Revised: April 16, 2014
Accepted: May 16, 2014
Published online: August 2, 2014
Processing time: 189 Days and 14.3 Hours
Lichen planus is a common inflammatory disease but its perforating variety is not so common and it has been described in small number of text and articles. Here we reported a case of plantar lichen planus where there was a history of discharge of dark grains from the sole of foot and diagnosing the disease as eumycetoma of dark grains repeated antifungal therapy could not resolve the lesions and histopathologically it showed the classical pictures of lichen planus. Collaborating the clinical and histological features we have diagnosed the case as perforating lichen planus but Verhoeff-Van Gieson stain could not elucidate the perforating channel which ot difficult to delineate and often missed. So, we have put the diagnosis of plantar lichen planus and treated with intramuscular triamcinolone and the lesions resolved.
Core tip: The case was initially thought to be eumycetoma of dark grains as there was history of discharge of grains but after repeated antifungal therapy it did not resolve and in histopathology it was found as lichen planus. In this case the clinical features collaborating with perforating lichen planus but histopathology has failed to elucidate the perforating channel which is often missed and difficult to delineate. So, it is better to do a histopathology before giving the treatment as there is overlapping clinical features of various diseases.
- Citation: Das A, Das D, Gharami RC. Plantar lichen planus masquerading eumycetoma of dark grains. World J Dermatol 2014; 3(3): 73-75
- URL: https://www.wjgnet.com/2218-6190/full/v3/i3/73.htm
- DOI: https://dx.doi.org/10.5314/wjd.v3.i3.73
Lichen planus (LP) is a common chronic inflammatory papulosquamous disorder of skin,hair, and nail generally characterized by shiny, violaceous, flat-topped polygonal papules. They may be closely aggregated or widely dispersed.
There are many variants of lichen planus including annular, linear or blaschkoid pattern, hypertrophic, atrophic, erosive, vesicular, follicular LP, micropapular or eruptive, lichen planus pigmentosus, etc. Involvement of palms and soles is not very common[1]. Morphology of palmoplantar lichen planus is not like that of other areas. Lesions may be profoundly hyperkeratotic plaque, honeycomb pattern, perforating type, ulcerative type, etc.[2].
Here we reported a case of plantar lichen planus presented with discrete keratotic papules with central crater and history of discharging of some material resembling mycetoma.
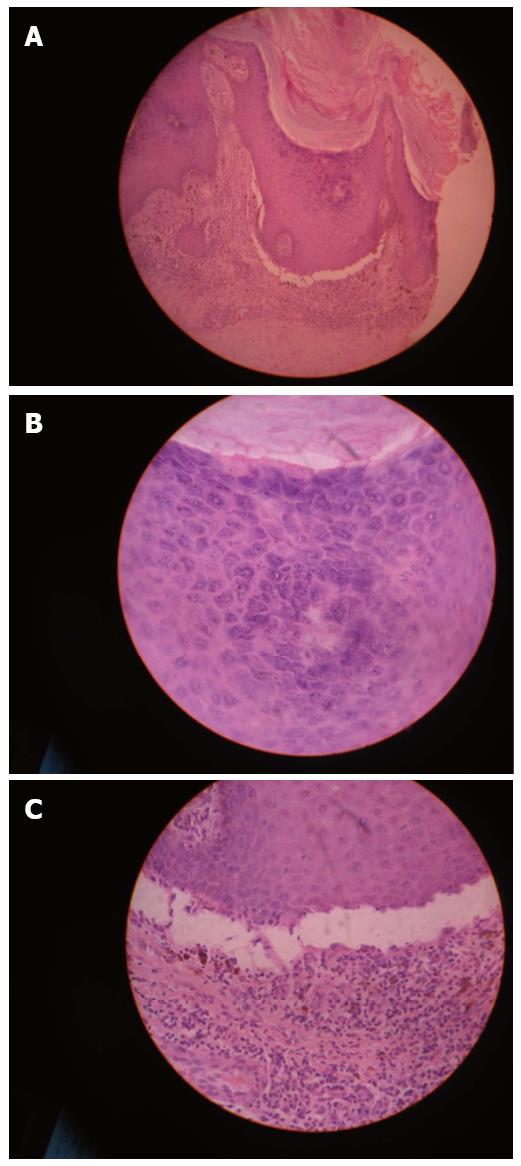
A 48-year-old farmer presented with solid elevated lesions over medial border of left foot and a history of blackish discharge from the lesions for last 2 years. On examination 4-5 hyperkeratotic papules with central craters with a mild indurated background were found (Figure 1). Mucosae, nails and other areas of the body were normal. The case was provisionally diagnosed as mycetoma. Biopsy was done for histopathological examination and fungal culture. Fungal culture yield negative result. X-ray of the foot revealed no abnormality. Biopsy showed a finding consisting of lichen planus (Figure 2) without any epidermal channel. Verhoeff-Van Gieson stain excluded discharge of any altered tissue. Routine examination of blood, urine and stool, chest X-ray found no abnormality. Two doses of injection triamcinolone (40 mg/cc) intramuscularly were given at 2 wk interval, followed by 3 wk interval for another 2 such. Lesions resolved completely without any relapse during 6 mo period of follow up.
Perforating lichen planus is an uncommon variant of LP. It presents as hyperkeratotic papules or plaques topped by crust or a keratotic plug. Occasionally keratotic plugs might be dislodged, leaving behind pitted keratotic papules or plaques. Hanau and Sengel[3] reported a case of perforating LP in 1984 in a 52-year-old woman where histology showed classic features of LP and there was a channel containing epithelial cells, hyaline bodies and fibrillar material. Hanau and Sengel[3] speculated that hyaline bodies present abundantly at the base of perforation could irritate the dermo-epidermal junction and consequently initiate the process of perforation of epidermis.
Gutte and Khopkar[4] again reported a case of perforating LP with acrosyringeal accentuation of infiltrate.
In our case there were keratotic papules with central craters. Craters were formed due to dislodgement of superficial hyperkeratotic layers and probably partially detached material was described by the patient as discharge. Serial sections of the specimen also failed to reveal any epidermal channel. So, our case is not exactly a case of perforating lichen planus as mentioned by others[3,4]. Or this might be a case of perforating lichen planus where histopathology was by chance failed to reveal the epidermal channel as it not an easy job to find out. Clinically the case is correlating what was described by previous authors[3,4].
Dark grains coming out from the plaque over the sole.
Mycetoma.
Eumycetoma, perforating disorders.
Fungal culture yields negative result.
Histopatholgy suggestive of lichen pplanus but it is very difficult to elucidate the perforating channel of the lesion and we didn’t get the same in histopathology.
Systemic glucocorticoid (injection triamcinolone acetonide 40 mg/cc deep intramuscular every monthly).
Perforating lichen planus-lichen planus presents as hyperkeratotic papules or plaques topped by crust or a keratotic plug. Occasionally keratotic plugs might be dislodged, leaving behind pitted keratotic papules or plaques. There lies a channel containing epithelial cells, hyaline bodies and fibrillar material. Hyaline bodies present abundantly at the base of perforation could irritate the dermo-epidermal junction and consequently initiate the process of perforation of epidermis.
Many dermatological lesions clinically misdiagnosed as other entity unless the histopatholgy helps to find the original lesion.
This paper is a usefull clinical case and wrote well.
P- Reviewer: Arenas RG, Rapuano CJ, Severo LC S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Breathnach SM. Lichen palnus and lichenoid disorders. Rook’s Textbook of dermatology. 8th edition. Oxford: Wiley-Blackwell 2010; 41.1-41.28. [DOI] [Full Text] |
| 2. | Haldar SS, Khopkar U. Clical Features of Lichen PLanus. In: Khopkar U, Valia A, editors. Lichen Planus. 1st ed 2013; 21-40. |
| 3. | Hanau D, Sengel D. Perforating lichen planus. J Cutan Pathol. 1984;11:176-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Gutte R, Khopkar U. Perforating lichen planus. Indian J Dermatol Venereol Leprol. 2011;77:515-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |