Published online Sep 27, 2020. doi: 10.5313/wja.v9.i1.3
Peer-review started: June 8, 2020
First decision: July 4, 2020
Revised: July 10, 2020
Accepted: August 25, 2020
Article in press: August 25, 2020
Published online: September 27, 2020
Processing time: 106 Days and 22.9 Hours
The usage of bronchoscopy during percutaneous dilatational tracheostomy remains under debate. The proponents of bronchoscopy advocating safety of the procedure, whereas the critics raising the concerns about the cost, possible delay in the procedure, and waiting for the device.
We are highlighting a case of percutaneous dilatational tracheostomy where bronchoscopy aided in diagnosing a rare situation of wire entrapment within the endotracheal tube, treated by withdrawing the wire from the endotracheal tube with good outcome.
The bronchoscopy guided approach permitted early diagnosis and helped to end the procedure without complication or possible major surgery in a case of accidental wire puncture of the endotracheal tube.
Core Tip: Bronchoscopic guided approach made diagnosis help to end the procedure without complication or possible major surgery.
- Citation: Omar AS, Sudarsanan S, AlKhulaifi A. Unusual bronchoscopic value in percutaneous dilatational tracheostomy: A case report. World J Anesthesiol 2020; 9(1): 3-6
- URL: https://www.wjgnet.com/2218-6182/full/v9/i1/3.htm
- DOI: https://dx.doi.org/10.5313/wja.v9.i1.3
Percutaneous dilatational tracheostomy (PDT) is a minimally invasive procedure that has greatly replaced surgical technique in modern intensive care units (ICU)[1]. The procedure is safe, rapid and effective in establishing long term airway for patients with long term ventilatory requirements[2]. The use of bronchoscopy during the procedure was suggested, as it provides tracheal visualization, during needle insertion, tracheal dilatation and tracheostomy tube placement[3]. In a recent single center study comparing both techniques, the authors found that PDT using blind technique was as safe as the bronchoscopic one, in terms of incidence of reported complications[4]. Additional advantage of cost effectiveness was described by Taha et al[5]. We are highlighting a case of PDT where bronchoscopy played a pivotal role in saving the patient from potential catastrophe.
A 56-year-old man was admitted to the ICU after cardiac surgery, he had a complicated course and prolonged mechanical ventilation, requiring percutaneous tracheostomy after 14 d of intubation.
The patient’s course was complicated with stroke and inability to wean from mechanical ventilation.
The patient is a nonsmoker, not known to have diabetes mellitus; he had 10 years history of essential arterial hypertension, he had also dyslipidemia. A coronary angiography done 6 months prior to surgery showed three-vessel disease for surgical intervention. His routine medications included atenolol (50 mg/d), acetylsalicylic acid (150 mg/d), and rosuvastatine (10 mg/d). The patient had family history of ischemic heart disease and dyslipidemia.
The patient pre-procedure examination showed dimished conscious level with inability to protect his airways. The vital signs showed temperature of 37.0 °C, blood pressure of 110/66 mmHg, heart rate of 71 beats/min, and oxygen saturation of 97% on mechanical ventilation with FIO2 of 30%. The heart rate was regular. The rest of cardiac, chest and abdomen examinations were unremarkable.
Laboratory work-up was unremarkable.
Computed tomography (CT) scan showed multiple lacunar infarctions.
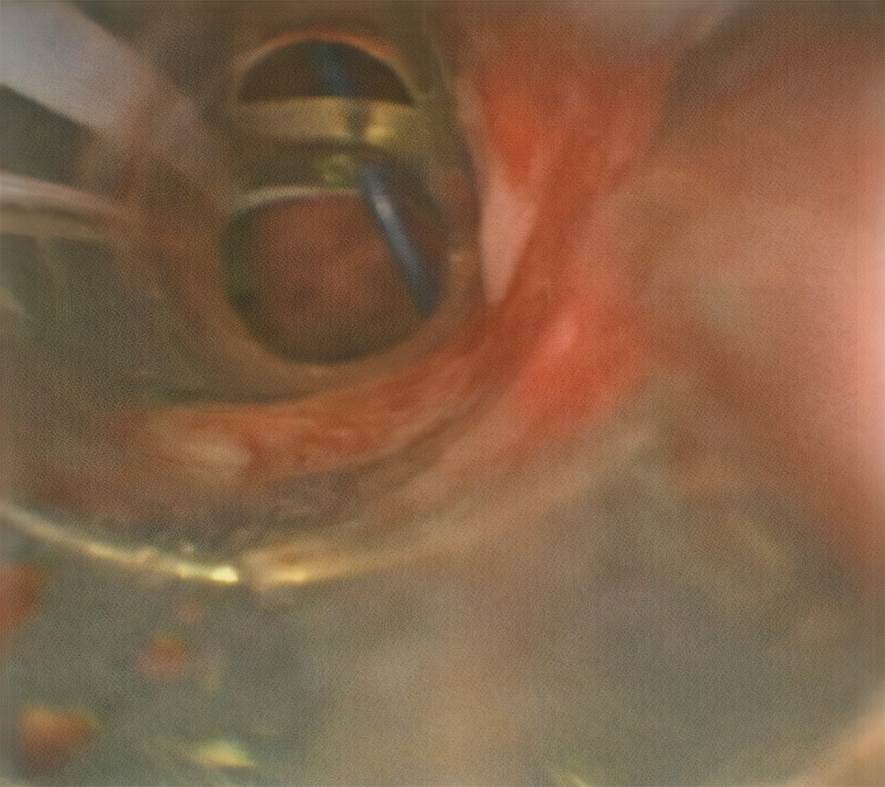
The patient was scheduled for percutaneous tracheostomy due to delayed recovery and expected prolonged hospital course. The procedure was done under bronchoscopic guidance, the needle followed by the guide wire were noted to pass into the trachea. Successive dilatations by the small followed by the large blue Rhino dilators were carried out, the procedure ended with insertion of the adequately sized tracheostomy tube over the respective dilator. Attempt to withdraw the wire was met with difficulty in the form of resistance, this aroused suspicion of abnormal course of wire or its entrapment. The bronchoscope was passed through the tracheostomy tube revealing acceptable position and level of the tracheostomy tube, the point where the wire was stuck could not be identified through the tracheostomy tube. The bronchoscope was withdrawn and advanced again through the endotracheal tube (ETT), it was noted that wire punctured the terminal end of the ETT distal to the Murphy’s eye and got entrapped in this position (Figure 1). The case was diagnosed as wire entrapment in the ETT after accidental trocar puncturing.
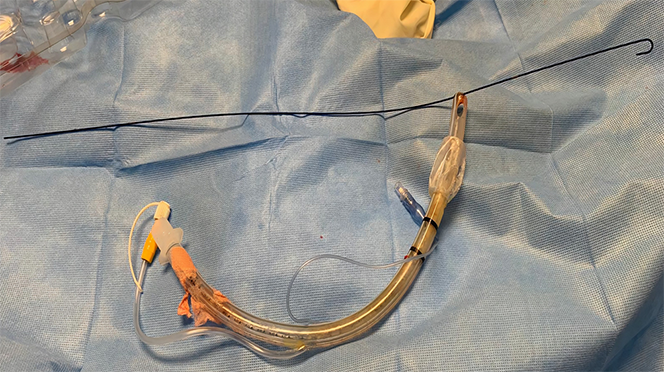
After careful bronchoscopic inspection the best option was to withdraw the ETT from the mouth, which pulled the wire accordingly.
The procedure ended smoothly, and the patient was left in a stable condition without any procedure related complications, follow up chest X-ray was unremarkable.
Percutaneous dilational tracheostomy (PDT) became a standard procedure since its introduction at by Cigalia more than 30 years back[6]. However, the safety of the procedure remains questionable. The concomitant use of bronchoscopy was associated with a significant reduction of the trachesotomy related complications in the early reports[7]. Identifying the place of the first tracheal puncture, confirming the position of the needle are additional bronchoscopic guided procedure advantages[8]. However, Taha and Omar performed a randomized controlled trial comparing bronchoscopic and blind techniques and argued that blind technique could be as safe as the bronchoscopy guided one, when experience exist[5]. Sampling of the airway could be an additional advantage in patients with suspected airway infection[9]. In our patient the bronchoscope provided an unusual advantage that needs to be highlighted. Our case emphasized this role when a gentle trial to remove the wire from tracheostomy end failed after which we elected to withdraw the ETT, the wire followed the tube without further complications (Figure 2).
The bronchoscopy guided approach permitted early diagnosis and helped to end the procedure without complication or possible major surgery in a case of accidental wire puncturing of the endotracheal tube.
Manuscript source: Unsolicited manuscript
Specialty type: Critical care medicine
Country/Territory of origin: Qatar
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Terrani A S-Editor: Zhang H L-Editor: A P-Editor: Li X
| 1. | Heikkinen M, Aarnio P, Hannukainen J. Percutaneous dilational tracheostomy or conventional surgical tracheostomy? Crit Care Med. 2000;28:1399-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 98] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Putensen C, Theuerkauf N, Guenther U, Vargas M, Pelosi P. Percutaneous and surgical tracheostomy in critically ill adult patients: a meta-analysis. Crit Care. 2014;18:544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 113] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 3. | Porter JM, Ivatury RR. Preferred route of tracheostomy--percutaneous versus open at the bedside: a randomized, prospective study in the surgical intensive care unit. Am Surg. 1999;65:142-146. [PubMed] |
| 4. | Gadkaree SK, Schwartz D, Gerold K, Kim Y. Use of Bronchoscopy in Percutaneous Dilational Tracheostomy. JAMA Otolaryngol Head Neck Surg. 2016;142:143-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Taha A, Omar AS. Percutaneous dilatational tracheostomy. Is bronchoscopy necessary? A randomized clinical trial. Trends Anaesth Crit Care. 2017;15:20-24. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Ciaglia P, Firsching R, Syniec C. Elective percutaneous dilatational tracheostomy. A new simple bedside procedure; preliminary report. Chest. 1985;87:715-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 733] [Cited by in RCA: 617] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 7. | Kost KM. Endoscopic percutaneous dilatational tracheotomy: a prospective evaluation of 500 consecutive cases. Laryngoscope. 2005;115:1-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 132] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 8. | Cho YJ. Percutaneous dilatational tracheostomy. Tuberc Respir Dis (Seoul). 2012;72:261-274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Afolabi-Brown O, Marcus M, Speciale P, Pagala M, Kazachkov M. Bronchoscopic and nonbronchoscopic methods of airway culturing in tracheostomized children. Respir Care. 2014;59:582-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |