Peer-review started: June 23, 2021
First decision: July 31, 2021
Revised: August 1, 2021
Accepted: January 29, 2022
Article in press: January 29, 2022
Published online: February 25, 2022
Processing time: 244 Days and 18 Hours
Previous cases that have been stated in this article have displayed that around 1% to 7% of patients that have been treated with chemotherapy for acute promyelocytic leukemia developed myelodysplastic syndrome or acute myeloid leukemia. One can see that’s why this case presentation of a 60-year-old man that had a good response to acute promyelocytic leukemia treatment, that later presented with a central nervous system recurrence of acute promyelocytic leukemia and acquired sideroblastic anemia (a form of myelodysplasia) from treatment is a unique case report.
The presence of central nervous system relapse in acute promyelocytic leukemia patients is very unlikely compared to recurring mainly in the bone marrow. It is also uncommon to be diagnosed with sideroblastic anemia (form of myelodysplastic syndrome) as a result from treatment for acute promyelocytic leukemia. This case report highlights the detection, treatment/maintenance with idarubicin, all-trans-retinoic-acid, arsenic trioxide, methotrexate, 6-mercaptopurine, and ommaya reservoir intrathecal methotrexate administration in a patient that had central nervous system relapse of acute promyelocytic leukemia and acquired sideroblastic anemia.
In essence, first time relapse concerning the central nervous system in treated acute promyelocytic leukemia patients who had a good response to therapy is very uncommon. The acquirement of a myelodysplastic syndrome such as ringed sideroblastic anemia is also rare regarding this patient population. Although such cases are infrequent, this case report represents a unique insight of the detection, treatment, and maintenance of a 60-year-old man diagnosed with acute promyelocytic leukemia, resulting in the acquirement of sideroblastic anemia and central nervous system relapse.
Core Tip: Central nervous system recurrence and acquirement of sideroblastic anemia is a rare occurrence on their own and are even more unlikely to occur together in treated acute promyelocytic leukemia patients. We present a case presentation of a 60-year-old man that had a good response to acute promyelocytic leukemia treatment, that later presented with a central nervous system recurrence of acute promyelocytic leukemia and acquired sideroblastic anemia (a form of myelodysplasia) from treatment is a unique case report.
- Citation: Nawaz H, Choudhry A, Morse WJ. Central nervous system recurrence in a patient treated for acute promyelocytic leukemia, resulting in sideroblastic anemia: A case report. World J Hematol 2022; 9(1): 1-5
- URL: https://www.wjgnet.com/2218-6204/full/v9/i1/1.htm
- DOI: https://dx.doi.org/10.5315/wjh.v9.i1.1
Acute promyelocytic leukemia is a form of acute myeloid leukemia that is mainly due to a translocation of chromosomes fifteen and seventeen that influence the expression of the promyelocytic leukemia/retinoic acid receptor alpha (PML-RARA) genes[1]. It has been noted that myeloid neoplasms related to treatment are more prevalent in solid tumors and lymphomas than compared to a myeloid neoplasm arising from acute myeloid leukemia (AML) or acute promyelocytic leukemia (APL). Denu et al[2] 2016 had shown that 1% to 7% of patients that were treated with chemotherapy for acute promyelocytic leukemia developed myelodysplastic syndrome or acute myeloid leukemia. In 1998, Liso et al[3] 1998 conducted a review of 120 patients treated with all-trans-retinoic acid (ATRA) and chemotherapy that were seen over a period of nine years at two different institutions. 7 out of the 120 patients were found to have extramedullary disease, but only one patient had disease in the central nervous system (CNS). Montesinos et al[4] 2009 conducted a study from 1996 to 2005 that had 739 acute promyelocytic leukemia (APL) patients who received induction therapy with ATRA and idarubicin, as well as consolidation chemotherapy for relapse. There were 11 patients that had confirmed central nervous system (CNS) relapse with a five-year cumulative central nervous system incidence of 1.7%. Latagliata et al[5] 2002 discovered that 6.5% of the 77 acute promyelocytic leukemia patients who had a complete response to induction and consolidation therapy acquired therapy-related myelodysplasia, acute myeloid leukemia, or a combination of the two in their study. One can see that’s why this case presentation of a 60-year-old man that had a good response to acute promyelocytic leukemia treatment, that later presented with a central nervous system recurrence of acute promyelocytic leukemia and acquired sideroblastic anemia (a form of myelodysplasia) from treatment is a unique case report.
A 60-year-old white male comes into the hospital in 2009 with a complaint of blurred vision in his right eye (ophthalmologist noted occlusion of retinal vein), feeling somnolent, and weak for the past four weeks.
He was admitted to the emergency room for weakness, fatigue, and leukocytosis. The patient attributed his condition to a treated sinus infection he had prior. The patient presentation noted minor bruising over the arms and legs, and no signs of bleeding episodes, such as, epistaxis, hematemesis, melena, or blood per rectum.
Sinus infection.
Non-contributory.
Generalized weakness, fatigue, and leukocytosis. The patient attributed his condition to a treated sinus infection he had prior. The patient presentation noted minor bruising over the arms and legs, and no signs of bleeding episodes, such as, epistaxis, hematemesis, melena, or blood per rectum.
White blood cell count of 41600, hemoglobin of 8.4, hematocrit of 23, platelet count of 20000, mean corpuscular volume of 93, segmented neutrophils percentage (seg %) of 2%, lymphocyte percentage of 6%, monocyte percentage of 3%, and absolute neutrophil count of 800. hemoglobin of 14, hematocrit of 39, white blood cell count of 9100, and platelet count of 130000. Three months later in 2020, the patient remained on maintenance low dose methotrexate and had improved blood counts that were a hemoglobin of 13, hematocrit of 40, white blood cell count of 7700, and platelet count of 158000. Hemoglobin of 14, hematocrit of 41, white blood cell count of 8600, and platelet count of 165000. Hemoglobin of 13, hematocrit of 39, white blood cell count of 7400, and platelet count of 157000.
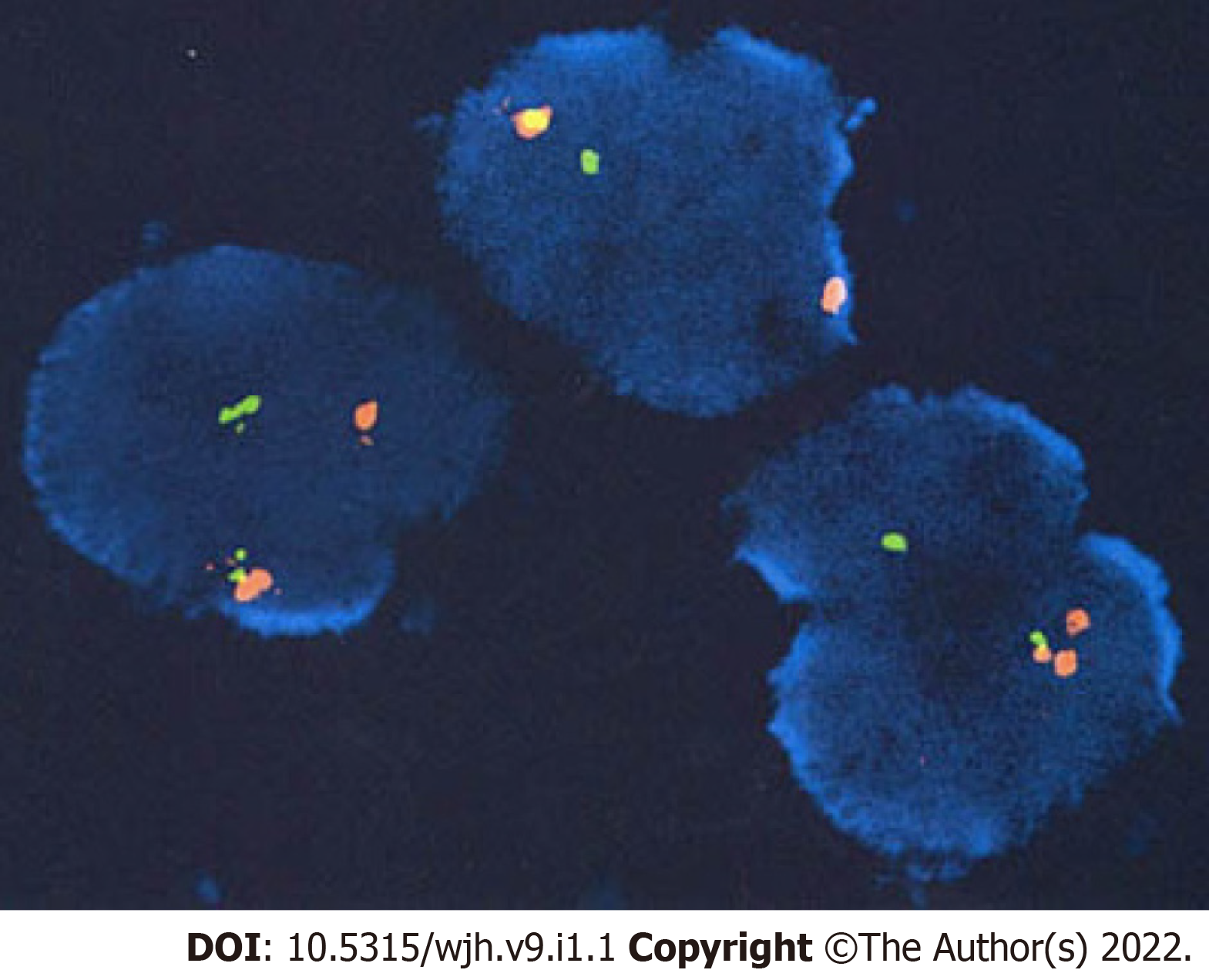
Bone marrow biopsy of PML-RARA gene fusion by interphase fluorescent in-situ hybridization (Figure 1).
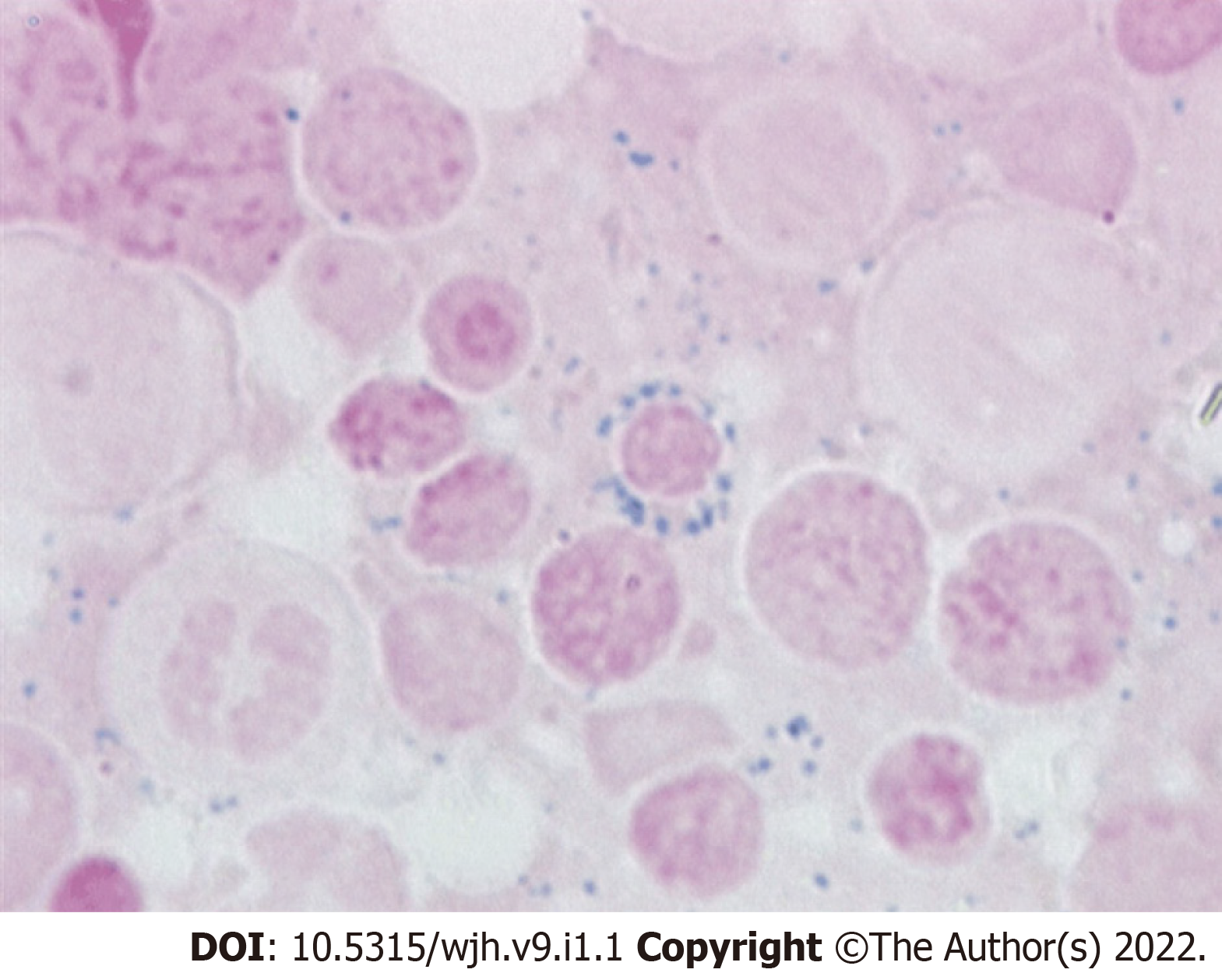
Central nervous system relapse of acute promyelocytic leukemia and acquired sideroblastic anemia (Figure 2).
Idarubicin, ATRA, arsenic trioxide, methotrexate, 6-Mercaptopurine, and ommaya reservoir intrathecal methotrexate.
Patient has remained stable as of 2020, being manages with folic acid, thiamine, and pyridoxine.
One can determine that central nervous system recurrence and acquirement of sideroblastic anemia is a rare occurrence on their own and are even more unlikely to occur together in treated acute promyelocytic leukemia patients. From 1996 to 2008, Montesinos et al[6] 2010 analyzed therapy-related myeloid neoplasms in 1025 acute promyelocytic leukemia patients who received anthracycline-based chemotherapy and All-Trans-Retinoic acid. Seven out of the 918 patients that achieved a complete response had developed a therapy related neoplasm after a median of 43 mo from complete response: With a 6-year cumulative incidence of therapy-related myeloid neoplasm of 2.2 %. From 1991 to 1998 Lobe et al[7] 2003 dealt with treating 677 newly diagnosed acute promyelocytic leukemia patients. Six hundred and seventeen out of the 677 patients achieved a complete response with combination All-Trans-Retinoic acid and chemotherapy; 246 acute promyelocytic leukemia patients had received maintenance chemotherapy, 6-mercaptopurine, and methotrexate. At the median 51-month follow-up, 0.97% of the treated acute promyelocytic leukemia patients developed myelodysplastic syndrome. De Botton et al[8] 2006 discovered that 23% of patients relapsed after obtaining a complete response, and about 5% had a 3-year cumulative incidence for first time central nervous system relapse. The study analyzed potential risk factors for central nervous system relapse: age less than 45 years-old (P = 0.05), bcr3 PML-RAR-alpha isoform (P = 0.0003), and a white blood cell count greater than or equal to 10000/mm3. Specchia et al[9] 2001 enrolled patients into two trials that were designed to see if there was any difference in extramedullary disease at relapse regarding combination All-Trans-Retinoic acid and chemotherapy compared to solely chemotherapy. It was discovered that the All-Trans-Retinoic acid plus chemotherapy and solely chemotherapy arms had 0.6% and 2%, respectively. These previous cases highlight the rarity of an acute promyelocytic leukemia patient acquiring central nervous system relapse as well as myelodysplastic syndrome, which make this case report relevant for future treatment applications pertaining to this patient population.
In essence, first time relapse concerning the central nervous system in treated acute promyelocytic leukemia patients who had a good response to therapy is very uncommon. The acquirement of a myelodysplastic syndrome such as ringed sideroblastic anemia is also rare regarding this patient population. Although such cases are infrequent, this case report represents a unique insight of the detection, treatment, and maintenance of a 60-year-old man diagnosed with acute promyelocytic leukemia, resulting in the acquirement of sideroblastic anemia and central nervous system relapse.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Hematology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Xu F, Zhou X S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Fenaux P, Chomienne C, Degos L. Acute promyelocytic leukemia: biology and treatment. Semin Oncol. 1997;24:92-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 85] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Denu RA, Henrich Lobo R, Mattison RJ. Management of differentiation syndrome in an elderly patient with acute promyelocytic leukemia who subsequently developed refractory anemia with ring sideroblasts. Leuk Lymphoma. 2016;57:2905-2907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Liso V, Specchia G, Pogliani EM, Palumbo G, Mininni D, Rossi V, Teruzzi E, Mestice A, Coppi MR, Biondi A. Extramedullary involvement in patients with acute promyelocytic leukemia: a report of seven cases. Cancer. 1998;83:1522-1528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Montesinos P, Díaz-Mediavilla J, Debén G, Prates V, Tormo M, Rubio V, Pérez I, Fernández I, Viguria M, Rayón C, González J, de la Serna J, Esteve J, Bergua JM, Rivas C, González M, González JD, Negri S, Brunet S, Lowenberg B, Sanz MA. Central nervous system involvement at first relapse in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and anthracycline monochemotherapy without intrathecal prophylaxis. Haematologica. 2009;94:1242-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 78] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | Latagliata R, Petti MC, Fenu S, Mancini M, Spiriti MA, Breccia M, Brunetti GA, Avvisati G, Lo Coco F, Mandelli F. Therapy-related myelodysplastic syndrome-acute myelogenous leukemia in patients treated for acute promyelocytic leukemia: an emerging problem. Blood. 2002;99:822-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 97] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Montesinos P, González JD, González J, Rayón C, de Lisa E, Amigo ML, Ossenkoppele GJ, Peñarrubia MJ, Pérez-Encinas M, Bergua J, Debén G, Sayas MJ, de la Serna J, Ribera JM, Bueno J, Milone G, Rivas C, Brunet S, Löwenberg B, Sanz M. Therapy-related myeloid neoplasms in patients with acute promyelocytic leukemia treated with all-trans-retinoic Acid and anthracycline-based chemotherapy. J Clin Oncol. 2010;28:3872-3879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Lobe I, Rigal-Huguet F, Vekhoff A, Desablens B, Bordessoule D, Mounier C, Ferrant A, Sanz M, Fey M, Chomienne C, Chevret S, Degos L, Fenaux P; European APL group experience. Myelodysplastic syndrome after acute promyelocytic leukemia: the European APL group experience. Leukemia. 2003;17:1600-1604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 58] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | de Botton S, Sanz MA, Chevret S, Dombret H, Martin G, Thomas X, Mediavilla JD, Recher C, Ades L, Quesnel B, Brault P, Fey M, Wandt H, Machover D, Guerci A, Maloisel F, Stoppa AM, Rayon C, Ribera JM, Chomienne C, Degos L, Fenaux P; European APL Group; PETHEMA Group. Extramedullary relapse in acute promyelocytic leukemia treated with all-trans retinoic acid and chemotherapy. Leukemia. 2006;20:35-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 119] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | Specchia G, Lo Coco F, Vignetti M, Avvisati G, Fazi P, Albano F, Di Raimondo F, Martino B, Ferrara F, Selleri C, Liso V, Mandelli F. Extramedullary involvement at relapse in acute promyelocytic leukemia patients treated or not with all-trans retinoic acid: a report by the Gruppo Italiano Malattie Ematologiche dell'Adulto. J Clin Oncol. 2001;19:4023-4028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 102] [Article Influence: 4.3] [Reference Citation Analysis (0)] |