Revised: November 3, 2013
Accepted: November 15, 2013
Published online: February 2, 2014
Processing time: 136 Days and 23.3 Hours
Verrucous epidermal naevus (VEN) is a rare form of epidermal naevus. We present a case of VEN occurring over the perianal region of a 7-year-old boy. The lesion was initially thought to be an area of chronic dermatitis; however it was refractory to treatment. Histopathology confirmed the diagnosis of VEN. VEN in the inguinogenital region may be misdiagnosed as flexural psoriasis, genital warts or sexual abuse. This is what precisely happened to our patient for a duration of more than 1 year.
Core tip: The most interesting feature of this case is the difficulty of diagnosing verrucous epidermal naevus (VEN) of the genital region. It is expected that genital lesions are troublesome entities with respect to accurate diagnosis. It is essential for pediatricians as well as dermatologists to consider VEN as a possibility in warty genital or perianal lesions to avoid inappropriate accusations and irrelevant investigations of child abuse.
- Citation: Das A, Gayen T, Das NK, Shome K. Perianal verrucous epidermal nevus masquerading as warts. World J Dermatol 2014; 3(1): 1-3
- URL: https://www.wjgnet.com/2218-6190/full/v3/i1/1.htm
- DOI: https://dx.doi.org/10.5314/wjd.v3.i1.1
Epidermal naevi are hamartomas of the epidermis and papillary dermis. The histopathological appearance of verrucous epidermal naevus (VEN) is characteristic, with columns of hypergranulosis and orthokeratotic hyperkeratosis alternating with well-defined columns of agranulosis and parakeratotic hyperkeratosis[1]. VEN affects the head neck region and the lower limbs; however, in a minority of patients, occur in the genital area.
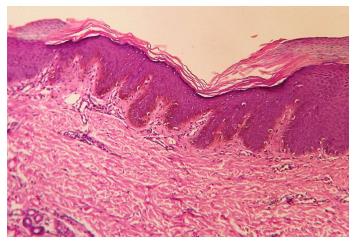
A 7-year-old boy, hailing from an orphanage was referred to Dermatology for review of an intensely pruritic lesion in the perianal area, which had been present since 1 year. Previous treatment comprised of topical steroids and topical tar preparations, as per the advice of local physicians. After multiple visits to different medical professionals, the case was diagnosed as warts and he had received 2 cycles of cryotherapy before presenting to us. But, these only partially relieved his symptoms and the lesion remained unchanged. He was otherwise in good health, without regular medications or allergies. Since the child came from an orphanage, we took a multidisciplinary approach and meticulously enquired about history of sexual abuse. There was a definite history of multiple episodes of sodomy in the orphanage. On cutaneous examination, we found an extremely itchy, moist hyperpigmented and excoriated plaque over the perianal region. The surface of the plaque was verrucous in some places and atrophic and dyspigmented in other areas (Figure 1). There were no stigmata of eczema elsewhere on the skin. Hair, nail and mucosae did not reveal any abnormality. Even we kept perianal warts as our first differential diagnosis. Apart from that, other intertriginous dermatitis like candidiasis, zinc deficiency etc. were also kept in consideration. Routine blood investigations were within normal limits. Biopsy of the perianal region showed evidence of psoriasiform epidermal hyperplasia, with acanthosis, alternating parakeratosis and compact hyperkeratosis (Figure 2). Based on the clinical and histopathological findings, a diagnosis of verrucous epidermal nevus was done. The patient was prescribed topical antibiotic and steroid combination and surgical referral has been done for discussion of the viability of excision in this location. He was referred for psychiatric counseling as well in order to take care of the mental trauma which was much more than the physical issues.
The verrucous morphology and the occurrence in the genitalia may raise the question of sexually transmitted disease and sexual abuse. In a case report by Sarifakioglu et al[2], a patient with scrotal verrucous epidermal naevus was treated with cryotherapy for genital warts prior to diagnosis. Sexual abuse is often suspected in children with genital dermatological conditions including dermatitis, vulval immunobullous conditions, infantile haemangioma, psoriasis etc.[3]. Lichen sclerosus et atrophicus is often mistaken for child abuse with clinical findings of atrophic plaques, genital pruritus, erosions and bruising. A case of vulvitis circumscripta plasmacellularis mimicking child abuse has been reported by Albers et al[4]. Porzionato et al[5] reported a case where sexual abuse was suspected in a patient with perianal and vulval Crohn's disease presenting as perianal pruritus, fissuring and swelling of the labia majora.
VEN is resistant to topical therapies and symptomatic improvement usually requires ongoing therapy. Topical therapies include coal tar, corticosteroids under occlusion and retinoic acid. Topical calcipotriol has been used successfully. The long-term application of potent steroids on the genitalia is limited due to the possible adverse effects. Physical therapies used in the treatment include dermabrasion, cryotherapy and carbon dioxide laser therapy. Full-thickness excision with primary closure, use of adjunctive tissue expansion, skin flaps and split-thickness skin graft has been reported by Lee et al[6] in a case series of four patients (three children, one adult). Sarifakioglu et al[2] described total excision of an epidermal naevus occurring on the scrotum.
The purpose behind reporting this case is to demonstrate the difficulty of diagnosing VEN of the genital region. It is quite common for genital lesions to evade accurate diagnosis and this is exemplified in our case. It is essential for pediatricians as well as dermatologists to consider VEN as a possibility in warty genital or perianal lesions to avoid inappropriate accusations and irrelevant investigations of child abuse. Diagnostic pointers include refractoriness to treatment, hyperkeratosis and the unilateral nature of the lesion. The diagnosis of verrucous epidermal naevus should be suspected in persistent genital eczematous or psoriasiform lesions in pediatric age group and any discordance in response to treatment for such lesions must be met with, seriously; and referral to a dermatologist is warranted.
A 7-year-old boy, hailing presented with an intensely pruritic lesion in the perianal area, which had been present since 1 year.
Cutaneous examination showed moist hyperpigmented and excoriated plaque over the perianal region, the surface being verrucous in some places and atrophic and dyspigmented in others. Clinically, it was probably a result of sexual abuse.
Clinical differentials include warts, lichen sclerosus et atrophicus, verrusous epidermal nevus, flexural psoriasis, dermatitis, candidiasis, zinc deficiency, etc.
Labortaory investigations were within normal limits.
Biopsy of the perianal region showed evidence of psoriasiform epidermal hyperplasia, with acanthosis, alternating parakeratosis and compact hyperkeratosis. It was consistent with Verrucous epidermal nevus.
Patient has been prescribed topical antibiotic and steroid combination and surgical referral has been done for discussion of the viability of excision in this location.
Sarifakioglu reported a patient with scrotal verrucous epidermal naevus who was treated with cryotherapy for genital warts prior to diagnosis. A case of vulvitis circumscripta plasmacellularis mimicking child abuse has been reported by Albers. Porzionato reported a case where sexual abuse was suspected in a patient with perianal and vulval Crohn's disease presenting as perianal pruritus, fissuring and swelling of the labia majora.
The crux of this report is the difficulty of diagnosing VEN of the genital region. It is quite common for genital lesions to evade accurate diagnosis, consistent with the case. It is essential for pediatricians as well as dermatologists to consider VEN as a possibility in warty genital or perianal lesions to avoid inappropriate accusations and irrelevant investigations of child abuse. In any case of diagnostic dilemma, a histopathological examination is quintessential.
The diagnosis of verrucous epidermal naevus should be suspected in persistent genital eczematous or psoriasiform lesions in pediatric age group and any discordance in response to treatment for such lesions must be met with, seriously; and a timely referral to a dermatologist is warranted. It is an interesting example to reflect on the implications of this disease and especially on the diagnostic difficulties. The manuscript emphasizes the special attention that was needed given that the boy lived in an orphanage.
P- Reviewers: Cuevas-Covarrubias SA, Guarneri F, Hu SCS, Kaliyadan F, Negosanti L, Schmidt E S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
| 1. | Bandyopadhyay D, Sen S. Perianal verrucous epidermal naevus mimicking perianal warts. Sex Transm Infect. 2003;79:424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Sarifakioglu E, Yenidunya S. Linear epidermolytic verrucous epidermal nevus of the male genitalia. Pediatr Dermatol. 2007;24:447-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Harth W, Linse R. Dermatological symptoms and sexual abuse: a review and case reports. J Eur Acad Dermatol Venereol. 2000;14:489-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Albers SE, Taylor G, Huyer D, Oliver G, Krafchik BR. Vulvitis circumscripta plasmacellularis mimicking child abuse. J Am Acad Dermatol. 2000;42:1078-1080. [PubMed] |
| 5. | Porzionato A, Alaggio R, Aprile A. Perianal and vulvar Crohn’s disease presenting as suspected abuse. Forensic Sci Int. 2005;155:24-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Lee BJ, Mancini AJ, Renucci J, Paller AS, Bauer BS. Full-thickness surgical excision for the treatment of inflammatory linear verrucous epidermal nevus. Ann Plast Surg. 2001;47:285-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |