Published online Dec 2, 2021. doi: 10.5313/wja.v10.i2.7
Peer-review started: March 8, 2021
First decision: May 14, 2021
Revised: May 31, 2021
Accepted: October 15, 2021
Article in press: October 15, 2021
Published online: December 2, 2021
Processing time: 268 Days and 9.5 Hours
In anesthesia practice, orotracheal intubation remains the primary concern of the anesthesiologist. The introduction of video laryngoscopy (VL) has increased the success rate of orotracheal intubation; however, conflicting results have been reported regarding the usefulness of the current technique with VL in clinical practice.
To describe a modification to improve intubation with VL, followed by evaluation of the practice in vivo.
First, a mannequin trial was conducted with operators having different experience and background. Then, a retrospective analysis was performed for an > 1-year period with patients who underwent general anesthesia with orotracheal intubation. The endotracheal tube used had been pre-formed with two curves. Stepwise intubation had been performed with direct eye vision, followed by screen assistance and rotation of the tube as needed to direct it toward the glottis. In the mannequin trial, the outcome measures were quantification of torque (force with angular acceleration during levering), need for external maneuvers, and time to intubate. In the clinical experience, orotracheal intubation used VL (pre-formed tube) or direct laryngoscopy (DL) at the anesthetist’s discretion and throat discomfort was reported by the patient.
In the mannequin trials using VL, there was less torque with the pre-formed tube than with a regular tube (8% and 65%, respectively). The first-pass rate was higher with the pre-formed tube (95%) than with a regular tube (81%). However, the time to intubate was longer with the pre-formed tube than with a regular tube (22 s and 12 s, respectively). In clinical practice, 562 patients underwent surgery under general anesthesia with orotracheal intubation using either VL (n = 244) or DL (n = 318) at the discretion of the attending anesthetist. VL was specifically planned in 62 of the patients, due to anticipated difficulty. Second attempts by readjustment of the curve of the tube were significantly fewer with VL than with DL (10% vs 18%). Throat discomfort was reported by fewer patients who underwent VL than those who underwent DL (6% vs 24%).
Pre-formed endotracheal tube with stepwise insertion produces less torque, fewer external maneuvers and higher first-pass success rate during VL intubation. Further, prospective studies are warranted.
Core Tip: Video laryngoscopy (VL) is gaining popularity in the practice of endotracheal intubation. Failure of VL-assisted intubation may be attributed to the fact that practitioners use the same technique employed for traditional rigid laryngoscopy. We describe a technique based on pre-forming the endotracheal tube with two specific curves and using a stepwise insertion technique to facilitate the VL and achieve a higher success rate. The tool was tested in a mannequin trial first and then applied to clinical practice. The first-pass success rate was higher, with minimal torque and fewer external maneuvers required.
- Citation: Shorrab AA, Helal MA. Pre-formed endotracheal tube and stepwise insertion for more successful intubation with video laryngoscopy. World J Anesthesiol 2021; 10(2): 7-15
- URL: https://www.wjgnet.com/2218-6182/full/v10/i2/7.htm
- DOI: https://dx.doi.org/10.5313/wja.v10.i2.7
Successful tracheal intubation remains a major concern in anesthesia practice. Failure to intubate the trachea may be associated with serious complications, such as pulmonary aspiration and difficult mask ventilation, which may result in life-threatening hypoxia. Furthermore, repeated attempts at intubation may damage the upper airway and make mask ventilation more difficult. In fact, difficulty in tracheal intubation is the most common cause of serious airway complications during anes
However, despite VL providing adequate visualization of the larynx, difficulty in intubation and longer intubation times have been reported[1,6,7]. Attempts at improving the curve of the blade or manipulating the stylet as a lever to the epiglottis have been described[8]. We believe that one reason for longer times or intubation failures is that the practitioner uses the same strategy as in direct laryngoscopy (DL). The technical difficulty may be attributed to the fact that the vision axis obtained by the camera at the tip of the blade is usually different from the axis of the tracheal tube. Moreover, the tracheal tube itself and its cuff may obscure the glottis view because of the camera’s short-sight of the larynx and glottis.
In this study, we aimed to evaluate a new technique for improving the success rate of VL intubation. The technique includes a pre-formed tracheal tube for which a stepwise insertion technique is employed.
The study protocol was approved by the Ethics and Research Committee of University Hospital Sharjah (No. UHS-HERC-014-30072019). It was designed to describe a modification to improve intubation with VL followed by evaluation of its application in practice (in vivo). All patients who participated in the study provided informed consent and underwent general anesthesia for orotracheal intubation (see Video at: https://drive.google.com/file/d/1AWJubzMF6o0as4r9rVbncq2H-QZ1Twr_/view?usp=sharing).
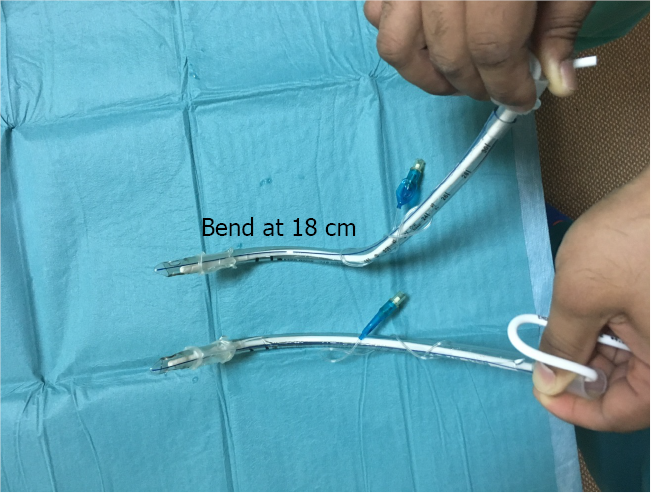
Two bends were created in the endotracheal tube, with the stylet in place. The first bend was made at the distal third, at 30° relative to the existing curve of the tube. The second bend was made between the middle and proximal thirds, at 30° clockwise. For adult applications, the two bends were located at approximately 9 cm and 18 cm, as shown in Figure 1.
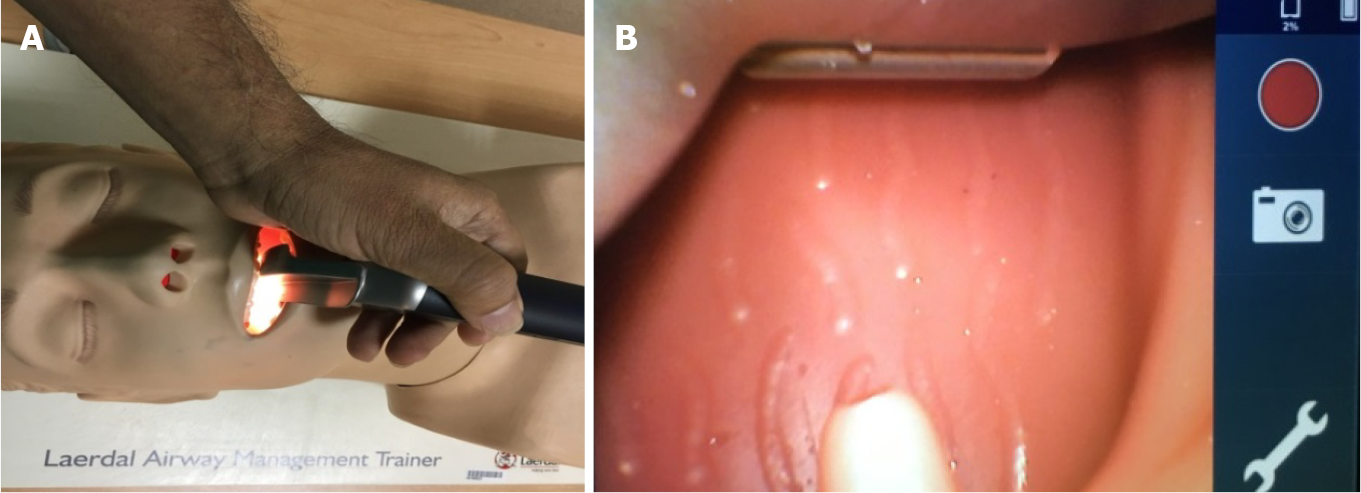
Step 1: Blade insertion, down to the base of the tongue, performed without looking at the video monitor screen (Figure 2).
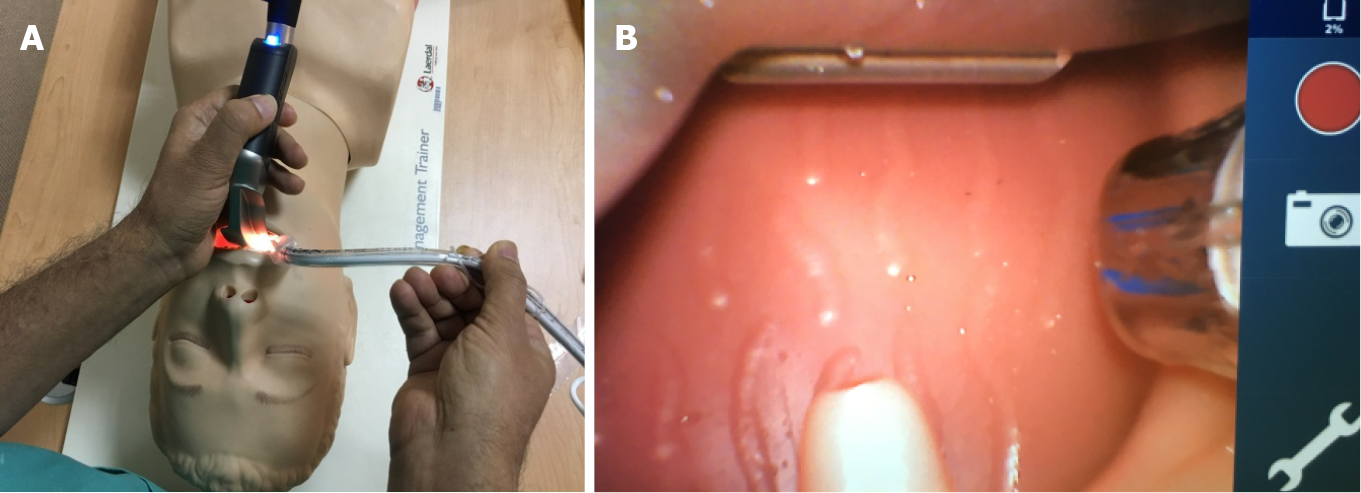
Step 2: Tube insertion, at the right corner of the mouth, to pass the pillars under direct vision and performed without looking at the video monitor screen; the distal angle is facing the angle of the mouth (Figure 3).
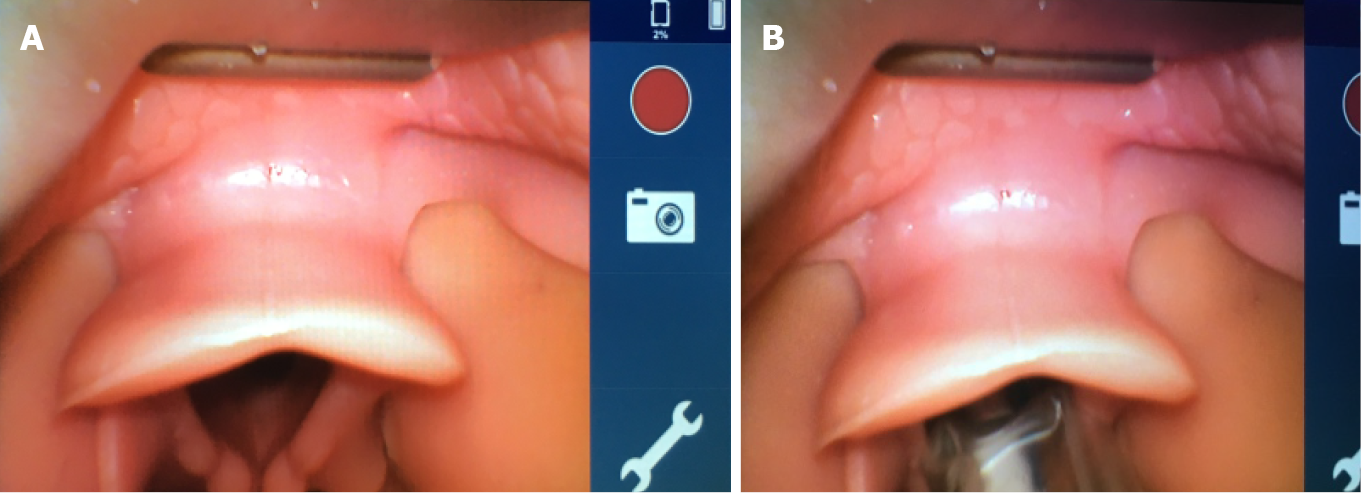
Step 3: Looking at the video monitor screen, the laryngoscope blade is advanced down to the epiglottis; then, gently passing the tube with counterclockwise rotation, as needed to intubate (Figure 4).
Step 4: As the tip of the tube passes the vocal cords, the stylet is removed with a gentle counter push to pass the cuff below the vocal cords.
The technique was first practiced by multiple operators on a mannequin and subsequently performed in clinical practice. In the mannequin trials, the outcome measures were quantification of torque, need for external maneuvers, and time to intubate. In clinical practice, the outcome measures were need for a second attempt and postoperative throat discomfort reported by the patients (data retrieved from patient records).
A commercially-available mannequin created for airway management (Laerdal® Airway Management Trainer; Laerdal Medical, Stavanger, Norway) and a C-MAC® video laryngoscope (Karl Storz SE & Co. KG, Tuttlingen, Germany) was used to practice the technique. A size-3 blade was used in both attempts. Twenty providers with varying experience levels and backgrounds in airway management (i.e., anesthesiologist, intensivist, and anesthesia technician) practiced the technique. The intubation method was explained and demonstrated by the 1st author (Shorrab AA), followed by hands-on practice by the participants. Then, for the study purpose, each participant performed three intubations with VL using a regular tube and three intubations with the pre-formed tube. The time to successful intubation and torque were recorded. Torque, defined as a force accompanied with angular acceleration during arm levering, was signified by a clicking sound coming from the joint articulating the jaw and head to the neck of the mannequin. The sound is audible when the force exceeds 8 pounds per square inch.
All cases scheduled for general anesthesia with endotracheal intubation over the year of 2019 were retrospectively analyzed. A total of 618 records were examined, of which 56 (9%) were excluded due to incomplete airway management documentation. The choice of airway management with either DL or VL had been made at the anesthetist’s discretion without prior randomization. The new VL technique had been employed in daily routine in patients with different demographic characteristics. The need for a second attempt at intubation had been recorded. Postoperative throat discomfort (reported by the patients) had also been recorded.
Because the clinical study was a retrospective, descriptive study covering almost 1 year of practice, the sample size had not been determined a priori. Considering that the new technique would increase the intubation rate success of 75% reported in the MACMAN trial[9] to 90%, setting the type I error at 5% and the type II error at 10%, the sample size of 562 patients collected over the study period was considered sufficient for meaningful statistics.
Categorical data were expressed as numbers and percentages, and continuous data were expressed as averages and ranges. Binary data were analyzed using a test for two proportions (Fisher’s exact test). Continuous data were analyzed using a two-sample t-test. An online calculator (https://statskingdom.com) was used for the analysis[10]. A P value of less than 0.05 was considered statistically significant.
In the mannequin trials, the time to intubate was longer with the pre-formed tube than with a regular tube. The first-pass success rate was higher with the pre-formed tube than with a conventional tube. More torque was exerted with DL than with VL (Table 1).
For the application in clinical practice, VL with the pre-formed tube was performed in 244 patients; in 62 of these patients, the VL had been specifically planned due to anticipated difficult intubation (Table 2). Second attempts by readjustment of the curve of the tube were significantly fewer with VL than with DL. Throat pain was reported by significantly fewer patients in the VL group than in the DL group (Table 3).
| Indication | n |
| Mallampati 4 | 9 |
| Micrognathia/receding mandible | 8 |
| Macroglossia | 4 |
| Abnormal dentation | 10 |
| Trisomy | 3 |
| Neck collar | 3 |
| Neck contracture | 2 |
| Neck osteoarthritis | 16 |
| BMI > 45 | 6 |
| Hemiglossectomy | 1 |
| Total | 62 |
With VL, the “can see the glottis but cannot intubate” scenario is still encountered. Challenges in the use of VL have been described, including the moment when the position of the tip of the tube cannot be confirmed during its insertion due to obscuration of the vision axis. Therefore, even when a clear view of the glottis is obtained on a video monitoring screen, it can often be difficult to direct the tube towards it, and the upper airway may be traumatized in this blind moment[1,2]. One reason for this is that practitioners are used to employing the same technical strategy used for DL.
During the practice on a mannequin, less torque was used with the pre-formed tube, as compared to that used with the conventional tube. The laryngoscopist who experiences difficulty will use more force, and torque will appear[11]. Direct stimulation of the extensively innervated oropharynx by the laryngoscope blade will increase the hemodynamic changes[12,13]. Excessive force and torque applied during DL will be associated with inadvertent damage to the teeth, oral cavity, and/or oropharynx[14,15].
The pre-formed tube with two curves described in this study proved to be efficient, in terms of both ease and intubation success with less torque. It has previously been reported that the C-MAC video laryngoscope provides a comparable or better glottic view than DL[16]. Strategies for enhancing the glottis view have also been described[17]; however, a good glottic view does not necessarily translate into greater intubation success. With our tool, the passage of the tube from the right lateral angle of the mouth offers room for better visualization, without obstructing the field of view. The double curves allow counterclockwise rotation and up-and-down movement of the tube tip, as required to reach the glottis. In patients with a non-visualized or partially visualized glottis opening, the styleted tube allows the anesthetist to lever the epiglottis with the distal tip of the tube, without the need for neck extension and with the least possible torque/force.
Our technique introduces a new way of using VL, including a pre-formed tube and a stepwise application to overcome the difficulties encountered in VL. Aziz et al[2] found that failure to intubate the trachea, despite achieving an adequate laryngeal view, occurred at a similar frequency with the C-MAC and with DL. In addition, VL is reported to have limited success and possible risks in both anesthetic[18] and intensive care[9,19] practices. The reason for first-pass endotracheal intubation failure is likely the difficulty in aligning the endotracheal tube with the orotracheal axis determined by the camera on the blade of the laryngoscope.
In our study, the time to intubate was significantly longer with VL than with DL. This is attributed to the careful insertion carried out in two stages: First, direct eye visualization, followed by video monitoring screen visualization. Additionally, the careful rotation of the tube during advancement increases the time to intubate. The time requested for intubation with the pre-formed tube was longer than that with the conventional tube. This may not be ideal during rapid sequence induction. However, it is useful in difficult scenarios, where adequate pre-oxygenation can ensure normoxia throughout the intubation period. However, none of the patients in our study were desaturated during intubation. Previous studies on VL have reported slightly longer intubation times compared with DL[2,20]. Moreover, as the practitioner progresses along the learning curve, the time to intubate is expected to become shorter.
With our technique in clinical practice, the rate of second attempts was approximately 10%, which was significantly lower than that with DL (18%). Previous studies have reported fewer external maneuvers required and less frequent need for a bougie with VL than with DL[2,21].
In practice, patient feedback on anesthesia experience includes the report of throat discomfort. In our study, significantly fewer patients reported throat discomfort with VL than with DL. The less torque and the stepwise insertion of the tube under direct vision followed by screen guidance may have caused a milder trauma to the oropharyngeal structures, resulting in less throat discomfort. Less force during intubation with VL than with DL practiced on mannequins by operators with varying experience has also been reported[22]. Therefore, we speculate that throat discomfort, stress during intubation, and cardiovascular responses are less severe with our technique.
In this cohort, VL was planned for 62 patients due to anticipated difficulty in airway management. We opted for VL in cases of difficult intubation based on previous reported experiences[23,24] and on the encouraging results of our mannequin trials.
A limitation of our study is that it was neither randomized nor blinded. The airway management decision was made at the anesthesia providers’ discretion, except in patients with expected difficulty, for whom VL was planned for safety reasons. However, the personnel collecting the data were not involved in the procedure. Another limitation is that the clinical portion of our study was not prospective, which would have allowed for comparison of the pre-formed and conventional endotracheal tube during VL. The underlying reason for this was that we considered an ethical obligation to apply the best practice of intubation to patients, without subjecting them to randomization. One more potential limitation is interoperator variability. However, including operators with various experience levels and backgrounds might mimic the real-world practice of airway management. In this study, comparisons between the traditional VL technique and the new VL technique concerned only the mannequin trials, whereas in clinical practice, the new VL technique was compared to DL, not to the conventional VL technique. Future randomized studies could be conducted on VL to compare the proposed technique to the conventional one.
In conclusion, the use of a pre-formed endotracheal tube and a combination of direct vision and video monitoring screen guidance, with careful rotation of the tracheal tube, is associated with less torque and fewer external maneuvers. The technique carries potential for a higher first-pass success rate and less postoperative throat discomfort. VL requires special tactics, however, different from those used in DL, and may warrant training and orientation. Prospective studies are also warranted.
Despite the wide use of video laryngoscopy (VL) for intubation, conflicting results have been reported regarding its usefulness. A new technique was introduced with the aim of improving the success rate of VL intubation. This technique includes pre-forming the tracheal tube, followed by a stepwise insertion process during VL intubation.
The “can see but can’t intubate” scenario is frequently reported during intubation with VL. We believe that the new technique will provide room for better manipulation of the tracheal tube, providing higher first pass rate and allowing for use of less force. In the future, a pre-formed tube with memory to negotiate for intubation could be introduced for more convenient and successful practice.
The objective of the study was to increase the success of intubation during VL.
First, a mannequin trial was conducted with operators having different experience levels and backgrounds. Then, a retrospective analysis was performed for an > 1-year period with patients who underwent general anesthesia with orotracheal intubation. The endotracheal tube used had been pre-formed with two curves, which was then applied in a stepwise intubation process with direct eye vision, followed by screen assistance to direct it toward the glottis. In the mannequin trial, the outcome measures were quantification of torque (force with angular acceleration during levering), need for external maneuvers, and time to intubate. In the clinical experience, orotracheal intubation used VL (pre-formed tube) or direct laryngoscopy (DL) at the anesthetist’s discretion, and throat discomfort was reported by the patient.
In the mannequin trials using VL, there was less torque required and a higher first pass rate achieved with the pre-formed tube than with a regular tube. In clinical practice, second attempts by readjustment of the curve of the tube were significantly fewer with VL than with DL, and throat discomfort was reported by fewer patients who underwent VL.
The use of a pre-formed endotracheal tube and a combination of direct vision and video monitoring screen guidance, with careful rotation of the tracheal tube, is associated with less torque and fewer external maneuvers. The technique carries potential for a higher first-pass success rate and less postoperative throat discomfort. Nonetheless, VL requires special tactics and may warrant training and orientation.
The authors thank Ms. Lorenzo MM for recording the photographic and video data. The authors also thank anesthesia technicians Mr. Khalid AA and Mr. Varghese B for their assistance in setting up the equipment and recording the data.
Provenance and peer review: Invited article; Externally peer reviewed.
Corresponding Author's Membership in Professional Societies: the Emirates Medical Association; Member of The Egyptian Society of Anesthesiologists; the European Society of Enteral and Parenteral Nutrition (ESPEN); and the Clinical Governance in Dubai Health Authority.
Specialty type: Anesthesiology
Country/Territory of origin: United Arab Emirates
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gajic O S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Cook TM, Woodall N, Frerk C; Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011;106:617-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1171] [Cited by in RCA: 1243] [Article Influence: 88.8] [Reference Citation Analysis (1)] |
| 2. | Min BC, Park JE, Lee GT, Kim TR, Yoon H, Cha WC, Shin TG, Song KJ, Park M, Han H, Hwang SY. C-MAC Video Laryngoscope versus Conventional Direct Laryngoscopy for Endotracheal Intubation During Cardiopulmonary Resuscitation. Medicina (Kaunas). 2019;55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Fiadjoe JE, Gurnaney H, Dalesio N, Sussman E, Zhao H, Zhang X, Stricker PA. A prospective randomized equivalence trial of the GlideScope Cobalt® video laryngoscope to traditional direct laryngoscopy in neonates and infants. Anesthesiology. 2012;116:622-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 83] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Orser BA. Recommendations for Endotracheal Intubation of COVID-19 Patients. Anesth Analg. 2020;130:1109-1110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 131] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 5. | Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67:568-576. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 658] [Cited by in RCA: 608] [Article Influence: 121.6] [Reference Citation Analysis (0)] |
| 6. | Aziz M, Brambrink A. The Storz C-MAC video laryngoscope: description of a new device, case report, and brief case series. J Clin Anesth. 2011;23:149-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Byhahn C, Iber T, Zacharowski K, Weber CF, Ruesseler M, Schalk R, Meininger D. Tracheal intubation using the mobile C-MAC video laryngoscope or direct laryngoscopy for patients with a simulated difficult airway. Minerva Anestesiol. 2010;76:577-583. [PubMed] |
| 8. | Hung TY, Lin LW, Yeh YH, Su YC, Lin CH, Yang TF. The evaluation of a better intubation strategy when only the epiglottis is visible: a randomized, cross-over mannequin study. BMC Anesthesiol. 2019;19:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Lascarrou JB, Boisrame-Helms J, Bailly A, Le Thuaut A, Kamel T, Mercier E, Ricard JD, Lemiale V, Colin G, Mira JP, Meziani F, Messika J, Dequin PF, Boulain T, Azoulay E, Champigneulle B, Reignier J; Clinical Research in Intensive Care and Sepsis (CRICS) Group. Video Laryngoscopy vs Direct Laryngoscopy on Successful First-Pass Orotracheal Intubation Among ICU Patients: A Randomized Clinical Trial. JAMA. 2017;317:483-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 171] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 10. | Statistics Kingdom. Statistics online. Test statistic calculators. [cited 13 January 2020]. Available from: www.statskingdom.com. |
| 11. | McCoy EP, Austin BA, Mirakhur RK, Wong KC. A new device for measuring and recording the forces applied during laryngoscopy. Anaesthesia. 1995;50:139-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Stoelting RK. Circulatory changes during direct laryngoscopy and tracheal intubation: influence of duration of laryngoscopy with or without prior lidocaine. Anesthesiology. 1977;47:381-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 200] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Xue FS, Zhang GH, Li XY, Sun HT, Li P, Li CW, Liu KP. Comparison of hemodynamic responses to orotracheal intubation with the GlideScope videolaryngoscope and the Macintosh direct laryngoscope. J Clin Anesth. 2007;19:245-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Hastings RH, Hon ED, Nghiem C, Wahrenbrock EA. Force, torque, and stress relaxation with direct laryngoscopy. Anesth Analg. 1996;82:456-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Gaudio RM, Feltracco P, Barbieri S, Tiano L, Alberti M, Delantone M, Ori C, Avato FM. Traumatic dental injuries during anaesthesia: part I: clinical evaluation. Dent Traumatol. 2010;26:459-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Cavus E, Thee C, Moeller T, Kieckhaefer J, Doerges V, Wagner K. A randomised, controlled crossover comparison of the C-MAC videolaryngoscope with direct laryngoscopy in 150 patients during routine induction of anaesthesia. BMC Anesthesiol. 2011;11:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Sulser S, Ubmann D, Schlaepfer M, Brueesch M, Goliasch G, Seifert B, Spahn DR, Ruetzler K. C-MAC videolaryngoscope compared with direct laryngoscopy for rapid sequence intubation in an emergency department: A randomised clinical trial. Eur J Anaesthesiol. 2016;33:943-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 67] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 18. | Niforopoulou P, Pantazopoulos I, Demestiha T, Koudouna E, Xanthos T. Video-laryngoscopes in the adult airway management: a topical review of the literature. Acta Anaesthesiol Scand. 2010;54:1050-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 214] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 19. | Gao YX, Song YB, Gu ZJ, Zhang JS, Chen XF, Sun H, Lu Z. Video versus direct laryngoscopy on successful first-pass endotracheal intubation in ICU patients. World J Emerg Med. 2018;9:99-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Sun DA, Warriner CB, Parsons DG, Klein R, Umedaly HS, Moult M. The GlideScope Video Laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth. 2005;94:381-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 246] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 21. | Platts-Mills TF, Campagne D, Chinnock B, Snowden B, Glickman LT, Hendey GW. A comparison of GlideScope video laryngoscopy versus direct laryngoscopy intubation in the emergency department. Acad Emerg Med. 2009;16:866-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 90] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 22. | Goto T, Koyama Y, Kondo T, Tsugawa Y, Hasegawa K. A comparison of the force applied on oral structures during intubation attempts between the Pentax-AWS airwayscope and the Macintosh laryngoscope: a high-fidelity simulator-based study. BMJ Open. 2014;4:e006416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | El-Tahan MR, El Kenany S, Khidr AM, Al Ghamdi AA, Tawfik AM, Al Mulhim AS. Cervical spine motion during tracheal intubation with King Vision™ video laryngoscopy and conventional laryngoscopy: a crossover randomized study. Minerva Anestesiol. 2017;83:1152-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Maassen R, Lee R, van Zundert A, Cooper R. The videolaryngoscope is less traumatic than the classic laryngoscope for a difficult airway in an obese patient. J Anesth. 2009;23:445-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |