Copyright
©The Author(s) 2016.
World J Dermatol. Nov 2, 2016; 5(4): 136-143
Published online Nov 2, 2016. doi: 10.5314/wjd.v5.i4.136
Published online Nov 2, 2016. doi: 10.5314/wjd.v5.i4.136
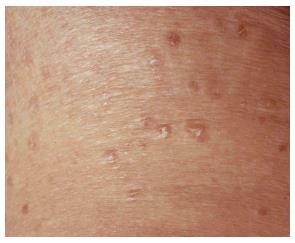
Figure 1 Patient 4 presented with a 6 mo history of persistent 2 to 8 mm papules of mycosis fungoides on the trunk and legs.
Figure 2 Skin specimen from patient 4 shows an acanthotic epidermis that contains atypical lymphocytes with hyperchromatic irregular nuclei (insert).
The dermis has a superficial infiltrate composed of normal and atypical lymphocytes (H and E, × 400).
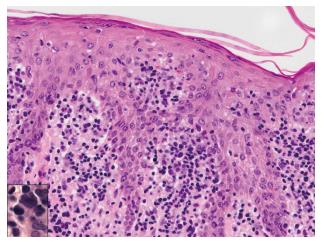
Figure 3 Persistent 2 to 14 mm papules of mycosis fungoides scattered on trunk and legs of patient 5.
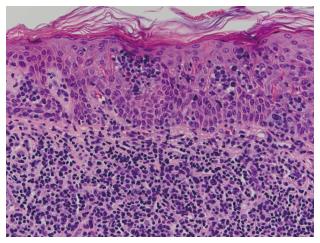
Figure 4 Skin specimen from patient 5 shows a moderately dense lichenoid infiltrate, wiry bundles of collagen in a thickened papillary dermis, and follicular mucinosis.
Numerous atypical lymphocytes, some with large irregular nuclei, are located within the epidermis, both as solitary units and in aggregates, and dermal infiltrate (H and E, × 400).
Figure 5 Patient 6 presented with a 15 mo history of persistent papules and small nodules, some with scaling, disseminated on the trunk and legs.
Figure 6 Skin specimen from patient 6 shows typical histopathologic features of mycosis fungoides.
Nests of medium to large sized neoplastic lymphocytes with pleomorphic and cerebriform nuclei are observed within the epidermis (Pautrier microabscesses) and adjacent superficial dermis (H and E, × 400).
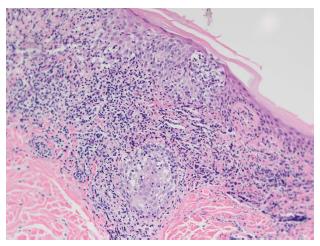
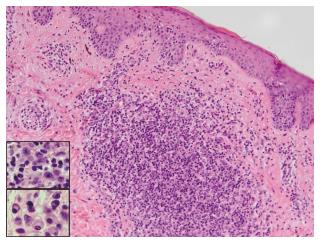
Figure 7 Skin specimen from patient 2 shows a perivascular and dense nodular infiltrate in the superficial and mid-dermis.
A fibrotic papillary dermis and scattered epidermotropic lymphocytes aligned along the basal layer in the absence of spongiosis (H and E, × 400). The dermal infiltrate is composed of lymphocytes, some with large hyperchromatic cerebriform nuclei, large immunoblast-like cells (top insert), small clusters of plasma cells (bottom insert), and occasional eosinophils.
- Citation: Vonderheid EC, Kadin ME, Telang GH. Papular mycosis fungoides: Six new cases and association with chronic lymphocytic leukemia. World J Dermatol 2016; 5(4): 136-143
- URL: https://www.wjgnet.com/2218-6190/full/v5/i4/136.htm
- DOI: https://dx.doi.org/10.5314/wjd.v5.i4.136