis[90]. Clinical features include mild to moderate weakness of lower limbs and milder or absent weakness of the upper limbs. Some patients had foot drop, pes cavus, hammer toes, absent ankle reflexes and hyporeflexia[89,91,92]. The age of onset is varying (6-54 years old) and MNCVs are normal.
CMT2O is caused by mutations in the dynein cytoplasmic 1 heavy chain 1 (DYNC1H1) gene on chromosome 14q32.31[93]. Dyneins are a group of ATPases that help to convert chemical into mechanical energy. Cytoplasmic dynein is a large motor protein complex that is involved in intracellular functions, including reversing axonal transport in neurons[93,94]. Clinical features include progressive distal lower limb weakness, pes cavus, variable sensory loss and in some patients proximal weakness and waddling gait[93]. The first symptoms occur in childhood and the MNCVs are normal.
CMT2P is caused by mutations in the leucine rich repeat and sterile alpha motif containing 1 (LRSAM1) gene on chromosome 9q33.3. The inheritance can be autosomal recessive (AR-CMT2)[95] or autosomal dominant (CMT2P)[96,97]. LRSAM1 is a multifunctional RING finger E3 ubiquitin ligase that plays an important role in endocytosis and in neuronal cells adhesion[98,99]. The first symptoms for CMT2P appear between the second and fifth decade of life and include distal weakness in the lower limbs and in some patients also present in the upper limbs. Other features have been reported in some patients including episodic cramps, bilateral pes cavus, foot drop, absent tendon reflexes, severe loss of sensation in feet and legs and mild loss of sensation on fingertips, sensory and motor dysfunction[95-97]. MNCVs are normal to slightly reduced.
CMT2Q is caused by mutations in the dehydrogenase E1 and transketolase domain-containing 1 (DHTKD1) gene on chromosome 10p14[100]. This gene encodes a mitochondrial 2-oxoglutarate-dehydrogenase-complex-like protein that is involved in the degradation of several amino acids pathways[100,101]. The age of onset is in the first and second decade and the phenotype is typical CMT2, including distal muscle weakness of the lower limbs, decreased or absent tendon reflexes, and mild to moderate sensory loss[100]. MNCVs are normal (> 40 m/s).
Late onset CMT2 is caused by mutations in the methionyl-tRNA synthetase (MARS) gene[102]. This type has recently been identified in one CMT2 family. Clinically it is characterized by late onset (> 50 years old) and a mild CMT2 phenotype[102]. MNCVs studies confirmed an axonal neuropathy.
Dominant intermediate CMT types (DI-CMT) are characterized by intermediate MNCVs (25-45 m/s) and the clinical symptoms are moderate to severe. Electrophysiological and pathological features include both axonal and demyelinating types.
DI-CMTA has been mapped to chromosome 10q24.1-q25.1, but the responsible gene is unknown[103,104]. The phenotype is typical CMT and the MNCVs are moderately reduced[103].
DI-CMTB is caused by mutations in the DNM2 gene that also cause axonal dominant CMT (CMT2M). Patients present with a classic CMT phenotype at the age of 2-50 years old. MNCVs are ranging from 26 to 54 m/s.
DI-CMTC is caused by mutations in the tyrosyl-tRNA synthetase (YARS) gene located on chromosome 1p35.1[105,106]. YARS plays an important role in protein synthesis and in signal transmission from nerves to muscles[106]. The age of onset is between the first and sixth decades with a classic CMT phenotype and numbness in some patients[106]. MNCVs are from 30-40 m/s.
DI-CMTD is caused by mutations in the MPZ gene[10]. MPZ mutations are also associated with CMT1B and CMT2I/2J. DI-CMTD is characterized by a variable severity, distal muscle atrophy, weakness, and sensory loss in the lower and upper limbs. MNCVs are 30-40 m/s.
DI-CMTE is caused by mutations in the inverted formin-2 (IFN2) gene on chromosome 14q32.33[107]. The encoded protein may function in polymerization and depolymerization of actin filaments. INF2 mutations disrupt actin dynamics in peripheral Schwann cells, leading to disturbed myelin formation and maintenance resulting in CMT[107]. The clinical phenotype is typical CMT, including distal muscle weakness and atrophy and distal sensory loss, with focal segmental glomerulonephritis (FSGS) including proteinuria that progresses to renal disease. The first symptoms appear between the first to third decade and MNCVs are normal to moderately reduced (23-45 m/s).
DI-CMTF is caused by mutations in the guanine nucleotide binding protein, beta polypeptide 4 (GNB4) gene[108]. GNB4 protein may play a role in peripheral nerve regeneration. DI-CMTF is characterized by slowly progressive distal muscle atrophy and weakness, and atrophy of the upper and lower limbs, steppage gait and distal sensory loss with decreased reflexes with onset around adolescence. MNCVs are between 16 to 45 m/s.
CMT4 is a demyelinating type of hereditary polyneuropathy with autosomal recessive inheritance[109].
CMT4A is caused by mutations in the GDAP1 gene. Clinically severe motor disturbances and progressive scoliosis are observed[110]. CMT4A is characterized by an early age of onset and reduced MNCVs (25-35 m/s).
CMT4B1 is caused by mutations in the myotubularin-related protein 2 (MTMR2) gene on chromosome 11q22[111,112]. MTMR2 protein has phosphatase activity and influences transcription and cell proliferation[112]. The phenotype of the disease is severe CMT1 and diaphragmatic and facial weakness may occur, as may scoliosis in adult patients[113-115]. Onset is usually in childhood and MNCVs are severely reduced (10-25 m/s).
CMT4B2 is caused by mutations in the set binding factor 2 (SBF2) or myotubularin related protein 13 (MTMR13) gene located on chromosome 11p15[116,117]. The encoded protein is a pseudophosphatase that is involved in membrane trafficking[118]. The clinical phenotype, age of onset and MNCVs are similar to CMT4B1[116,119].
CMT4C is caused by mutations in the SH3 domain and tetratricopeptide repeat domain 2 (SH3TC2) gene that is located on chromosome 5q32[119,120]. SH3TC2 protein is expressed in Schwann cells of the peripheral nerves and localizes to the membrane with a possible function in myelination and in regions of axoglial interactions[121]. CMT4C is characterized by early-onset, distal weakness, foot deformities, walking difficulty, scoliosis and occasionally facial and bulbar weakness, sensorineural deafness and respiratory insufficiency[119,122-124]. MNCVs are reduced (10-35 m/s).
CMT4D (HMSN-L) is caused by mutations in the N-myc downstream-regulated gene 1 (NDRG1) on chromosome 8q24.3[125]. NDRG1 protein appears to play a role in growth arrest and cell differentiation[126]. CMT4C is characterized by distal muscle wasting and atrophy, foot and hand deformities, absent tendon reflexes, and sensory loss. The age of onset is between the first and second decade. Deafness is an invariant feature of the phenotype and usually develops in the third decade.
CMT4E (Congenital Hypomyelinating Neuropathy-CHN) is caused by mutations in the EGR2 gene[37]. EGR2 mutations are also associated with CMT1D. CMT4E is characterized clinically by an early age of onset, hypotonia, absent of reflexes, distal muscle weakness, and extremely reduced MNCVs (< 10 m/s).
CMT4F is caused by mutations in the periaxin (PRX) gene located on chromosome 9q13.2[127-129]. PRX is a Schwann cell protein that plays an important role in axon-glial interactions and is needed for the maintenance of peripheral nerve myelin and regenerating axons[130,131]. CMT4F is characterized, by distal muscle weakness and atrophy, affecting the lower more than the upper limbs, by distal sensory loss and occasionally sensory ataxia. The age at onset is variable, from first to fifth decade and the MNCVs are severely reduced (< 15 m/s)[128,132]. PRX mutations also cause DSS (CMT3D)[128].
CMT4G or CMT-Russe (HSMNR) is caused by mutations in the Hexokinase 1 (HK1) gene that is located on chromosome 10q23.2[133,134]. HK1 protein is involved in the controlled production of ATP and in the regulation of cell survival. Also HK1 is highly expressed in the nervous system and it is involved in NGF-mediated neurite outgrowth[57,134]. Clinically it is characterized by an early age of onset (5-16 years old), distal muscle weakness progressing to severe on lower limbs, prominent sensory loss, hand and foot deformities[133,135]. MNCVs are mildly reduced (30-35 m/s).
CMT4H is caused by mutations in the FYVE, RhoGEF and PH domain containing 4 (FGD4) gene, on chromosome 12p11.21[136,137]. FGD4 (or Frabin) protein is involved in the myelination process, although the molecular mechanisms by which FGD4 mutations cause CMT4H are completely unknown[57,137,138]. CMT4H is characterized by distal muscle weakness and atrophy, areflexia, sensory loss, foot abnormalities and occasionally scoliosis, hypotrophy of thenar and hypothenar muscles[136,139,140].
CMT4J is caused by mutations in the FIG4 homolog, SAC1 lipid phosphatase domain containing (FIG4) gene, located on chromosome 6q21[141]. FIG4 protein has been shown to possess phosphoinositide phosphatase activity and plays a key role in intracellular transport vesicles[141,142]. The clinical phenotype is severe CMT1 with early onset (childhood but sometimes adult onset) and severely reduced MNCVs (< 10 m/s)[3].
AR-CMT2 also called CMT4C is a recessive axonal hereditary neuropathy that is very rare.
AR-CMT2A or CMT2B1 or CMT4C1 is caused by mutations in the lamin A/C (LMNA) gene on chromosome 1q22. Lamin A/C is an intermediate filament protein that forms the nuclear lamina[57]. Lamin proteins are involved in nuclear stability, chromatin structure and gene expression, and also the A-type lamins are important in the protection of the cell from mechanical damage[29,143]. Clinical symptoms usually appear in the second decade (onset between 5-25 years old) with a severe CMT phenotype including proximal muscle involvement although some have a milder phenotype. LMNA mutations have also been associated with other phenotypes including Emery-Dreifuss muscular dystrophy, cardiomyopathy and Dunnigan-type familial partial lipodystrophy[144,145]. MNCV are normal or just slightly reduced.
AR-CMT2B or CMT2B2 or CMT4C3 is caused by mutations in the mediator complex subunit 25 (MED25) gene, also known as ACID1, that is located on chromosome 19q13.33[146-148]. The encoded protein is a component of the Mediator complex that plays a role in gene transcription and also is important in myelination[146,149]. Clinical phenotype is typical CMT2 with late onset, in the third to fifth decade of life, and normal or mildly decreased MNCVs[147,148].
AR-CMT2C or CMT4C2 is caused by mutations in the NEFL gene. The clinical phenotype is severe CMT2 with early onset (< 2 years old) and severely reduced MNCVs (10-25 m/s)[150].
AR-CMT2D or CMT4C4 is caused by mutations in the GDAP1 gene. The clinical phenotype is more severe than CMT2H/K, with early onset and normal MNCVs[76,151,152].
AR-CMT2E is caused by mutations in the LRSAM1 gene with a more severe clinical phenotype than CMT2P and earlier age of onset (first and second decade)[95-97].
CMTX is an X-linked CMT with dominant or recessive inheritance. Clinically heterozygous females are more mildly affected (or asymptomatic) than hemizygous males[153].
CMTX1 is the second commonest form of demyelinating CMT with a frequency of 12% among all CMT patients[16,20]. CMTX1 has both demyelinating and axonal features and is caused by mutations in the gap junction binding 1 (GJB1) gene that is located on chromosome Xq13.1[154]. The encoded protein CX32 (connexin 32) is a transmembrane protein that forms gap junction channels that allow the transfer of small molecules between cells[153]. Clinically males have more severe symptoms, than females. Symptoms in males appear in childhood and later in females[35,155]. MNCVs are slightly reduced, between 30-40 m/s in affected males and 30-50 m/s in affected females[156]
CMTX2 has been mapped to chromosome Xp22.2 and the associated gene mutations are still unknown[157,158]. CMTX2 also has both demyelinating and axonal features and the clinical phenotype is characterized by onset in infancy, weakness and atrophy of the lower limbs, absent reflexes and pes cavus in males. MNCVs are normal to slightly reduced.
CMTX3 has been mapped to chromosome Xq26 and the associated gene mutations are also still unknown[159]. The disease onset is in first and second decade are patients and clinically characterized by progressive weakness of lower limbs and decreased tendon reflexes[157,158]. Electrophysiological findings are compatible with both axonal and demyelination features with MNCVs in the range of 25-57 m/s.
CMTX4 (Cowchock syndrome) is caused by mutations in the apoptosis-inducing factor, mitochondrion-associate 1 (AIFM1) gene on chromosome Xq26.1[160,161]. CMTX4 is characterized by an early childhood onset, distal muscle weakness and atrophy, sensory loss, areflexia and in some patients (approximately 60%) deafness and mental retardation[160]. Heterozygous females are asymptomatic[162]. MNCVs are normal to slightly reduced (33-56 m/s) with decreased sensory conduction velocities.
CMTX5 is caused by mutations in the phosphoribosylpyrophosphate synthetase 1 (PRPS1) gene located in chromosome Xq22.3[163-165]. PRS1 protein is an enzyme critical for nucleotide biosynthesis[57]. Symptoms appear in the first decade of life and the phenotype is characterized by severe peripheral neuropathy with sensorineural deafness, and optic atrophy[165]. MNCVs are normal (43-51 m/s). Heterozygous females are asymptomatic.
CMTX6 is caused by mutations in the pyruvate dehydrogenase kinase isoenzyme 3 (PDK3) gene on chromosome Xp22.11[166]. PDK3 is involved in the regulation of the pyruvate dehydrogenase complex (PDC). PDC catalyzes the oxidation of pyruvate to acetyl-CoA that is a key enzyme involved in the Krebs cycle and lipogenic pathways[166,167]. Disease onset is in the second decade and includes progressive moderate-to-severe wasting below the knees, minimal weakness of the hand muscles, foot deformity, steppage gait, absent ankle reflexes distal lower limb weakness and sensory abnormalities[166]. MNCVs are normal (> 38 m/s).
As outlined above the CMT group of disorders is characterized by a high variability in the clinical phenotype, and great differences exist in the age of the onset, disease progression and severity. There are many types of CMT and a large number of causative genes. As a result of this complexity and the considerable cost of molecular studies, it is useful to establish an algorithm for targeted molecular analysis. Several studies have been published that suggest particular methodologies for performing genetic analysis based on clinical and electrophysiological findings, age of onset of symptoms, family history and relative frequencies of gene mutations[19,20,34,35,145,168,169]. However, some laboratories are currently switching to new screening methods, such as the next generation sequencing (NGS) technology for whole exome and whole genome analysis, slowly replacing the more traditional Sanger sequencing based screening methods. The established flowchart is based on the different CMT types that are determined following the clinical and electrophysiological evaluation of the patient and the existing frequency of causative mutations (Figure 1). PMP22 duplication is the most frequent genetic abnormality and accounts for about 40% of CMT patients, GJB1 for 15%, MFN2 for 10%, MPZ for 5%, PMP22 point mutation for 2.5%; mutations in each of the other CMT genes account for less than 1%[16,19,35,170].
Traditional Sanger sequencing based screening methods are important tools in genetic research. However, the NGS technology already used as a diagnostic tool in some centers will provide new potential capabilities in molecular diagnostic services. NGS is a high throughput technique with low cost and enables sequencing of multiple known and unknown genes in a single run. Additionally, NGS, in combination with other new technologies, such as proteomics and cellular reprogramming may play an important role in the effort to elucidate the pathogenic mechanisms of the disease and lead to the discovery of new therapeutic approaches in CMT and other diseases.
Despite the progress in molecular genetics and the development of new techniques, molecular diagnosis of patients with CMT is still challenging. New genes causing CMT continue to be identified and there exist many more that need to be identified. Increased understanding of the biological processes involved in CMT will enable better understanding of the CMT neuropathy pathogenetic mechanisms and contribute further towards the goal of inventing more effective therapeutic strategies.
P- Reviewers Marco P, Nikolaos P, Yang Z S- Editor Song XX L- Editor A E- Editor Yan JL
| 1. | Charcot JM, Marie , P . Sur une forme particuliere d’atrophie musculaire progressive, souvent familiale, debutante par les pieds et les jambes et atteignant plus tard les mains. Rev Med Parie. 1886;6:97–138. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Tooth H. The Peroneal type of progressive Muscular Atrophy. London: H K Lewis Co. Ltd 1886; . |
| 3. | Barisic N, Claeys KG, Sirotković-Skerlev M, Löfgren A, Nelis E, De Jonghe P, Timmerman V. Charcot-Marie-Tooth disease: a clinico-genetic confrontation. Ann Hum Genet. 2008;72:416-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Skre H. Genetic and clinical aspects of Charcot-Marie-Tooth’s disease. Clin Genet. 1974;6:98-118. [PubMed] |
| 5. | Harding AE, Thomas PK. Genetic aspects of hereditary motor and sensory neuropathy (types I and II). J Med Genet. 1980;17:329-336. [PubMed] |
| 6. | Harding AE, Thomas PK. The clinical features of hereditary motor and sensory neuropathy types I and II. Brain. 1980;103:259-280. [PubMed] |
| 7. | Dyck PJ, Litchy WJ, Minnerath S, Bird TD, Chance PF, Schaid DJ, Aronson AE. Hereditary motor and sensory neuropathy with diaphragm and vocal cord paresis. Ann Neurol. 1994;35:608-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 77] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Bird TD. Hereditary motor-sensory neuropathies. Charcot-Marie-Tooth syndrome. Neurol Clin. 1989;7:9-23. [PubMed] |
| 9. | Berger P, Young P, Suter U. Molecular cell biology of Charcot-Marie-Tooth disease. Neurogenetics. 2002;4:1-15. [PubMed] |
| 10. | Mastaglia FL, Nowak KJ, Stell R, Phillips BA, Edmondston JE, Dorosz SM, Wilton SD, Hallmayer J, Kakulas BA, Laing NG. Novel mutation in the myelin protein zero gene in a family with intermediate hereditary motor and sensory neuropathy. J Neurol Neurosurg Psychiatry. 1999;67:174-179. [PubMed] |
| 11. | Dyck PJ, Lambert EH. Lower motor and primary sensory neuron diseases with peroneal muscular atrophy. I. Neurologic, genetic, and electrophysiologic findings in hereditary polyneuropathies. Arch Neurol. 1968;18:603-618. [PubMed] |
| 12. | Fischbeck KH, ar-Rushdi N, Pericak-Vance M, Rozear M, Roses AD, Fryns JP. X-linked neuropathy: gene localization with DNA probes. Ann Neurol. 1986;20:527-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 58] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Rozear MP, Pericak-Vance MA, Fischbeck K, Stajich JM, Gaskell PC, Krendel DA, Graham DG, Dawson DV, Roses AD. Hereditary motor and sensory neuropathy, X-linked: a half century follow-up. Neurology. 1987;37:1460-1465. [PubMed] |
| 14. | Harding AE, Thomas PK. Autosomal recessive forms of hereditary motor and sensory neuropathy. J Neurol Neurosurg Psychiatry. 1980;43:669-678. [PubMed] |
| 15. | Ben Hamida M, Letaief F, Ben Hamida C, Samoud S. [Peroneal atrophy in Tunisia. Study of 70 cases, pure or associated with other heredodegenerative diseases]. J Neurol Sci. 1981;50:335-356. [PubMed] |
| 16. | Nicolaou P, Zamba-Papanicolaou E, Koutsou P, Kleopa KA, Georghiou A, Hadjigeorgiou G, Papadimitriou A, Kyriakides T, Christodoulou K. Charcot-Marie-Tooth disease in Cyprus: epidemiological, clinical and genetic characteristics. Neuroepidemiology. 2010;35:171-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Patzko A, Shy ME. Charcot-Marie-Tooth disease and related genetic neuropathies. Continuum (Minneap Minn). 2012;18:39-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Juárez P, Palau F. Neural and molecular features on Charcot-Marie-Tooth disease plasticity and therapy. Neural Plast. 2012;2012:171636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Szigeti K, Lupski JR. Charcot-Marie-Tooth disease. Eur J Hum Genet. 2009;17:703-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 152] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 20. | England JD, Gronseth GS, Franklin G, Carter GT, Kinsella LJ, Cohen JA, Asbury AK, Szigeti K, Lupski JR, Latov N. Practice Parameter: evaluation of distal symmetric polyneuropathy: role of autonomic testing, nerve biopsy, and skin biopsy (an evidence-based review). Report of the American Academy of Neurology, American Association of Neuromuscular and Electrodiagnostic Medicine, and American Academy of Physical Medicine and Rehabilitation. Neurology. 2009;72:177-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 196] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 21. | Lupski JR, de Oca-Luna RM, Slaugenhaupt S, Pentao L, Guzzetta V, Trask BJ, Saucedo-Cardenas O, Barker DF, Killian JM, Garcia CA. DNA duplication associated with Charcot-Marie-Tooth disease type 1A. Cell. 1991;66:219-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 925] [Cited by in RCA: 906] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 22. | Raeymaekers P, Timmerman V, Nelis E, De Jonghe P, Hoogendijk JE, Baas F, Barker DF, Martin JJ, De Visser M, Bolhuis PA. Duplication in chromosome 17p11.2 in Charcot-Marie-Tooth neuropathy type 1a (CMT 1a). The HMSN Collaborative Research Group. Neuromuscul Disord. 1991;1:93-97. [PubMed] |
| 23. | Valentijn LJ, Bolhuis PA, Zorn I, Hoogendijk JE, van den Bosch N, Hensels GW, Stanton VP, Housman DE, Fischbeck KH, Ross DA. The peripheral myelin gene PMP-22/GAS-3 is duplicated in Charcot-Marie-Tooth disease type 1A. Nat Genet. 1992;1:166-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 227] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 24. | Nelis E, Van Broeckhoven C, De Jonghe P, Löfgren A, Vandenberghe A, Latour P, Le Guern E, Brice A, Mostacciuolo ML, Schiavon F. Estimation of the mutation frequencies in Charcot-Marie-Tooth disease type 1 and hereditary neuropathy with liability to pressure palsies: a European collaborative study. Eur J Hum Genet. 1996;4:25-33. [PubMed] |
| 25. | Adlkofer K, Frei R, Neuberg DH, Zielasek J, Toyka KV, Suter U. Heterozygous peripheral myelin protein 22-deficient mice are affected by a progressive demyelinating tomaculous neuropathy. J Neurosci. 1997;17:4662-4671. [PubMed] |
| 26. | Martini R, Schachner M. Molecular bases of myelin formation as revealed by investigations on mice deficient in glial cell surface molecules. Glia. 1997;19:298-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Banchs I, Casasnovas C, Albertí A, De Jorge L, Povedano M, Montero J, Martínez-Matos JA, Volpini V. Diagnosis of Charcot-Marie-Tooth disease. J Biomed Biotechnol. 2009;2009:985415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 28. | Hayasaka K, Himoro M, Sato W, Takada G, Uyemura K, Shimizu N, Bird TD, Conneally PM, Chance PF. Charcot-Marie-Tooth neuropathy type 1B is associated with mutations of the myelin P0 gene. Nat Genet. 1993;5:31-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 244] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 29. | Niemann A, Berger P, Suter U. Pathomechanisms of mutant proteins in Charcot-Marie-Tooth disease. Neuromolecular Med. 2006;8:217-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 30. | Nelis E, Haites N, Van Broeckhoven C. Mutations in the peripheral myelin genes and associated genes in inherited peripheral neuropathies. Hum Mutat. 1999;13:11-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 31. | Hayasaka K, Himoro M, Sawaishi Y, Nanao K, Takahashi T, Takada G, Nicholson GA, Ouvrier RA, Tachi N. De novo mutation of the myelin P0 gene in Dejerine-Sottas disease (hereditary motor and sensory neuropathy type III). Nat Genet. 1993;5:266-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 132] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 32. | Reilly MM. Sorting out the inherited neuropathies. Pract Neurol. 2007;7:93-105. [PubMed] |
| 33. | Street VA, Bennett CL, Bird TD, Chance PF. New gene for CMT. J Peripher Nerv Syst. 2003;8:206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 34. | Siskind CE, Panchal S, Smith CO, Feely SM, Dalton JC, Schindler AB, Krajewski KM. A review of genetic counseling for Charcot Marie Tooth disease (CMT). J Genet Couns. 2013;22:422-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 35. | Saporta AS, Sottile SL, Miller LJ, Feely SM, Siskind CE, Shy ME. Charcot-Marie-Tooth disease subtypes and genetic testing strategies. Ann Neurol. 2011;69:22-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 437] [Cited by in RCA: 397] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 36. | Saifi GM, Szigeti K, Wiszniewski W, Shy ME, Krajewski K, Hausmanowa-Petrusewicz I, Kochanski A, Reeser S, Mancias P, Butler I. SIMPLE mutations in Charcot-Marie-Tooth disease and the potential role of its protein product in protein degradation. Hum Mutat. 2005;25:372-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 37. | Warner LE, Mancias P, Butler IJ, McDonald CM, Keppen L, Koob KG, Lupski JR. Mutations in the early growth response 2 (EGR2) gene are associated with hereditary myelinopathies. Nat Genet. 1998;18:382-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 348] [Cited by in RCA: 329] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 38. | Topilko P, Schneider-Maunoury S, Levi G, Baron-Van Evercooren A, Chennoufi AB, Seitanidou T, Babinet C, Charnay P. Krox-20 controls myelination in the peripheral nervous system. Nature. 1994;371:796-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 571] [Cited by in RCA: 617] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 39. | Nagarajan R, Svaren J, Le N, Araki T, Watson M, Milbrandt J. EGR2 mutations in inherited neuropathies dominant-negatively inhibit myelin gene expression. Neuron. 2001;30:355-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 191] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 40. | Timmerman V, De Jonghe P, Ceuterick C, De Vriendt E, Löfgren A, Nelis E, Warner LE, Lupski JR, Martin JJ, Van Broeckhoven C. Novel missense mutation in the early growth response 2 gene associated with Dejerine-Sottas syndrome phenotype. Neurology. 1999;52:1827-1832. [PubMed] |
| 41. | Yoshihara T, Kanda F, Yamamoto M, Ishihara H, Misu K, Hattori N, Chihara K, Sobue G. A novel missense mutation in the early growth response 2 gene associated with late-onset Charcot--Marie--Tooth disease type 1. J Neurol Sci. 2001;184:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 42. | Chung KW, Sunwoo IN, Kim SM, Park KD, Kim WK, Kim TS, Koo H, Cho M, Lee J, Choi BO. Two missense mutations of EGR2 R359W and GJB1 V136A in a Charcot-Marie-Tooth disease family. Neurogenetics. 2005;6:159-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 43. | Boerkoel CF, Takashima H, Bacino CA, Daentl D, Lupski JR. EGR2 mutation R359W causes a spectrum of Dejerine-Sottas neuropathy. Neurogenetics. 2001;3:153-157. [PubMed] |
| 44. | Russo M, Laurá M, Polke JM, Davis MB, Blake J, Brandner S, Hughes RA, Houlden H, Bennett DL, Lunn MP. Variable phenotypes are associated with PMP22 missense mutations. Neuromuscul Disord. 2011;21:106-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 45. | Roa BB, Dyck PJ, Marks HG, Chance PF, Lupski JR. Dejerine-Sottas syndrome associated with point mutation in the peripheral myelin protein 22 (PMP22) gene. Nat Genet. 1993;5:269-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 177] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 46. | Jordanova A, De Jonghe P, Boerkoel CF, Takashima H, De Vriendt E, Ceuterick C, Martin JJ, Butler IJ, Mancias P, Papasozomenos SCh. Mutations in the neurofilament light chain gene (NEFL) cause early onset severe Charcot-Marie-Tooth disease. Brain. 2003;126:590-597. [PubMed] |
| 47. | Auer-Grumbach M, Weger M, Fink-Puches R, Papić L, Fröhlich E, Auer-Grumbach P, El Shabrawi-Caelen L, Schabhüttl M, Windpassinger C, Senderek J. Fibulin-5 mutations link inherited neuropathies, age-related macular degeneration and hyperelastic skin. Brain. 2011;134:1839-1852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 48. | Yanagisawa H, Schluterman MK, Brekken RA. Fibulin-5, an integrin-binding matricellular protein: its function in development and disease. J Cell Commun Signal. 2009;3:337-347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 127] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 49. | Züchner S, De Jonghe P, Jordanova A, Claeys KG, Guergueltcheva V, Cherninkova S, Hamilton SR, Van Stavern G, Krajewski KM, Stajich J. Axonal neuropathy with optic atrophy is caused by mutations in mitofusin 2. Ann Neurol. 2006;59:276-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 265] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 50. | Verhoeven K, Claeys KG, Züchner S, Schröder JM, Weis J, Ceuterick C, Jordanova A, Nelis E, De Vriendt E, Van Hul M. MFN2 mutation distribution and genotype/phenotype correlation in Charcot-Marie-Tooth type 2. Brain. 2006;129:2093-2102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 296] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 51. | Zhao C, Takita J, Tanaka Y, Setou M, Nakagawa T, Takeda S, Yang HW, Terada S, Nakata T, Takei Y. Charcot-Marie-Tooth disease type 2A caused by mutation in a microtubule motor KIF1Bbeta. Cell. 2001;105:587-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 552] [Cited by in RCA: 532] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 52. | Züchner S, Mersiyanova IV, Muglia M, Bissar-Tadmouri N, Rochelle J, Dadali EL, Zappia M, Nelis E, Patitucci A, Senderek J. Mutations in the mitochondrial GTPase mitofusin 2 cause Charcot-Marie-Tooth neuropathy type 2A. Nat Genet. 2004;36:449-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1141] [Cited by in RCA: 1187] [Article Influence: 56.5] [Reference Citation Analysis (0)] |
| 53. | Chung KW, Kim SB, Park KD, Choi KG, Lee JH, Eun HW, Suh JS, Hwang JH, Kim WK, Seo BC. Early onset severe and late-onset mild Charcot-Marie-Tooth disease with mitofusin 2 (MFN2) mutations. Brain. 2006;129:2103-2118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 203] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 54. | Lawson VH, Graham BV, Flanigan KM. Clinical and electrophysiologic features of CMT2A with mutations in the mitofusin 2 gene. Neurology. 2005;65:197-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 127] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 55. | Verhoeven K, De Jonghe P, Coen K, Verpoorten N, Auer-Grumbach M, Kwon JM, FitzPatrick D, Schmedding E, De Vriendt E, Jacobs A. Mutations in the small GTP-ase late endosomal protein RAB7 cause Charcot-Marie-Tooth type 2B neuropathy. Am J Hum Genet. 2003;72:722-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 345] [Cited by in RCA: 394] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 56. | Feng Y, Press B, Wandinger-Ness A. Rab 7: an important regulator of late endocytic membrane traffic. J Cell Biol. 1995;131:1435-1452. [PubMed] |
| 57. | Bucci C, Bakke O, Progida C. Charcot-Marie-Tooth disease and intracellular traffic. Prog Neurobiol. 2012;99:191-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 58. | De Jonghe P, Timmerman V, FitzPatrick D, Spoelders P, Martin JJ, Van Broeckhoven C. Mutilating neuropathic ulcerations in a chromosome 3q13-q22 linked Charcot-Marie-Tooth disease type 2B family. J Neurol Neurosurg Psychiatry. 1997;62:570-573. [PubMed] |
| 59. | Auer-Grumbach M, De Jonghe P, Wagner K, Verhoeven K, Hartung HP, Timmerman V. Phenotype-genotype correlations in a CMT2B family with refined 3q13-q22 locus. Neurology. 2000;55:1552-1557. [PubMed] |
| 60. | Klein CJ, Cunningham JM, Atkinson EJ, Schaid DJ, Hebbring SJ, Anderson SA, Klein DM, Dyck PJ, Litchy WJ, Thibodeau SN. The gene for HMSN2C maps to 12q23-24: a region of neuromuscular disorders. Neurology. 2003;60:1151-1156. [PubMed] |
| 61. | Landouré G, Zdebik AA, Martinez TL, Burnett BG, Stanescu HC, Inada H, Shi Y, Taye AA, Kong L, Munns CH. Mutations in TRPV4 cause Charcot-Marie-Tooth disease type 2C. Nat Genet. 2010;42:170-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 233] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 62. | Chen DH, Sul Y, Weiss M, Hillel A, Lipe H, Wolff J, Matsushita M, Raskind W, Bird T. CMT2C with vocal cord paresis associated with short stature and mutations in the TRPV4 gene. Neurology. 2010;75:1968-1975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 63. | Ionasescu V, Searby C, Sheffield VC, Roklina T, Nishimura D, Ionasescu R. Autosomal dominant Charcot-Marie-Tooth axonal neuropathy mapped on chromosome 7p (CMT2D). Hum Mol Genet. 1996;5:1373-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 81] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 64. | Antonellis A, Ellsworth RE, Sambuughin N, Puls I, Abel A, Lee-Lin SQ, Jordanova A, Kremensky I, Christodoulou K, Middleton LT. Glycyl tRNA synthetase mutations in Charcot-Marie-Tooth disease type 2D and distal spinal muscular atrophy type V. Am J Hum Genet. 2003;72:1293-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 65. | Sivakumar K, Kyriakides T, Puls I, Nicholson GA, Funalot B, Antonellis A, Sambuughin N, Christodoulou K, Beggs JL, Zamba-Papanicolaou E. Phenotypic spectrum of disorders associated with glycyl-tRNA synthetase mutations. Brain. 2005;128:2304-2314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 101] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 66. | Mersiyanova IV, Perepelov AV, Polyakov AV, Sitnikov VF, Dadali EL, Oparin RB, Petrin AN, Evgrafov OV. A new variant of Charcot-Marie-Tooth disease type 2 is probably the result of a mutation in the neurofilament-light gene. Am J Hum Genet. 2000;67:37-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 294] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 67. | Georgiou DM, Zidar J, Korosec M, Middleton LT, Kyriakides T, Christodoulou K. A novel NF-L mutation Pro22Ser is associated with CMT2 in a large Slovenian family. Neurogenetics. 2002;4:93-96. [PubMed] |
| 68. | Ismailov SM, Fedotov VP, Dadali EL, Polyakov AV, Van Broeckhoven C, Ivanov VI, De Jonghe P, Timmerman V, Evgrafov OV. A new locus for autosomal dominant Charcot-Marie-Tooth disease type 2 (CMT2F) maps to chromosome 7q11-q21. Eur J Hum Genet. 2001;9:646-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 69. | Evgrafov OV, Mersiyanova I, Irobi J, Van Den Bosch L, Dierick I, Leung CL, Schagina O, Verpoorten N, Van Impe K, Fedotov V. Mutant small heat-shock protein 27 causes axonal Charcot-Marie-Tooth disease and distal hereditary motor neuropathy. Nat Genet. 2004;36:602-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 443] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 70. | Zhai J, Lin H, Julien JP, Schlaepfer WW. Disruption of neurofilament network with aggregation of light neurofilament protein: a common pathway leading to motor neuron degeneration due to Charcot-Marie-Tooth disease-linked mutations in NFL and HSPB1. Hum Mol Genet. 2007;16:3103-3116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 94] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 71. | Houlden H, Laura M, Wavrant-De Vrièze F, Blake J, Wood N, Reilly MM. Mutations in the HSP27 (HSPB1) gene cause dominant, recessive, and sporadic distal HMN/CMT type 2. Neurology. 2008;71:1660-1668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 145] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 72. | Chung KW, Kim SB, Cho SY, Hwang SJ, Park SW, Kang SH, Kim J, Yoo JH, Choi BO. Distal hereditary motor neuropathy in Korean patients with a small heat shock protein 27 mutation. Exp Mol Med. 2008;40:304-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 73. | Berciano J, Combarros O, Figols J, Calleja J, Cabello A, Silos I, Coria F. Hereditary motor and sensory neuropathy type II. Clinicopathological study of a family. Brain. 1986;109:897-914. [PubMed] |
| 74. | Nelis E, Berciano J, Verpoorten N, Coen K, Dierick I, Van Gerwen V, Combarros O, De Jonghe P, Timmerman V. Autosomal dominant axonal Charcot-Marie-Tooth disease type 2 (CMT2G) maps to chromosome 12q12-q13.3. J Med Genet. 2004;41:193-197. [PubMed] |
| 75. | Barhoumi C, Amouri R, Ben Hamida C, Ben Hamida M, Machghoul S, Gueddiche M, Hentati F. Linkage of a new locus for autosomal recessive axonal form of Charcot-Marie-Tooth disease to chromosome 8q21.3. Neuromuscul Disord. 2001;11:27-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 76. | Cuesta A, Pedrola L, Sevilla T, García-Planells J, Chumillas MJ, Mayordomo F, LeGuern E, Marín I, Vílchez JJ, Palau F. The gene encoding ganglioside-induced differentiation-associated protein 1 is mutated in axonal Charcot-Marie-Tooth type 4A disease. Nat Genet. 2002;30:22-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 242] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 77. | Boerkoel CF, Takashima H, Garcia CA, Olney RK, Johnson J, Berry K, Russo P, Kennedy S, Teebi AS, Scavina M. Charcot-Marie-Tooth disease and related neuropathies: mutation distribution and genotype-phenotype correlation. Ann Neurol. 2002;51:190-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 180] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 78. | Baxter RV, Ben Othmane K, Rochelle JM, Stajich JE, Hulette C, Dew-Knight S, Hentati F, Ben Hamida M, Bel S, Stenger JE. Ganglioside-induced differentiation-associated protein-1 is mutant in Charcot-Marie-Tooth disease type 4A/8q21. Nat Genet. 2002;30:21-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 258] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 79. | Claramunt R, Pedrola L, Sevilla T, López de Munain A, Berciano J, Cuesta A, Sánchez-Navarro B, Millán JM, Saifi GM, Lupski JR. Genetics of Charcot-Marie-Tooth disease type 4A: mutations, inheritance, phenotypic variability, and founder effect. J Med Genet. 2005;42:358-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 112] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 80. | Marrosu MG, Vaccargiu S, Marrosu G, Vannelli A, Cianchetti C, Muntoni F. Charcot-Marie-Tooth disease type 2 associated with mutation of the myelin protein zero gene. Neurology. 1998;50:1397-1401. [PubMed] |
| 81. | De Jonghe P, Timmerman V, Ceuterick C, Nelis E, De Vriendt E, Löfgren A, Vercruyssen A, Verellen C, Van Maldergem L, Martin JJ. The Thr124Met mutation in the peripheral myelin protein zero (MPZ) gene is associated with a clinically distinct Charcot-Marie-Tooth phenotype. Brain. 1999;122:281-290. [PubMed] |
| 82. | Tang BS, Luo W, Xia K, Xiao JF, Jiang H, Shen L, Tang JG, Zhao GH, Cai F, Pan Q. A new locus for autosomal dominant Charcot-Marie-Tooth disease type 2 (CMT2L) maps to chromosome 12q24. Hum Genet. 2004;114:527-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 83. | Tang BS, Zhao GH, Luo W, Xia K, Cai F, Pan Q, Zhang RX, Zhang FF, Liu XM, Chen B. Small heat-shock protein 22 mutated in autosomal dominant Charcot-Marie-Tooth disease type 2L. Hum Genet. 2005;116:222-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 138] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 84. | Züchner S, Noureddine M, Kennerson M, Verhoeven K, Claeys K, De Jonghe P, Merory J, Oliveira SA, Speer MC, Stenger JE. Mutations in the pleckstrin homology domain of dynamin 2 cause dominant intermediate Charcot-Marie-Tooth disease. Nat Genet. 2005;37:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 265] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 85. | Kennerson ML, Zhu D, Gardner RJ, Storey E, Merory J, Robertson SP, Nicholson GA. Dominant intermediate Charcot-Marie-Tooth neuropathy maps to chromosome 19p12-p13.2. Am J Hum Genet. 2001;69:883-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 86. | McNiven MA. Dynamin: a molecular motor with pinchase action. Cell. 1998;94:151-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 145] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 87. | Fabrizi GM, Ferrarini M, Cavallaro T, Cabrini I, Cerini R, Bertolasi L, Rizzuto N. Two novel mutations in dynamin-2 cause axonal Charcot-Marie-Tooth disease. Neurology. 2007;69:291-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 88. | Gallardo E, Claeys KG, Nelis E, García A, Canga A, Combarros O, Timmerman V, De Jonghe P, Berciano J. Magnetic resonance imaging findings of leg musculature in Charcot-Marie-Tooth disease type 2 due to dynamin 2 mutation. J Neurol. 2008;255:986-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 89. | Latour P, Thauvin-Robinet C, Baudelet-Méry C, Soichot P, Cusin V, Faivre L, Locatelli MC, Mayençon M, Sarcey A, Broussolle E, Camu W, David A, Rousson R. A major determinant for binding and aminoacylation of tRNA(Ala) in cytoplasmic Alanyl-tRNA synthetase is mutated in dominant axonal Charcot-Marie-Tooth disease. Am J Hum Genet. 2010;86:77-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 186] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 90. | Schimmel P. Aminoacyl tRNA synthetases: general scheme of structure-function relationships in the polypeptides and recognition of transfer RNAs. Annu Rev Biochem. 1987;56:125-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 439] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 91. | Lin KP, Soong BW, Yang CC, Huang LW, Chang MH, Lee IH, Antonellis A, Lee YC. The mutational spectrum in a cohort of Charcot-Marie-Tooth disease type 2 among the Han Chinese in Taiwan. PLoS One. 2011;6:e29393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 92. | McLaughlin HM, Sakaguchi R, Giblin W, Wilson TE, Biesecker L, Lupski JR, Talbot K, Vance JM, Züchner S, Lee YC. A recurrent loss-of-function alanyl-tRNA synthetase (AARS) mutation in patients with Charcot-Marie-Tooth disease type 2N (CMT2N). Hum Mutat. 2012;33:244-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 93] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 93. | Weedon MN, Hastings R, Caswell R, Xie W, Paszkiewicz K, Antoniadi T, Williams M, King C, Greenhalgh L, Newbury-Ecob R. Exome sequencing identifies a DYNC1H1 mutation in a large pedigree with dominant axonal Charcot-Marie-Tooth disease. Am J Hum Genet. 2011;89:308-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 208] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 94. | Vaisberg EA, Koonce MP, McIntosh JR. Cytoplasmic dynein plays a role in mammalian mitotic spindle formation. J Cell Biol. 1993;123:849-858. [PubMed] |
| 95. | Guernsey DL, Jiang H, Bedard K, Evans SC, Ferguson M, Matsuoka M, Macgillivray C, Nightingale M, Perry S, Rideout AL. Mutation in the gene encoding ubiquitin ligase LRSAM1 in patients with Charcot-Marie-Tooth disease. PLoS Genet. 2010;6:pii: e1001081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 96. | Weterman MA, Sorrentino V, Kasher PR, Jakobs ME, van Engelen BG, Fluiter K, de Wissel MB, Sizarov A, Nürnberg G, Nürnberg P. A frameshift mutation in LRSAM1 is responsible for a dominant hereditary polyneuropathy. Hum Mol Genet. 2012;21:358-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 97. | Nicolaou P, Cianchetti C, Minaidou A, Marrosu G, Zamba-Papanicolaou E, Middleton L, Christodoulou K. A novel LRSAM1 mutation is associated with autosomal dominant axonal Charcot-Marie-Tooth disease. Eur J Hum Genet. 2013;21:190-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 98. | Li B, Su Y, Ryder J, Yan L, Na S, Ni B. RIFLE: a novel ring zinc finger-leucine-rich repeat containing protein, regulates select cell adhesion molecules in PC12 cells. J Cell Biochem. 2003;90:1224-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 99. | Amit I, Yakir L, Katz M, Zwang Y, Marmor MD, Citri A, Shtiegman K, Alroy I, Tuvia S, Reiss Y. Tal, a Tsg101-specific E3 ubiquitin ligase, regulates receptor endocytosis and retrovirus budding. Genes Dev. 2004;18:1737-1752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 127] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 100. | Xu WY, Gu MM, Sun LH, Guo WT, Zhu HB, Ma JF, Yuan WT, Kuang Y, Ji BJ, Wu XL. A nonsense mutation in DHTKD1 causes Charcot-Marie-Tooth disease type 2 in a large Chinese pedigree. Am J Hum Genet. 2012;91:1088-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 101. | Danhauser K, Sauer SW, Haack TB, Wieland T, Staufner C, Graf E, Zschocke J, Strom TM, Traub T, Okun JG. DHTKD1 mutations cause 2-aminoadipic and 2-oxoadipic aciduria. Am J Hum Genet. 2012;91:1082-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 102. | Gonzalez M, McLaughlin H, Houlden H, Guo M, Yo-Tsen L, Hadjivassilious M, Speziani F, Yang XL, Antonellis A, Reilly MM, Züchner S; Inherited Neuropathy Consortium (INC). Exome sequencing identifies a significant variant in methionyl-tRNA synthetase (MARS) in a family with late-onset CMT2. J Neurol Neurosurg Psychiatry. 2013;Jun 1; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 115] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 103. | Verhoeven K, Villanova M, Rossi A, Malandrini A, De Jonghe P, Timmerman V. Localization of the gene for the intermediate form of Charcot-Marie-Tooth to chromosome 10q24.1-q25.1. Am J Hum Genet. 2001;69:889-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 104. | Villanova M, Timmerman V, De Jonghe P, Malandrini A, Rizzuto N, Van Broeckhoven C, Guazzi G, Rossi A. Charcot-Marie-Tooth disease: an intermediate form. Neuromuscul Disord. 1998;8:392-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 105. | Jordanova A, Thomas FP, Guergueltcheva V, Tournev I, Gondim FA, Ishpekova B, De Vriendt E, Jacobs A, Litvinenko I, Ivanova N. Dominant intermediate Charcot-Marie-Tooth type C maps to chromosome 1p34-p35. Am J Hum Genet. 2003;73:1423-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 106. | Jordanova A, Irobi J, Thomas FP, Van Dijck P, Meerschaert K, Dewil M, Dierick I, Jacobs A, De Vriendt E, Guergueltcheva V. Disrupted function and axonal distribution of mutant tyrosyl-tRNA synthetase in dominant intermediate Charcot-Marie-Tooth neuropathy. Nat Genet. 2006;38:197-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 299] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 107. | Boyer O, Nevo F, Plaisier E, Funalot B, Gribouval O, Benoit G, Cong EH, Arrondel C, Tête MJ, Montjean R. INF2 mutations in Charcot-Marie-Tooth disease with glomerulopathy. N Engl J Med. 2011;365:2377-2388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 210] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 108. | Soong BW, Huang YH, Tsai PC, Huang CC, Pan HC, Lu YC, Chien HJ, Liu TT, Chang MH, Lin KP. Exome sequencing identifies GNB4 mutations as a cause of dominant intermediate Charcot-Marie-Tooth disease. Am J Hum Genet. 2013;92:422-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 109. | Kuhlenbäumer G, Young P, Hünermund G, Ringelstein B, Stögbauer F. Clinical features and molecular genetics of hereditary peripheral neuropathies. J Neurol. 2002;249:1629-1650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 39] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 110. | Ammar N, Nelis E, Merlini L, Barisić N, Amouri R, Ceuterick C, Martin JJ, Timmerman V, Hentati F, De Jonghe P. Identification of novel GDAP1 mutations causing autosomal recessive Charcot-Marie-Tooth disease. Neuromuscul Disord. 2003;13:720-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 111. | Bolino A, Levy ER, Muglia M, Conforti FL, LeGuern E, Salih MA, Georgiou DM, Christodoulou RK, Hausmanowa-Petrusewicz I, Mandich P. Genetic refinement and physical mapping of the CMT4B gene on chromosome 11q22. Genomics. 2000;63:271-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 112. | Bolino A, Muglia M, Conforti FL, LeGuern E, Salih MA, Georgiou DM, Christodoulou K, Hausmanowa-Petrusewicz I, Mandich P, Schenone A. Charcot-Marie-Tooth type 4B is caused by mutations in the gene encoding myotubularin-related protein-2. Nat Genet. 2000;25:17-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 336] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 113. | Tyson J, Ellis D, Fairbrother U, King RH, Muntoni F, Jacobs J, Malcolm S, Harding AE, Thomas PK. Hereditary demyelinating neuropathy of infancy. A genetically complex syndrome. Brain. 1997;120:47-63. [PubMed] |
| 114. | Verny C, Ravisé N, Leutenegger AL, Pouplard F, Dubourg O, Tardieu S, Dubas F, Brice A, Genin E, LeGuern E. Coincidence of two genetic forms of Charcot-Marie-Tooth disease in a single family. Neurology. 2004;63:1527-1529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 115. | Parman Y, Battaloglu E, Baris I, Bilir B, Poyraz M, Bissar-Tadmouri N, Williams A, Ammar N, Nelis E, Timmerman V. Clinicopathological and genetic study of early-onset demyelinating neuropathy. Brain. 2004;127:2540-2550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 116. | Azzedine H, Bolino A, Taïeb T, Birouk N, Di Duca M, Bouhouche A, Benamou S, Mrabet A, Hammadouche T, Chkili T. Mutations in MTMR13, a new pseudophosphatase homologue of MTMR2 and Sbf1, in two families with an autosomal recessive demyelinating form of Charcot-Marie-Tooth disease associated with early-onset glaucoma. Am J Hum Genet. 2003;72:1141-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 117. | Senderek J, Bergmann C, Weber S, Ketelsen UP, Schorle H, Rudnik-Schöneborn S, Büttner R, Buchheim E, Zerres K. Mutation of the SBF2 gene, encoding a novel member of the myotubularin family, in Charcot-Marie-Tooth neuropathy type 4B2/11p15. Hum Mol Genet. 2003;12:349-356. [PubMed] |
| 118. | Azzedine H, Senderek J, Rivolta C, Chrast R. Molecular genetics of charcot-marie-tooth disease: from genes to genomes. Mol Syndromol. 2012;3:204-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 119. | Senderek J, Bergmann C, Stendel C, Kirfel J, Verpoorten N, De Jonghe P, Timmerman V, Chrast R, Verheijen MH, Lemke G. Mutations in a gene encoding a novel SH3/TPR domain protein cause autosomal recessive Charcot-Marie-Tooth type 4C neuropathy. Am J Hum Genet. 2003;73:1106-1119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 146] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 120. | LeGuern E, Guilbot A, Kessali M, Ravisé N, Tassin J, Maisonobe T, Grid D, Brice A. Homozygosity mapping of an autosomal recessive form of demyelinating Charcot-Marie-Tooth disease to chromosome 5q23-q33. Hum Mol Genet. 1996;5:1685-1688. [PubMed] |
| 121. | Arnaud E, Zenker J, de Preux Charles AS, Stendel C, Roos A, Médard JJ, Tricaud N, Kleine H, Luscher B, Weis J. SH3TC2/KIAA1985 protein is required for proper myelination and the integrity of the node of Ranvier in the peripheral nervous system. Proc Natl Acad Sci U S A. 2009;106:17528-17533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 122. | Azzedine H, Ravisé N, Verny C, Gabrëels-Festen A, Lammens M, Grid D, Vallat JM, Durosier G, Senderek J, Nouioua S. Spine deformities in Charcot-Marie-Tooth 4C caused by SH3TC2 gene mutations. Neurology. 2006;67:602-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 74] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 123. | Colomer J, Gooding R, Angelicheva D, King RH, Guillén-Navarro E, Parman Y, Nascimento A, Conill J, Kalaydjieva L. Clinical spectrum of CMT4C disease in patients homozygous for the p.Arg1109X mutation in SH3TC2. Neuromuscul Disord. 2006;16:449-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 124. | Gooding R, Colomer J, King R, Angelicheva D, Marns L, Parman Y, Chandler D, Bertranpetit J, Kalaydjieva L. A novel Gypsy founder mutation, p.Arg1109X in the CMT4C gene, causes variable peripheral neuropathy phenotypes. J Med Genet. 2005;42:e69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 125. | Kalaydjieva L, Gresham D, Gooding R, Heather L, Baas F, de Jonge R, Blechschmidt K, Angelicheva D, Chandler D, Worsley P. N-myc downstream-regulated gene 1 is mutated in hereditary motor and sensory neuropathy-Lom. Am J Hum Genet. 2000;67:47-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 262] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 126. | Kalaydjieva L, Hallmayer J, Chandler D, Savov A, Nikolova A, Angelicheva D, King RH, Ishpekova B, Honeyman K, Calafell F. Gene mapping in Gypsies identifies a novel demyelinating neuropathy on chromosome 8q24. Nat Genet. 1996;14:214-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 124] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 127. | Delague V, Bareil C, Tuffery S, Bouvagnet P, Chouery E, Koussa S, Maisonobe T, Loiselet J, Mégarbané A, Claustres M. Mapping of a new locus for autosomal recessive demyelinating Charcot-Marie-Tooth disease to 19q13.1-13.3 in a large consanguineous Lebanese family: exclusion of MAG as a candidate gene. Am J Hum Genet. 2000;67:236-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 128. | Boerkoel CF, Takashima H, Stankiewicz P, Garcia CA, Leber SM, Rhee-Morris L, Lupski JR. Periaxin mutations cause recessive Dejerine-Sottas neuropathy. Am J Hum Genet. 2001;68:325-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 129. | Guilbot A, Williams A, Ravisé N, Verny C, Brice A, Sherman DL, Brophy PJ, LeGuern E, Delague V, Bareil C. A mutation in periaxin is responsible for CMT4F, an autosomal recessive form of Charcot-Marie-Tooth disease. Hum Mol Genet. 2001;10:415-421. [PubMed] |
| 130. | Gillespie CS, Sherman DL, Blair GE, Brophy PJ. Periaxin, a novel protein of myelinating Schwann cells with a possible role in axonal ensheathment. Neuron. 1994;12:497-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 125] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 131. | Scherer SS, Xu YT, Bannerman PG, Sherman DL, Brophy PJ. Periaxin expression in myelinating Schwann cells: modulation by axon-glial interactions and polarized localization during development. Development. 1995;121:4265-4273. [PubMed] |
| 132. | Marchesi C, Milani M, Morbin M, Cesani M, Lauria G, Scaioli V, Piccolo G, Fabrizi GM, Cavallaro T, Taroni F. Four novel cases of periaxin-related neuropathy and review of the literature. Neurology. 2010;75:1830-1838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 133. | Thomas PK, Kalaydjieva L, Youl B, Rogers T, Angelicheva D, King RH, Guergueltcheva V, Colomer J, Lupu C, Corches A. Hereditary motor and sensory neuropathy-russe: new autosomal recessive neuropathy in Balkan Gypsies. Ann Neurol. 2001;50:452-457. [PubMed] |
| 134. | Hantke J, Chandler D, King R, Wanders RJ, Angelicheva D, Tournev I, McNamara E, Kwa M, Guergueltcheva V, Kaneva R. A mutation in an alternative untranslated exon of hexokinase 1 associated with hereditary motor and sensory neuropathy -- Russe (HMSNR). Eur J Hum Genet. 2009;17:1606-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 135. | Sevilla T, Martínez-Rubio D, Márquez C, Paradas C, Colomer J, Jaijo T, Millán JM, Palau F, Espinós C. Genetics of the Charcot-Marie-Tooth disease in the Spanish Gypsy population: the hereditary motor and sensory neuropathy-Russe in depth. Clin Genet. 2013;83:565-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 136. | De Sandre-Giovannoli A, Delague V, Hamadouche T, Chaouch M, Krahn M, Boccaccio I, Maisonobe T, Chouery E, Jabbour R, Atweh S. Homozygosity mapping of autosomal recessive demyelinating Charcot-Marie-Tooth neuropathy (CMT4H) to a novel locus on chromosome 12p11.21-q13.11. J Med Genet. 2005;42:260-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 137. | Delague V, Jacquier A, Hamadouche T, Poitelon Y, Baudot C, Boccaccio I, Chouery E, Chaouch M, Kassouri N, Jabbour R. Mutations in FGD4 encoding the Rho GDP/GTP exchange factor FRABIN cause autosomal recessive Charcot-Marie-Tooth type 4H. Am J Hum Genet. 2007;81:1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 138. | Stendel C, Roos A, Deconinck T, Pereira J, Castagner F, Niemann A, Kirschner J, Korinthenberg R, Ketelsen UP, Battaloglu E. Peripheral nerve demyelination caused by a mutant Rho GTPase guanine nucleotide exchange factor, frabin/FGD4. Am J Hum Genet. 2007;81:158-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 106] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 139. | Houlden H, Hammans S, Katifi H, Reilly MM. A novel Frabin (FGD4) nonsense mutation p.R275X associated with phenotypic variability in CMT4H. Neurology. 2009;72:617-620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 140. | Fabrizi GM, Taioli F, Cavallaro T, Ferrari S, Bertolasi L, Casarotto M, Rizzuto N, Deconinck T, Timmerman V, De Jonghe P. Further evidence that mutations in FGD4/frabin cause Charcot-Marie-Tooth disease type 4H. Neurology. 2009;72:1160-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 141. | Chow CY, Zhang Y, Dowling JJ, Jin N, Adamska M, Shiga K, Szigeti K, Shy ME, Li J, Zhang X. Mutation of FIG4 causes neurodegeneration in the pale tremor mouse and patients with CMT4J. Nature. 2007;448:68-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 407] [Cited by in RCA: 397] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 142. | Zhang X, Chow CY, Sahenk Z, Shy ME, Meisler MH, Li J. Mutation of FIG4 causes a rapidly progressive, asymmetric neuronal degeneration. Brain. 2008;131:1990-2001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 117] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 143. | Hutchison CJ, Worman HJ. A-type lamins: guardians of the soma? Nat Cell Biol. 2004;6:1062-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 169] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 144. | De Sandre-Giovannoli A, Chaouch M, Kozlov S, Vallat JM, Tazir M, Kassouri N, Szepetowski P, Hammadouche T, Vandenberghe A, Stewart CL. Homozygous defects in LMNA, encoding lamin A/C nuclear-envelope proteins, cause autosomal recessive axonal neuropathy in human (Charcot-Marie-Tooth disorder type 2) and mouse. Am J Hum Genet. 2002;70:726-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 145. | Reilly MM, Murphy SM, Laurá M. Charcot-Marie-Tooth disease. J Peripher Nerv Syst. 2011;16:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 173] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 146. | Leal A, Huehne K, Bauer F, Sticht H, Berger P, Suter U, Morera B, Del Valle G, Lupski JR, Ekici A. Identification of the variant Ala335Val of MED25 as responsible for CMT2B2: molecular data, functional studies of the SH3 recognition motif and correlation between wild-type MED25 and PMP22 RNA levels in CMT1A animal models. Neurogenetics. 2009;10:275-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 147. | Leal A, Morera B, Del Valle G D, Kayser C, Berghoff M, Villegas R, Hernández E, Méndez M, Hennies HC, Neundörfer B. A second locus for an axonal form of autosomal recessive Charcot-Marie-Tooth disease maps to chromosome 19q13.3. Am J Hum Genet. 2001;68:269-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 148. | Berghoff C, Berghoff M, Leal A, Morera B, Barrantes R, Reis A, Neundörfer B, Rautenstrauss B, Del Valle G, Heuss D. Clinical and electrophysiological characteristics of autosomal recessive axonal Charcot-Marie-Tooth disease (ARCMT2B) that maps to chromosome 19q13.3. Neuromuscul Disord. 2004;14:301-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 149. | Rana R, Surapureddi S, Kam W, Ferguson S, Goldstein JA. Med25 is required for RNA polymerase II recruitment to specific promoters, thus regulating xenobiotic and lipid metabolism in human liver. Mol Cell Biol. 2011;31:466-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 150. | Yum SW, Zhang J, Mo K, Li J, Scherer SS. A novel recessive Nefl mutation causes a severe, early-onset axonal neuropathy. Ann Neurol. 2009;66:759-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 89] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 151. | Birouk N, Azzedine H, Dubourg O, Muriel MP, Benomar A, Hamadouche T, Maisonobe T, Ouazzani R, Brice A, Yahyaoui M. Phenotypical features of a Moroccan family with autosomal recessive Charcot-Marie-Tooth disease associated with the S194X mutation in the GDAP1 gene. Arch Neurol. 2003;60:598-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 152. | Bernard R, De Sandre-Giovannoli A, Delague V, Lévy N. Molecular genetics of autosomal-recessive axonal Charcot-Marie-Tooth neuropathies. Neuromolecular Med. 2006;8:87-106. [PubMed] |
| 153. | Bergoffen J, Scherer SS, Wang S, Scott MO, Bone LJ, Paul DL, Chen K, Lensch MW, Chance PF, Fischbeck KH. Connexin mutations in X-linked Charcot-Marie-Tooth disease. Science. 1993;262:2039-2042. [PubMed] |
| 154. | Gal A, Mücke J, Theile H, Wieacker PF, Ropers HH, Wienker TF. X-linked dominant Charcot-Marie-Tooth disease: suggestion of linkage with a cloned DNA sequence from the proximal Xq. Hum Genet. 1985;70:38-42. [PubMed] |
| 155. | Siskind CE, Murphy SM, Ovens R, Polke J, Reilly MM, Shy ME. Phenotype expression in women with CMT1X. J Peripher Nerv Syst. 2011;16:102-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 156. | Kleopa KA, Scherer SS. Molecular genetics of X-linked Charcot-Marie-Tooth disease. Neuromolecular Med. 2006;8:107-122. [PubMed] |
| 157. | Ionasescu VV, Trofatter J, Haines JL, Summers AM, Ionasescu R, Searby C. Heterogeneity in X-linked recessive Charcot-Marie-Tooth neuropathy. Am J Hum Genet. 1991;48:1075-1083. [PubMed] |
| 158. | Ionasescu VV, Trofatter J, Haines JL, Summers AM, Ionasescu R, Searby C. X-linked recessive Charcot-Marie-Tooth neuropathy: clinical and genetic study. Muscle Nerve. 1992;15:368-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 159. | Huttner IG, Kennerson ML, Reddel SW, Radovanovic D, Nicholson GA. Proof of genetic heterogeneity in X-linked Charcot-Marie-Tooth disease. Neurology. 2006;67:2016-2021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 160. | Cowchock FS, Duckett SW, Streletz LJ, Graziani LJ, Jackson LG. X-linked motor-sensory neuropathy type-II with deafness and mental retardation: a new disorder. Am J Med Genet. 1985;20:307-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 58] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 161. | Rinaldi C, Grunseich C, Sevrioukova IF, Schindler A, Horkayne-Szakaly I, Lamperti C, Landouré G, Kennerson ML, Burnett BG, Bönnemann C. Cowchock syndrome is associated with a mutation in apoptosis-inducing factor. Am J Hum Genet. 2012;91:1095-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 115] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 162. | Priest JM, Fischbeck KH, Nouri N, Keats BJ. A locus for axonal motor-sensory neuropathy with deafness and mental retardation maps to Xq24-q26. Genomics. 1995;29:409-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 163. | Pauli RM. Sensorineural deafness and peripheral neuropathy. Clin Genet. 1984;26:383-384. [PubMed] |
| 164. | Kim HJ, Hong SH, Ki CS, Kim BJ, Shim JS, Cho SH, Park JH, Kim JW. A novel locus for X-linked recessive CMT with deafness and optic neuropathy maps to Xq21.32-q24. Neurology. 2005;64:1964-1967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 165. | Kim HJ, Sohn KM, Shy ME, Krajewski KM, Hwang M, Park JH, Jang SY, Won HH, Choi BO, Hong SH. Mutations in PRPS1, which encodes the phosphoribosyl pyrophosphate synthetase enzyme critical for nucleotide biosynthesis, cause hereditary peripheral neuropathy with hearing loss and optic neuropathy (cmtx5). Am J Hum Genet. 2007;81:552-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 96] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 166. | Kennerson ML, Yiu EM, Chuang DT, Kidambi A, Tso SC, Ly C, Chaudhry R, Drew AP, Rance G, Delatycki MB. A new locus for X-linked dominant Charcot-Marie-Tooth disease (CMTX6) is caused by mutations in the pyruvate dehydrogenase kinase isoenzyme 3 (PDK3) gene. Hum Mol Genet. 2013;22:1404-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 167. | Gudi R, Bowker-Kinley MM, Kedishvili NY, Zhao Y, Popov KM. Diversity of the pyruvate dehydrogenase kinase gene family in humans. J Biol Chem. 1995;270:28989-28994. [PubMed] |
| 168. | Saporta MA, Shy ME. Inherited peripheral neuropathies. Neurol Clin. 2013;31:597-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 169. | Berciano J, Sevilla T, Casasnovas C, Sivera R, Vílchez JJ, Infante J, Ramón C, Pelayo-Negro AL, Illa I. [Guidelines for molecular diagnosis of Charcot-Marie-Tooth disease]. Neurologia. 2012;27:169-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 170. | Murphy SM, Laura M, Fawcett K, Pandraud A, Liu YT, Davidson GL, Rossor AM, Polke JM, Castleman V, Manji H. Charcot-Marie-Tooth disease: frequency of genetic subtypes and guidelines for genetic testing. J Neurol Neurosurg Psychiatry. 2012;83:706-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 273] [Article Influence: 21.0] [Reference Citation Analysis (0)] |