Published online Sep 18, 2018. doi: 10.5312/wjo.v9.i9.138
Peer-review started: February 10, 2018
First decision: March 9, 2018
Revised: May 20, 2018
Accepted: May 23, 2018
Article in press: May 23, 2018
Published online: September 18, 2018
Processing time: 218 Days and 15.2 Hours
To present our results on the use of a single rod instrumentation correction technique in a small number of patients with major medical co-morbidities.
This study was a prospective single surgeon series. Patients were treated with single rod hybrid constructs and had a minimum 2-year follow-up. Indications included complex underlying co-morbidities, conversion of growing rods to definitive fusion, and moderate adolescent idiopathic primarily thoracic scoliosis with severe eczema and low body mass index (BMI).
We included 99 consecutive patients. Mean age at surgery was 12.8 years (SD 3.5 years). Mean scoliosis correction was 62% (SD 15%) from 73° (SD 22°) to 28° (SD 15°). Mean surgical time was 153 min (SD 34 min), and blood loss was 530 mL (SD 327 mL); 20% BV (SD 13%). Mean clinical and radiological follow-up was 3.2 years (range: 2-12) post-operatively. Complications included rod failure, which occurred in three of our complex patients with severe syndromic or congenital kyphoscoliosis (3%). Only one of these three patients required revision surgery to address a non-union. Our revision rate was 2% (including a distal junctional kyphosis in a Marfan’s syndrome patient).
The single rod technique has achieved satisfactory deformity correction and a low rate of complications in patients with specific indications and severe underlying medical conditions. In these children with significant co-morbidities, where the risks of scoliosis surgery are significantly increased, this technique has achieved low operative time, blood loss, and associated surgical morbidity.
Core tip: We reviewed 99 pediatric patients treated for scoliosis with a single-rod hybrid technique. They belonged in three groups: Group A included 62 patients with complex deformities and low body mass index (BMI) associated with medical co-morbidities increasing the risk of cardiac, respiratory, neurological complications and intra-operative blood loss; group B included 21 patients treated with growing rod lengthenings who underwent spinal fusion; group C included 16 patients with moderate adolescent idiopathic scoliosis, low BMI, and severe eczema at risk of wound or systemic infection. The single-rod technique has achieved and maintained at follow-up good deformity correction with low surgical time, blood loss, and surgical morbidity.
- Citation: Tsirikos AI, Loughenbury PR. Single rod instrumentation in patients with scoliosis and co-morbidities: Indications and outcomes. World J Orthop 2018; 9(9): 138-148
- URL: https://www.wjgnet.com/2218-5836/full/v9/i9/138.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i9.138
Dual rod instrumentation has become the standard of care for scoliosis correction. The use of bilateral segmental pedicle screw fixation over two rods can produce effective coronal and axial deformity correction and a stable construct whilst fusion occurs[1-3]. In most surgical techniques, the majority of curve correction occurs during placement of the first rod with the second rod providing additional stability in the post-operative period while the bone grafts are healing. Use of a single rod construct may offer theoretical advantages, including shorter surgical time, lesser blood loss, lower rates of infection, technically easier procedures, simpler pre-operative planning, lower instrumentation profile, and reduced implant cost. There is only one direct comparison of single and double rod instrumentation in the treatment of adolescent idiopathic scoliosis (AIS). This demonstrates superiority of the double rod technique and a higher rate of rod breakage with single rods (21% compared to 4% with double rods)[4]. Mechanical testing of single-rod and double-rod segmental hook fixation constructs with hooks at every level except the apex in a long-segment animal model (calf spines) indicated that over 12 vertebral segments the single rod instrumentation allowed more neutral zone rotation than the double rod construct[5]. There remains interest in using a single rod technique in high-risk patients, such as children with Duchenne muscular dystrophy (DMD), in order to minimize duration and morbidity of surgery[6].
This study reports a prospective series of patients treated by a single surgeon with a single rod hybrid technique in an effort to reduce peri-operative morbidity. The indications for use of this technique are discussed and the post-operative clinical, radiological, and functional outcomes are reported.
We reviewed 99 patients who underwent surgical correction of scoliosis using a single rod hybrid technique between 2005 and 2015. Indications for this technique over the traditional dual rod construct which is the standard of care in our practice, included high risk of neurological/cardiac complications and intra-operative bleeding, low body mass index (BMI), previous partial fusion due to long-term use of growing rods, and pre-existing severe eczema. Eighty-seven patients underwent posterior and 12 patients with early onset scoliosis (10 idiopathic - 2 syndromic) combined one-stage anterior/posterior spinal fusion. Operative data included surgical time, blood loss (recorded as a volume and percentage of body weight [percentage by volume - blood volume]), and problems related to intra-operative neuro-monitoring. Radiographs were examined pre-operatively to include curve severity (using the Cobb method[7]), skeletal maturity (Risser grade[8]), and location of curve apex[9]. Clinical and radiological review was performed post-operatively at mean follow-up 3.2 years (range: 2-12). Patient reported outcomes (Scoliosis Research Society-22 questionnaire) were available for patients with AIS before and after surgery. Statistical analysis was made using standard descriptive terms and the Microsoft Excel for Mac 2016 (Microsoft, Redmond, WA, United States).
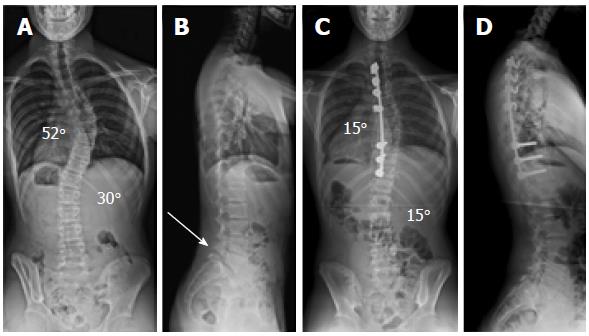
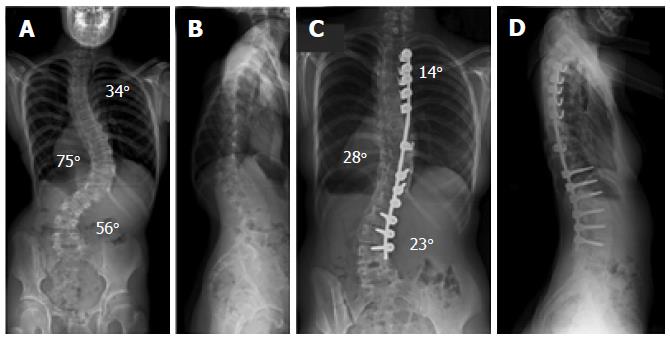
Anesthetic management included non-invasive monitoring, use of an arterial line, and urinary catheter. A warming blanket was also used, and our patients received prophylactic cefuroxime on induction and two further doses post-operatively. Blood loss was reduced with intra-operative tranexamic acid and transfusion of autologous blood using cell salvage. Multimodal spinal cord monitoring was applied recording cortical and cervical somatosensory (SSEPs), as well as transcranial motor evoked potentials (MEPs) that remained stable in all patients throughout the procedure. Anterior release was performed through a convex thoracotomy in 12 patients. All patients underwent posterior correction across the thoracic or thoracic/lumbar spine short of the sacrum and pelvis through a midline incision with bilateral subperiosteal exposure to the tips of the transverse processes. Soft tissue release and facetectomies were performed, and correction was achieved with a single rod. This was secured using distal pedicle screws, proximal pedicle hooks, and transverse process hooks or sublaminar wires at the apex of the curve. Scoliosis correction was achieved either through concave rod derotation and apical translation towards the midline (Figure 1) or through apical translation and convex rod cantilever maneuver from proximal to distal (Figure 2). The Universal Spinal System (USS) instrumentation was used (DePuy/Synthes, West Chester, Pennsylvania, United States) in all patients. Decortication of the posterior elements and use of autologous local and allograft bone (fresh frozen femoral heads) aimed to achieve a solid fusion. Autologous rib graft was used when an anterior release was performed. In six patients who underwent posterior surgery, additional iliac crest graft was used. Topical vancomycin (1 g) was applied prior to closure. The wound was closed in layers without wound drains. Mobilization commenced on the first post-operative day and patients were fitted with a custom-molded removable underarm spinal jacket to wear when out of bed for 6 mo after surgery.
The cost of our typical construct used in AIS was considered for both a thoracic (mean 10 instrumented levels) and a double thoracic/lumbar fusion (mean 15 instrumented levels). For a thoracic fusion, our single rod construct included three proximal pedicle screw hooks, three distal pedicle screws, one transverse process hook, and a single rod (Figure 1). For a thoracic and lumbar fusion, our single rod construct included maximum five proximal pedicle screw hooks, six distal pedicle screws, one transverse process hook, and a single rod (Figure 2). This was then compared to a double rod construct using bilateral segmental pedicle screws (implant density: 2) and a double rod construct using the authors’ preferred technique with reduced implant density 1.38[10]. All costs were calculated using standard prices for USS instrumentation and reported as percentage decrease in cost.
Mean age at surgery was 12.8 years [standard deviation (SD) 3.5 years]. Mean surgical time was 153 min (SD 34 min), and mean blood loss was 530 mL (SD 327 mL); 20% blood volume (BV) (SD 13%). Three patient groups were included:
This group included 62 complex patients with severe deformities and associated co-morbidities (Tables 1-3 and Figure 2). Underlying scoliosis diagnosis included syndromic (21 patients, Table 3), early onset idiopathic (17 patients; juvenile: 9, infantile: 8), congenital (13 patients), neuromuscular (5 patients; congenital myopathy: 1, cerebral palsy: 1, demyelinating neuropathy: 1, Friedreich’s ataxia: 1, congenital hypotonia: 1), and scoliosis associated with intraspinal anomalies (6 patients; Chiari I malformation with syringomyelia: 4, astrocytoma: 1, gaglioglioma: 1). Indications to use the single rod technique were high risk of neurological/cardiac complications, complex congenital vertebral anomalies, increased intra-operative bleeding, and low BMI. In the syndromic patients, mean scoliosis correction was 65% for upper thoracic, 62% for main thoracic, and 56% for lumbar curves (P < 0.001), surgical time was 164 min (SD 47 min), and blood loss was 27% BV (SD 13%). In the congenital patients, mean scoliosis correction was 54% for upper thoracic, 50% for main thoracic, and 48% for lumbar curves (P < 0.001), surgical time was 138 min (SD 29 min), and blood loss was 13% BV (SD 3%). In the early onset idiopathic group, mean scoliosis correction was 62% for upper thoracic, 60% for main thoracic, and 61% for lumbar curves (P < 0.001), surgical time was 185 min (SD 101 min), and blood loss was 25% BV (SD 16%). In the neuromuscular patients, mean scoliosis correction was 66% for main thoracic and 57% for lumbar curves (P < 0.001), surgical time was 125 min (SD 13 min), and blood loss was 24% BV (SD 11%). In the intraspinal anomalies group, all patients had a thoracic scoliosis. Mean curve correction was 56% (P < 0.001), surgical time was 145 min (SD 17 min), and blood loss was 22% BV (SD 11%).
| Group | Type of scoliosis | No. ofpatients | Mean age at surgery (yr) | Procedure (No. of patients) | Operatingtime (min) | Blood loss(mL) | Bloodloss (BV) | Mean follow-up (yr) | Complications |
| A - Complex deformity | Syndromic | 21 | 13 | PSF: 19; A/PSF: 2 | 164 | 727 | 27 | 3.0 | 2 rod breakages-one revision required due to non-union; 1 distal junctional kyphosis-distal fusion extension required |
| Early onset idiopathic | 17 | 11 | PSF: 11; A/PSF: 6 | 185 | 519 | 25 | 2.9 | None | |
| Congenital | 13 | 11 | PSF: 13 | 138 | 368 | 13 | 4.8 | One rod breakage-no revision required | |
| Neuromuscular | 5 | 14 | PSF: 5 | 125 | 662 | 24 | 3.0 | None | |
| Intraspinal anomalies | 6 | 13 | PSF: 6 | 145 | 525 | 22 | 4.5 | None | |
| B - Conversion of growing rods to definitive fusion | Early onset | 21 | 12 | PSF: 17; A/PSF: 4 | 159 | 497 | 20 | 2.8 | None |
| C - AIS | Adolescent idiopathic | 16 | 15.8 | PSF: 16 | 128 | 406 | 9 | 2.8 | None |
| Summary of data | 99 | 13 | PSF: 87; A/PSF: 12 | 153 | 530 | 20 | 3.2 | 4 |
| Group | Type of scoliosis | No. of patients | Thoracic scoliosis (meanpreop/postop; degrees);(%correction) | Double thoracic scoliosis(mean preop/postop;degrees); (%correction) | Thoracic/lumbar scoliosis(mean preop/postop; degrees);(%correction) | Triple thoracic/lumbar scoliosis(mean preop/postop; degrees);(%correction) | Thoracic kyphoscoliosis(mean preop/postop;degrees); (%correction) |
| A – Complex deformity | Syndromic | 21 | 78/30 (62%); 8 patients | Upper TH: 46/19 (59%) main TH: 60/24 (60%); 5 patients | TH: 55/18 (67%) L: 43/15 (65%); 4 patients | Upper TH: 32/6 (81%) main TH: 61/28 (54%) L: 52/25 (52%); 2 patients | Scoliosis: 120/48 (60%) kyphosis: 103/60 (42%); 2 patients |
| Early onset idiopathic | 17 (infantile: 9; juvenile: 8) | 99/34 (66%); 4 patients | Upper TH: 53/25 (53%) main TH: 81/47 (42%); one patient | TH: 89/36 (60%) L: 70/27 (61%); 6 patients | Upper TH: 49/15 (69%) main TH: 84/30 (64%) L: 52/20 (62%); 5 patients | Scoliosis: 56/31 (45%) kyphosis: 122/65 (47%); one patient | |
| Congenital | 13 | 58/36 (38%); 6 patients | Upper TH: 39/22 (44%) main TH: 76/40 (47%); 2 patients | TH: 75/38 (49%) L: 68/36 (47%); 3 patients | Upper TH: 41/15 (63%) main TH: 55/25 (55%) L: 44/22 (50%); one patient | Scoliosis: 70/31 (56%) kyphosis: 75/35 (53%); one patient | |
| Neuromuscular | 5 | 66/19 (71%); 2 patients | - | TH: 79/31 (61%) L: 65/28 (57%); 3 patients | - | - | |
| Associated with intraspinal anomalies | 6 | 82/36 (56%); 6 patients | - | - | - | ||
| B – Conversion of growing rods to definitive fusion | Syndromic | 10 | 91/39 (57%); 6 patients | - | TH: 93/52 (44%) L: 69/37 (46%); 4 patients | - | - |
| Infantile idiopathic | 6 | 74/28 (62%); 2 patients | Upper TH: 59/34 (42%) main TH: 100/55 (45%); one patient | TH: 61/38 (38%) L: 101/52 (49%); one patient | - | Scoliosis: 63/32 (49%) kyphosis: 104/61 (41%); 2 patients | |
| Congenital | 4 | 77/38 (51%); 4 patients | - | - | - | - | |
| Neuromuscular | 1 | - | - | - | - | Scoliosis: 65/25 (62%) kyphosis: 78/50 (36%); one patient |
| Group A – Complex deformity (n = 21 patients) | Group B - Conversion of growing rods to definitive fusion (n = 10 patients) |
| Neurofibromatosis type 1 (2) | Skeletal dysplasia (2) |
| Osteogenesis imperfecta (1) | Oculo-auriculo-fronto-nasal syndrome (1) |
| Rubinstein-Taybi type 2 (1) | Chromosome abnormality (7) |
| Cystic Fibrosis (1) | |
| Arthrogryposis multiplex congenital (1) | |
| Ehlers-Danlos (1) | |
| Angelman’s (1) | |
| Marfan’s (1) | |
| Prader-Willi (1) | |
| Down’s syndrome (1) | |
| Chromosome abnormality (4) | |
| Undiagnosed syndromic condition (6) |
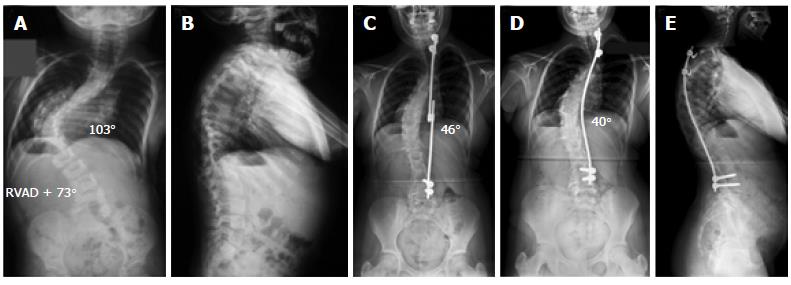
There were 21 patients where a single rod was used to achieve final correction and definitive fusion at the end of treatment with growing rod lengthenings (Tables 1-3 and Figure 3). Underlying cause of scoliosis included syndromic (10 patients), infantile idiopathic (6 patients), congenital (4 patients), and neuromuscular (horizontal gaze palsy: 1 patient). Indications for using the single rod technique were the presence of partial fusion and inherent stiffness of the spine due to the long-standing deformity, anterior apical convex epiphysiodesis (9 patients), and several previous growing rod lengthenings in order to achieve a globally balanced spine, low BMI, and a high risk of complications due to existing co-morbidities. Twelve patients had single thoracic, five had thoracic and lumbar, and one had double thoracic scoliosis while three patients had thoracic kyphoscoliosis. Mean scoliosis correction was 42% for upper thoracic, 52% for main thoracic, and 47% for lumbar curves (P < 0.001), surgical time was 159 min (SD 86 min), and blood loss was 20% BV (SD 13%).
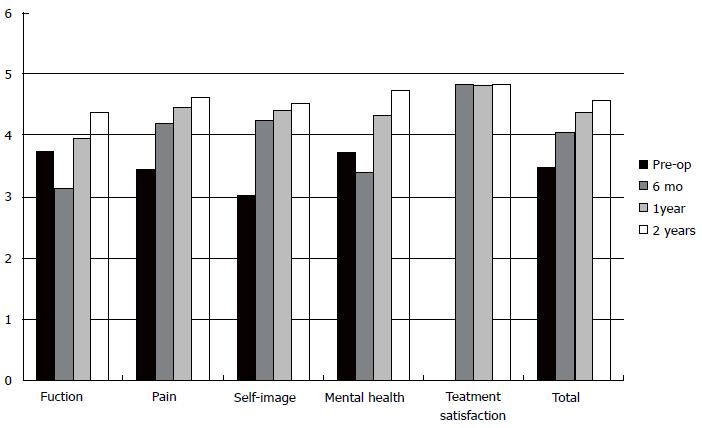
The single rod technique was used in 16 patients with AIS (Tables 1 and 4). Indications for the single rod technique were pre-existing severe eczema increasing significantly the risk of wound infection and low BMI. Fifteen patients had moderate single or double thoracic scoliosis with compensatory lumbar curves (12 patients), and one patient had a double thoracic and lumbar scoliosis. Mean flexibility index {FI, % = [(pre-operative Cobb angle – supine maximum lateral bending Cobb angle)/preoperative Cobb angle] × 100} as calculated before surgery was 25% (range: 22%-35%) for upper thoracic, 30% (range: 10%-59%) for main thoracic, and 50% (range: 35%-62%) for lumbar curves. Mean correction was 64% for upper thoracic, 70% for main thoracic, and 67% for lumbar curves (P < 0.001), surgical time was 128 min (SD 20 min), and blood loss was 9% BV (SD 5%). When compared to our previous AIS series of segmental bilateral (mean surgical time: 320 min; mean blood loss: 50% BV)[10], segmental unilateral (mean surgical time: 240 min; mean blood loss: 30% BV)[10], or segmental convex (mean surgical time: 183 min; mean blood loss: 22% BV)[11] pedicle screw correction techniques, both surgical time and intra-operative blood loss in the single rod technique was significantly reduced (P < 0.001). Excellent correction of global coronal and sagittal balance, including thoracic kyphosis and lumbar lordosis, was also achieved. This was associated with high patient satisfaction (4.8 at latest follow-up) and good functional outcomes (Figure 4).
| Patientnumber | Gender | Risser grade | Scoliosis type(No. ofpatients)[9] | Procedure(posterior spinalfusion/levels) | Upper thoracic scoliosis(pre-op/post-op;degrees); (% correction) | Main thoracic scoliosis(pre-op/post-op;degrees); (% correction) | Lumbar scoliosis (pre-op/post-op; degrees);(%correction) | Kyphosis (pre-op/post-op);(degrees) | Lordosis (pre-op/post-op);(degrees) | Coronal balance(pre-op/post-op);(cm) | Sagittal balance (pre-op/post-op); (cm) |
| 1 | F | 5 | 2A | PSF T2-T10 | 52/23 (56%) | 49/22 (55%) | - | 19/52 | 49/52 | 0/0 | -3.5/0 |
| 2 | F | 5 | 1B | PSF T3-T11 | - | 48/15 (69%) | 35/17 (51%- spontaneous correction) | 27/52 | 47/53 | 0.3/0 | -2.8/0 |
| 3 | M | 2 | 2A | PSF T2-L1 | 32/11 (66%) | 47/11 (77%) | - | 35/44 | 40/42 | 0.8/0 | -0.8/0 |
| 4 | F | 4 | 1A | PSF T2/T9 | - | 45/0 (100%) | - | 45/55 | 55/58 | 2.3/0 | -0.3/0 |
| 5 | M | 5 | 2A | PSF T2-T11 | 32/12 (62.5%) | 52/16 (69%) | 30/6 (80%-spontaneous correction) | 23/44 | 59/45 | 0.8/0 | -3.1/0 |
| 6 | F | 5 | 3C | PSF T2-L4 | - | 55/12 (78%) | 48/10 (79%) | 25/50 | 40/50 | 1.2/0 | -2.8/0 |
| 7 | F | 5 | 2B | PSF T3-T12 | 35/12 (66%) | 55/21 (62%) | 36/11 (69%-spontaneous correction) | 28/48 | 50/50 | 1/0 | -3.0/0 |
| 8 | M | 4 | 1A | PSF T2-T12 | - | 60/15 (75%) | 39/10 (74%-spontaneous correction) | 16/38 | 43/42 | 0/0 | 1.5/0 |
| 9 | F | 3 | 2A | PSF T3-T12 | 29/9 (69%) | 48/14 (71%) | 30/2 (93%-spontaneous correction) | 17/38 | 33/38 | 0.6/0 | -1.2/0 |
| 10 | F | 3 | 1A | PSF T2-T11 | - | 52/20 (61.5%) | 36/15 (58%-spontaneous correction) | 24/46 | 61/51 | 0/0 | -2.5/0 |
| 11 | M | 5 | 1B | PSF T2-T11 | - | 55/16 (71%) | 30/15 (50%-spontaneous correction) | 20/48 | 47/50 | 3.5/0 | 4.1/0 |
| 12 | F | 4 | 2A | PSF T3-T12 | 32/11 (66%) | 59/17 (71%) | 32/13 (59%-spontaneous correction) | 46/48 | 57/46 | 0.8/0.2 | -3.5/-1 |
| 13 | M | 4 | 1A | PSF T2-T11 | - | 52/15 (71%) | 30/15 (50%-spontaneous correction) | 20/47 | 48/46 | 3/0 | 3.5/0 |
| 14 | F | 5 | 2B | PSF T2-T11 | 42/15 (64.3%) | 60/25 (58.3%) | 40/14 (65%-spontaneous correction) | 31/48 | 46/47 | 1.2/0.5 | -2.3/0 |
| 15 | F | 4 | 2A | PSF T3-T12 | 39/14 (64%) | 69/23 (67%) | 37/14 (62%-spontaneous correction) | 31/47 | 45/50 | 0.5/0 | -0.5/0 |
| 16 | F | 3 | 2A | PSF T3-L2 | 22/8 (64%) | 59/20 (66%) | 28/9 (68%-spontaneous correction) | 56/54 | 54/53 | 2.5/0.3 | 2.2/0 |
| Summary of data | 11 F; 5 M | Mean: 4.1 | Scoliosis type 1 (1); 2 (2); 3 (6); 4 (7) | 15 TH fusions; one TH/L fusion | Mean values: 35/12.7 (64%) | Mean values: 54/16 (70.4%) | Mean values: 35/11.6 (67%) | Mean values: 29/47.4 (63.4%) | Mean values: 48/48 no change | Mean values: 1.16/0.06 (95%) | Mean values: 2.35/0.06 (97.4%) |
We compared the single-rod and dual-rod techniques in our practice and did not record significant difference in the degree of scoliosis correction for main thoracic curves, which was the primary deformity among the patients included in our single rod series of 16 AIS patients (P > 0.05)[10,11]. However, the degree of preoperative thoracic scoliosis was significantly greater (P < 0.001) among the patients included in our cohorts treated with segmental pedicle screws and a dual rod construct (bilateral technique-mean scoliosis: 68°, range: 40°-98°; unilateral technique-mean scoliosis: 65°, range: 38°-95°; convex technique-mean scoliosis: 70.2°, range: 55°-110°) when compared to our single rod AIS group (mean scoliosis: 54°, range: 45°-69°)[10,11]. SRS-22 individual domain and total scores, as well as patients’ satisfaction at 2-year follow-up between single-rod and dual-rod constructs, was also no different (P > 0.05)[10,11].
We recorded four post-operative complications (4%) that occurred in three patients with syndromic kyphoscoliosis and in a patient with a congenital kyphoscoliosis (group A). Three of these complications involved rod failure. The first was the result of a non-union presenting with rod breakage occurring 17 mo after surgery. This patient had chromosomal abnormality, complex cardiac disease, poor skin healing, and severe behavioral problems. She had a thoracic scoliosis corrected from 120° to 35° through a combined anterior/posterior fusion and associated thoracic hyperkyphosis. Revision posterior surgery was performed to address a hairline non-union using a new rod and the existing fixation points. The fusion was augmented with autologous rib and allograft bone with a good outcome at skeletal maturity. The other two rod failures occurred in a patient with syndromic and another with congenital kyphoscoliosis and presented 3 years after index surgery. Both patients were asymptomatic, and there was no radiographic evidence of recurrence of the deformity. The two opposing ends of the rod were undisplaced at the point of failure, and a computed tomography (CT) scan confirmed a solid fusion across the previously instrumented levels. Therefore, revision surgery was not required, and the patients remained pain-free with a full range of activities and a stable residual deformity at subsequent follow-up. The fourth patient had Marfan’s syndrome, intraspinal anomalies, and severe cardiac disease. Following index posterior correction, she developed distal junctional kyphosis. Revision surgery to extend the fusion by two caudal levels resulted in a good outcome at end of skeletal growth. Our revision rate was 2% (1% each for rod breakage and distal junctional kyphosis).
Analysis of the instrumentation costs used to treat thoracic and thoracic/lumbar AIS is shown in Table 5. Considering thoracic scoliosis correction and fusion over 10 levels, use of the single rod technique in our series would reduce implant cost by 65% compared to a double rod construct with bilateral segmental screws and by 51% compared to a construct using the authors’ reported lesser screw density technique[10]. If this was extended to correction and fusion of 15 levels (such as in double major curves) use of the single rod technique would result in 64% reduction in cost compared to a double rod construct with bilateral segmental screws and 49% compared to a construct using the authors’ reduced screw density.
| No. of levels included | Type of construct | Instrumentation | Comparative cost |
| 10 (thoracic fusion) | Double rod construct with bilateral segmental pedicle screws (implant density: 2) | 20 pedicle screws 20 sleeves and nuts 2 rods | 100% |
| Double rod construct using the authors’ preferred technique (implant density: 1.38)[10] | 14 pedicle screws 14 sleeves and nuts 2 rods | 29% reduction compared to bilateral segmental pedicle screw construct | |
| Single rod hybrid construct | 3 pedicle screws 3 pedicle screw hooks 1 transverse process hook 7 sleeves and nuts 1 rod | 65% reduction compared to bilateral segmental pedicle screw construct; 51% reduction compared to authors’ preferred technique | |
| 15 (Thoracic and Lumbar fusion) | Double rod construct with bilateral segmental pedicle screws (implant density: 2) | 30 pedicle screws 30 sleeves and nuts 2 rods | 100% |
| Double rod construct using authors preferred technique (implant density: 1.38)[10] | 21 pedicle screws 21 sleeves and nuts 2 rods | 29% reduction compared with bilateral segmental pedicle screw construct | |
| Single rod construct | 6 pedicle screws 5 pedicle screw hooks 1 transverse process hook 12 sleeves and nuts 1 rod | 64% reduction compared to bilateral segmental pedicle screw construct; 49% reduction compared to authors’ preferred technique |
The use of double rod constructs in the treatment of scoliosis is associated with satisfactory clinical and radiographic outcomes, and this has always been the standard of care in the vast majority of our patients. Bilateral pedicle screw instrumentation has become the standard of care to provide powerful correction and stable fixation until a solid fusion is achieved. However, the use of bilateral segmental pedicle screws leads to greater neurological risks, longer operative times and blood loss, potential for instrumentation prominence, and an increase in the risk of deep infection due to high implant density. There is an ongoing interest in limiting the risks of instrumentation placement by reducing the number of implants used during correction[10,12].
There may be a number of patients where it is valid to use a single rod construct in order to minimize surgical morbidity. Cawley et al[6] reported 41 patients with DMD, where early correction using limited fixation with one rod proximal to the pelvis allowed adequate sitting posture with low peri-operative morbidity. Unilateral rod fixation is also commonly used in growing rod constructs with good reported outcomes[13]. Reduced operative morbidity is especially attractive for pediatric patients who require repetitive surgeries. Whilst it is apparent that the potential advantages of a limited surgical technique may be useful in select patient groups, clear indications have not been established.
This study presents our experience of the single rod technique and describes the limited indications for its use in our practice. The decision to use such surgical approach is tailored to the individual patient. This includes high risk of neurological or cardiac complications; risk of increased intra-operative blood loss due to severe underlying co-morbidities; low BMI leading to problems related to instrumentation prominence; early onset deformity and repetitive surgery with partial fusion due to the use of growing rods and often initial apical convex growth arrest; and pre-existing severe eczema. One or more of these indications has been present in our patients, and we have used the single rod technique in three groups: (1) complex deformity - high risk of cardiac/pulmonary/neurological complications and intra-operative blood loss as well as low BMI; (2) Conversion of growing rod to definitive fusion - a balanced correction is required; the patients often have low BMI and significant medical co-morbidities; and (3) Adolescent idiopathic scoliosis - in patients with moderate curves, low BMI, and severe eczema that increase the risk of either wound or systemic infection. The first two groups represent a mixture of underlying diagnoses and include syndromic, early onset idiopathic, neuromuscular, and congenital scoliosis associated with intraspinal anomalies[14,15].
The outcomes from the use of the single rod technique in our AIS patients with moderate primarily thoracic curves were satisfactory, and we did not record any complications. In AIS patients with no severe eczema, we select a dual pedicle screw/rod technique that is more effective to correct the deformity and has produced optimum outcomes[10,11]. In severe AIS we also find that the dual rod segmental pedicle screw techniques have greater ability to correct the deformity without the need for anterior release to increase curve flexibility when compared to the single rod hybrid technique[10,11]. Our results of the single rod technique are in contrast to those reported by Wattenbarger et al[4] who identified a higher rate of rod breakage with single (21%) than double rods (4%) in AIS. Rod failure occurred in three of our complex patients with severe syndromic or congenital kyphoscoliosis (3%). Our revision rate was 2% (including a distal junctional kyphosis in a Marfan’s syndrome patient). Cawley et al[6] recorded 7.3% rod breakage when they used the single rod technique in DMD patients. The use of post-operative immobilization (spinal jacket) may have contributed to our reduced instrumentation failure rates. Post-operative orthotic support can protect the rod construct and provide additional stability until fusion is achieved.
Due to the multitude of underlying diagnoses in groups A and B, a direct comparison to previous studies cannot be made. The number of patients where we felt a single rod construct would be preferable to dual instrumentation is small and represents less than 10% of the senior author’s practice in the same chronological period. However, our results demonstrate that the single rod correction technique within the above limited indications can achieve satisfactory deformity correction with low complication rates in patients with severe underlying co-morbidities. In our experience, this technique has reduced surgical time and intra-operative blood loss resulting in lower peri-operative morbidity in medically compromised patients with considerably less implant related complications than previously reported[4]. Instrumentation cost has also been significantly reduced when compared to a double pedicle screw/rod technique.
Scoliosis surgery is a major spinal procedure that is associated with significant risks of neurological and medical complications, producing permanent patient disability and increasing surgical morbidity. Surgical techniques have been developed in an attempt to standardize patient treatment and reduce the rate of operative complications. In recent decades, dual-rod instrumentation has become the standard of care for scoliosis correction. The introduction of segmental pedicle screws has allowed better coronal and axial deformity correction but has increased surgical risks. Single-rod correction techniques have been used in patients with adolescent idiopathic scoliosis (AIS) and Duchenne muscular dystrophy with controversial results in two previous series.
Single-rod correction techniques may offer advantages over dual-rod pedicle screw constructs, including reduced operative time and blood loss, lower risk of infection and instrumentation profile, easier surgical planning and operative technique, as well as reduced implant cost. In patients with major co-morbidities, such techniques may improve surgical safety and reduce associated morbidity and mortality of the procedure.
In this study, we reviewed demographic, radiographic, surgical, as well as quality of life data of 99 children and adolescents with scoliosis who underwent surgical correction using a single rod hybrid technique under the senior author. We report on the effectiveness of this technique in correcting the spinal deformity and focus on the rate of complications. We also analyzed the instrumentation costs in AIS and compared the single rod construct to previous series of patients treated in our practice with segmental pedicle screw dual instrumentation.
We prospectively collected data on 99 pediatric patients including review of patient records and spinal radiographs as well as assessment of quality of life questionnaires (SRS-22) in AIS patients both before and after surgery. We applied statistical analysis of our results where appropriate and compared the outcomes of the single rod technique to those that we had previously reported in the treatment of AIS using dual segmental pedicle screw constructs.
We included three groups of patients: Group A had 62 patients with complex deformities and low BMI associated with medical co-morbidities increasing the risk of cardiac, respiratory, and neurological complications, and intra-operative blood loss; group B had 21 patients previously treated with growing rod lengthenings who underwent definitive spinal fusion; group C had 16 patients with moderate AIS, low BMI, and severe eczema at risk of wound or systemic infection. Mean age at surgery was 12.8 years (SD 3.5 years). Mean scoliosis correction for the 99 patients was 62% (SD 15%) from 73° (SD 22°) to 28° (SD 15°). Mean surgical time was 153 min (SD 34 min), and blood loss was 530 mL (SD 327 mL); 20% blood volume (SD 13%). Mean clinical and radiological follow-up was 3.2 years (range: 2-12) post-operatively. Complications included rod failure, which occurred in three of our complex patients (group A) with severe syndromic or congenital kyphoscoliosis (3%). Only one of these three patients required revision surgery to address a non-union. Our revision rate was 2% (including a distal junctional kyphosis in a Marfan’s syndrome patient that required distal extension of the fusion).
The single-rod technique has achieved and maintained at follow-up good deformity correction associated with low surgical time, blood loss, and surgical morbidity. The use of lesser implants may reduce the instrumentation related risks, such as pedicle screw malposition, producing neurological, vascular, or visceral injury. The risk of wound infection may also be reduced as the volume of implants used in single rod instrumentation is much less than that in a dual rod/segmental pedicle screw construct. In our practice, this technique has a role primarily in pediatric patients with severe underlying co-morbidities and high surgical risks. The single rod technique has also reduced significantly the instrumentation cost compared to dual rod pedicle screw techniques, which is an important consideration at a time when health economics play an essential role in provision of patient care. Our complication rate is markedly lower than that reported in the two previous series of AIS or Duchenne muscular dystrophy patients with a low rate of re-operation (2%). We recorded high patient satisfaction among AIS patients and good functional outcomes that are comparable to our previous series of patients treated with dual rod/segmental pedicle screw instrumentation.
Despite the fact that the longest postoperative follow-up in our study was 12 years (mean follow-up: 3.2 years), we are monitoring our patients beyond skeletal maturity and well into adult life in order to confirm that no long-term complications occur. We believe that in light of this study the single rod technique is a reasonable alternative to dual rod techniques, especially in the treatment of complex patients with associated high morbidity. Further studies comparing outcomes of different techniques would be useful to determine the best option in different clinical scenarios and types of deformity.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Cheuk DKL, Lykissas MG S- Editor: Ji FF L- Editor: Filipodia E- Editor: Song H
| 1. | Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29:343-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 287] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 2. | Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke Type I adolescent idiopathic scoliosis curves. Spine (Phila Pa 1976). 2005;30:1859-1866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 109] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 3. | Suk SI, Kim JH, Kim SS, Lim DJ. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur Spine J. 2012;21:13-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 88] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 4. | Wattenbarger JM, Richards BS, Herring JA. A comparison of single-rod instrumentation with double-rod instrumentation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2000;25:1680-1688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Wattenbarger JM, Herring JA, Bronson D, Ashman RB. Mechanical testing of a single rod versus a double rod in a long-segment animal model. J Spinal Disord. 2001;14:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Cawley DT, Carmody O, Dodds MK, McCormack D. Early limited instrumentation of scoliosis in Duchenne muscular dystrophy: is a single-rod construct sufficient? Spine J. 2015;15:2166-2171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Cobb JR. Outline for the study of scoliosis. The American Academy of Orthopedic Surgeons Instructional Course Lectures. Instr Course Lect. 1948;5:261-275. |
| 8. | Risser JC. The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop. 1958;11:111-119. [PubMed] |
| 9. | Lenke LG, Betz RR, Haher TR, Lapp MA, Merola AA, Harms J, Shufflebarger HL. Multisurgeon assessment of surgical decision-making in adolescent idiopathic scoliosis: curve classification, operative approach, and fusion levels. Spine (Phila Pa 1976). 2001;26:2347-2353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 139] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 10. | Tsirikos AI, Subramanian AS. Posterior spinal arthrodesis for adolescent idiopathic scoliosis using pedicle screw instrumentation: does a bilateral or unilateral screw technique affect surgical outcome? J Bone Joint Surg Br. 2012;94:1670-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Tsirikos AI, Mataliotakis G, Bounakis N. Posterior spinal fusion for adolescent idiopathic scoliosis using a convex pedicle screw technique: a novel concept of deformity correction. Bone Joint J. 2017;99-B:1080-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Quan GM, Gibson MJ. Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation: does higher implant density improve correction? Spine (Phila Pa 1976). 2010;35:562-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Farooq N, Garrido E, Altaf F, Dartnell J, Shah SA, Tucker SK, Noordeen H. Minimizing complications with single submuscular growing rods: a review of technique and results on 88 patients with minimum two-year follow-up. Spine (Phila Pa 1976). 2010;35:2252-2258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Bounakis N, Karampalis C, Sharp H, Tsirikos AI. Surgical treatment of scoliosis in Rubinstein-Taybi syndrome type 2: a case report. J Med Case Rep. 2015;9:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Mataliotakis GI, Tsirikos AI, Pearson K, Urquhart DS, Smith C, Fall A. Scoliosis Surgery in Cystic Fibrosis: Surgical Considerations and the Multidisciplinary Approach of a Rare Case. Case Rep Orthop. 2016;2016:7186258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |