Published online Sep 18, 2018. doi: 10.5312/wjo.v9.i9.120
Peer-review started: March 29, 2018
First decision: April 29, 2018
Revised: June 20, 2018
Accepted: June 26, 2018
Article in press: June 27, 2018
Published online: September 18, 2018
Processing time: 171 Days and 7.5 Hours
To evaluate the treatment of osteonecrosis of the femoral head (ONFH) with the use of vascular endothelial growth factor (VEGF).
In 30 mature beagles (6 groups of 5 beagles) ONFH was induced cryosurgically and one of the following solutions was administered locally in the femoral head (FH) in each group: Single injection of 500 μg VEGF (t-VEGFμ group); single injection of 500 ng VEGF (t-VEGFn group); continuous delivery of 500 μg VEGF through osmotic micropump (t-VEGFpump-μ group); continuous delivery of 500 ng VEGF through osmotic micropump (t-VEGFpump-n group); single injection of 0.9% sodium chloride (t-NS group), while one group that served as control group did not receive any local solution (No-t group). FHs were retrieved 12 wk postoperatively, underwent decalcification and hematoxylin/eosin and toluidine blue staining. In two canines per group, one half of FH was processed without decalcification and stained with modified Masson Trichrome. Histological sections were observed by light microscopy and measured with a semi-automatized bone histomorphometry system and Bone Volume/Total Volume (BV/TV), Marrow Volume/Total Volume (MaV/TV), and Trabecular Thickness (TbTh) were assessed. Standard and robust tests (Welch, Brown Forsythe) of analysis of variance along with multiple comparisons, were carried out among the categories.
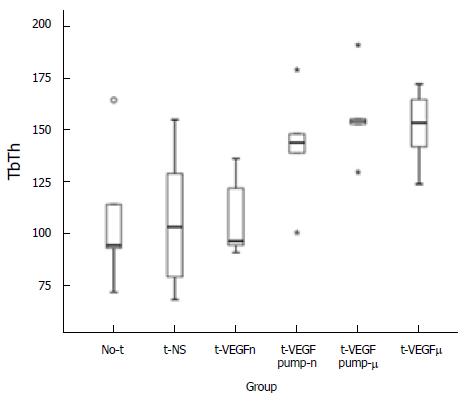
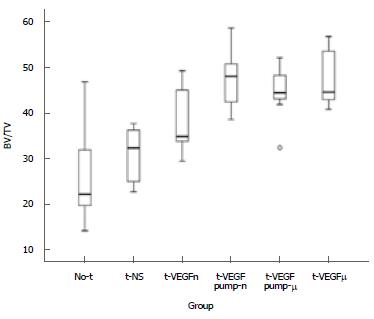
The untreated (No-t) group had signs of osteonecrosis, whereas the VEGF groups revealed reversal of the osteonecrosis. Statistical analysis of the decalcified specimens revealed a significantly better BV/TV ratio and a higher TbTh between the VEGF treatment groups (except the t-VEGFn group) and the No-t group or the control t-NS group. Single dose 500 μgVEGF group had significantly better BV/TV ratio and higher TbTh when compared to the No-t group (50.45 ± 6.18 vs 29.50 ± 12.27, P = 0.002 and 151.44 ± 19.07 vs 107.77 ± 35.15, P = 0.161 respectively) and the control t-NS group (50.45 ± 6.18 vs 30.9 ± 6.67, P = 0.004 and 151.44 ± 19.07 vs 107.14 ± 35.71, P = 0.151 respectively). Similar differences were found for the prolonged VEGF delivery/pump groups of 500 μg and 500 ng. Analysis of the totality of specimens (decalcified/non-decalcified) enhanced the aforementioned differences and additionally revealed significant differences in the comparison of the TbTh.
In an experimental model of ONFH in canines it was found that local treatment with VEGF leads to bone tissue remodeling and new bone formation.
Core tip: Osteonecrosis of the femoral head (ONFH) is a painful disorder which usually results in hip joint destruction. Although the pathogenic process is poorly understood, ON is the final condition that completes an already precarious microcirculation of the FH by traumatic and non-traumatic causes. Since vascular endothelial growth factor (VEGF) regulates numerous cellular events associated with angiogenesis and osteogenesis, we evaluated, in an experimental model of ONFH in canines if the local treatment with VEGF leads to bone tissue remodeling and new bone formation at the necrotic site, and subsequently to reversal of ON.
- Citation: Dailiana ZH, Stefanou N, Khaldi L, Dimakopoulos G, Bowers JR, Fink C, Urbaniak JR. Vascular endothelial growth factor for the treatment of femoral head osteonecrosis: An experimental study in canines. World J Orthop 2018; 9(9): 120-129
- URL: https://www.wjgnet.com/2218-5836/full/v9/i9/120.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i9.120
Osteonecrosis (ON), also known as avascular necrosis (AVN), is defined as a pathologic process that results from a crucial disruption of blood supply to the bone and elevated intraosseous pressure. Ischemic injury subsequently leads to the degradation of the organic elements of the bone and the marrow and usually results in a collapse of subchondral bone in the femoral head (FH)[1-3]. Also, numerous studies have emphasized the association of multiple risk factors, including alcohol consumption, glucocorticoids, trauma, autoimmune diseases, thrombophilia, genetic and metabolic components with secondary ON[4,5]. A process of repair is initiated at the necrotic - adjacent intact trabeculae interface by fibrovascular tissue invasion and osteoclasts activation followed by a temporary osteoblastic activity, but unless the lesion is small, this repair procedure is usually ineffective. The structural collapse of the osteonecrotic segment indicates the progressive course of the disease, leads to osteoarthritis of the hip joint in young adults and up to now total hip replacement is predestinate in the long term[6].
Early diagnosis and management aims to suspend the process of joint destruction through enhancement of bone repair and bone renewal. In the early stages of ON there are surgical alternatives to restrain the progressive destruction of the subchondral bone such as core decompression, osteotomy, non-vascularized or vascularized bone grafting, which might be enhanced with the use of growth and differentiation factors[6-12]. Recently, scientists introduced the use of cell-based strategies to enhance osseous regeneration by the application of multipotent mesenchymal stem cells (MSCs), endothelial progenitor cells (EPCs), and osteochondral auto- and allografts in a variety of in vivo and ex vivo processing[10-11,13]. Furthermore, promising osteogenic growth factors, investigated for their bone healing potential, such as bone morphogenetic proteins (BMPs), transforming growth factor-β1 (TGF-β1), hepatocyte growth factor (HGF) and vascular endothelial growth factor (VEGF)[10,14,15], received attention the past decades.
As bone is a highly vascularized tissue, angiogenic cytokines are essential components during the healing process of the necrotic FH. Among them, VEGF has shown its vital role, in a paracrine and autocrine manner, as a specific endothelial cell mitogen and a promoter of angiogenesis[16,17]. It is the major endothelial cell survival factor that is required for effective coupling of angiogenesis and osteogenesis in the bone microenvironment. Reconstructing local microcirculation and increasing blood vessel density are essential parameters for effective bone regeneration, the major objective of bone tissue engineering[18,19]. Furthermore, it has been suggested that the inhibition of the VEGF downregulates the extracellular matrix remodeling and bone formation in animal models[20]. Thus, it is not surprising that a recent meta-analysis clarified an association between VEGF polymorphisms and the risk of the FH necrosis[21].
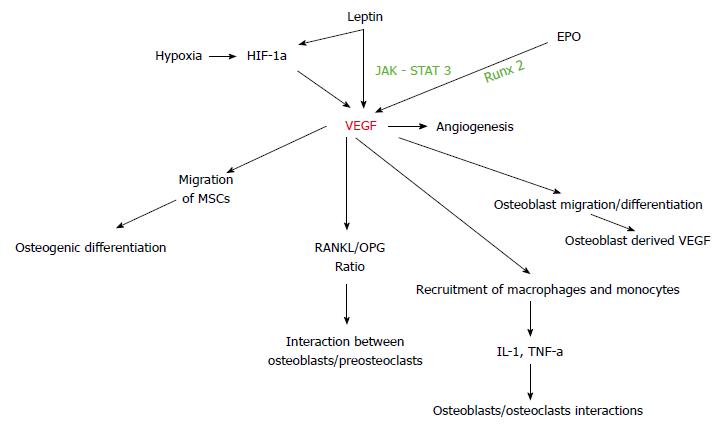
It seems that several molecular pathways regulate the balance between osteoclasts and osteoblasts and determine the rate of bone remodeling. Thus, considerable effort, using in vitro and in vivo models including animal models, has been directed towards understanding the effect of growth factors and transcription factors on bone resorption and formation. Through the last decades it was well established that VEGF is a crucial part of the wide network of the molecules regulating osteoinduction on the femoral head like BMPs, leptin, hypoxia - inducible factor (HIF) and their target genes[22-25]. Under these considerations, an experimental model of cryosurgically-induced ONFH in canines was used to assess the power of our hypothesis that VEGF could be a crucial therapeutic factor for bone tissue remodeling and reversal of osseous degradation during the treatment of ON.
After approval from the Institutional Animal Care and Use Committee, cryosurgically-induced ON of the right FH was established in 30 mature beagles (6 groups with 5 specimens)[26]. The canines were sedated with Acepromazine and anesthetized with iv injection of Thiopental. Anesthesia was maintained with endotracheal intubation and inhalation of isoflurane, while a Fentanyl patch provided analgesia during the procedure and postoperatively. Under absolute aseptic conditions a cryoprobe (CMS Accuprobe 620, Cryomedical Sciences Inc, Rockville, MD) was inserted in the FH through a drill hole extending from the lateral subtrochanteric region to the subchondral bone of the FH. A freezing lesion was created by a freeze (-180 oC) - thaw cycle[26]. Subsequently, the necrotic area of the FH was either left untreated or treated with local delivery of VEGF (rhVEGF, Genentech Inc, South San Francisco, CA) or 0.9% sodium chloride (normal saline, NS). NS was injected in a single dose of 1 mL, while VEGF was either injected in a single dose of 500 μg (in 1 mL) or 500 ng (in 1 mL) or administered continuously in the necrotic area with the use of an osmotic micropump (ALZET osmotic pumps, ALZA Corporation, Palo Alto, CA), in a dose of 500 μg or 500 ng, delivering 5 μL/h over a period of 14 d.
The beagles were assigned to 6 groups of 5 canines each: Untreated ONFH (No-t group), ONFH treated with NS (t-NS group), ONFH treated with a single injection of 500 μg VEGF (t-VEGFμ group), ONFH treated with a single injection of 500 ng VEGF (t-VEGFn group), ONFH treated with 500 μg VEGF delivered through a pump (t-VEGFpump-μ group), ONFH treated with 500 ng VEGF delivered through a pump (t-VEGFpump-n group). The procedure lasted less than one hour and was tolerated very well by the animals which were weight - bearing the first postoperative hours.
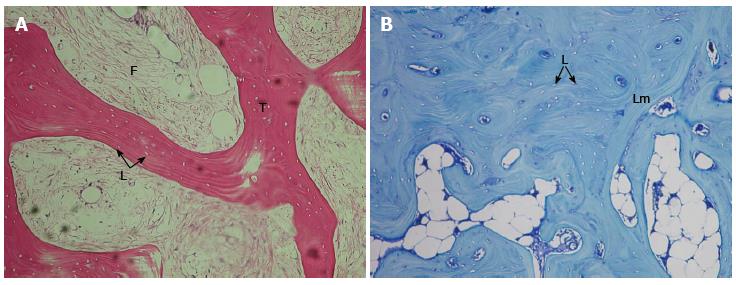
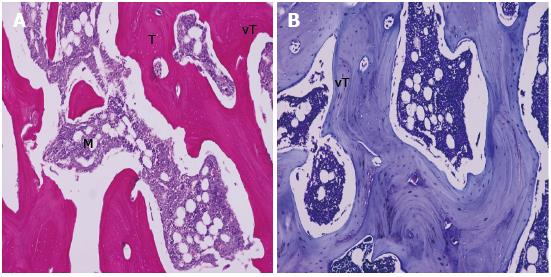
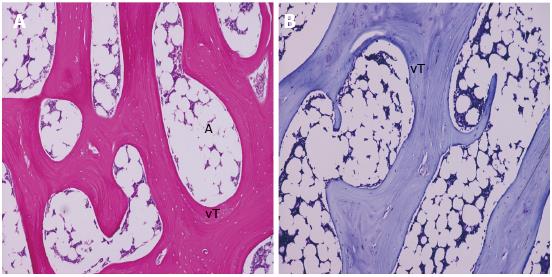
The canines were euthanized at 12 wk. All FHs were retrieved and fixed in 10% neutral buffer formalin for 24 h, cut in half in the frontal level using low-speed diamond sawing machine (IsoMet-Buehler). One half underwent decalcification with neutral EDTA solution pH 7, dehydrated and embedded in paraffin. Sections (5 μm thick) were stained with hematoxylin and eosin (H and E) (Figures 1A, 2A and 3A), as well as toluidine blue (TB) (Figures 1B, 2B and 3B). In two canines per group (with the exception of the t-NS group) the other half of the retrieved FH was processed without decalcification, dehydrated, embedded in methylmethacrylate, sectioned with Polycut Model microtome (Leica, Heidelberg, Germany), and stained with modified Masson Trichrome (MT). Histological sections were observed by light microscopy and measured with a semi-automatized bone histomorphometry system using OsteoMeasure software (Interactive measure system for bone histomorphometry, Osteometrics, Atlanta, GA) and the following values were assessed: Bone Volume/Total Volume (BV/TV), Marrow Volume/Total Volume (MaV/TV) and Trabecular Thickness (TbTh), at the subchondral area (above the tip of the tunnel created for the insertion of the cryoprobe)[27]. The 4 groups treated with VEGF (t-VEGFμ, t-VEGFn, t-VEGFpump-μ, t-VEGFpump-n) were compared with each other, with the group treated with normal saline (t-NS) and with the untreated group (No-t).
Means and standard deviations were used to describe the values of BV/TV, MaV/TV and TbTh across the categories studied. Standard, as well as robust tests (Welch, Brown Forsythe), of analysis of variance along with multiple comparisons under the Tukey’s HSD criterion, were carried out to detect statistically significant differences among the categories. Statistical significance was set at 0.05 and the SPSS v21.0 was used for the analysis of the data.
The untreated group had signs of osteonecrosis (Figure 1A and B), whereas the treatment groups revealed reversal of the osteonecrosis (Figures 2A and B, 3A and B) except the group treated with NS, that served as control[26]. Statistical analysis was performed in the decalcified specimens (5 samples per group). An additional analysis was performed in the totality of specimens (5 decalcified and 2 non-decalcified; 7 samples per group except of the t-NS group where only 5 decalcified were included). Analysis of the decalcified specimens revealed a significant difference in the BV/TV and MV/TV ratio (BV/TV and MV/TV ratios are complementary) between the VEGF treatment groups (apart of the t-VEGFn group) and the untreated (No-t) group or the t-NS control group (Table 1). A non-significant difference of the trabecular thickness (TbTh) was observed between the VEGF (apart of the t-VEGFn) treatment groups and the untreated (No-t) group or the t-NS control group (Table 1).
| N | mean | SD | P-value vs No-t | P-value vs t-NS | P-value vs t-VEGF-n | |
| BV/TV | ||||||
| No-t | 5 | 29497 | 12265 | - | NS | NS |
| t-NS | 5 | 30902 | 6672 | NS | - | NS |
| t-VEGFn | 5 | 35220 | 5256 | NS | NS | - |
| t-VEGFpump-n | 5 | 48250 | 6869 | 0.006 | 0.013 | NS |
| t-VEGFpump-μ | 5 | 47077 | 4677 | 0.011 | 0.023 | NS |
| t-VEGFμ | 5 | 50450 | 6181 | 0.002 | 0.004 | 0.036 |
| Total | 30 | 40233 | 11039 | |||
| TbTh | ||||||
| No-t | 5 | 107776 | 35146 | - | NS | NS |
| t-NS | 5 | 107149 | 35711 | NS | - | NS |
| t-VEGFn | 5 | 108195 | 19986 | NS | NS | - |
| t-VEGFpump-n | 5 | 142307 | 28107 | 0.380 | 0.361 | NS |
| t-VEGFpump-μ | 5 | 156875 | 21965 | 0.088 | 0.082 | NS |
| t-VEGFμ | 5 | 151445 | 19065 | 0.161 | 0.151 | 0.168 |
| Total | 30 | 128958 | 33361 | |||
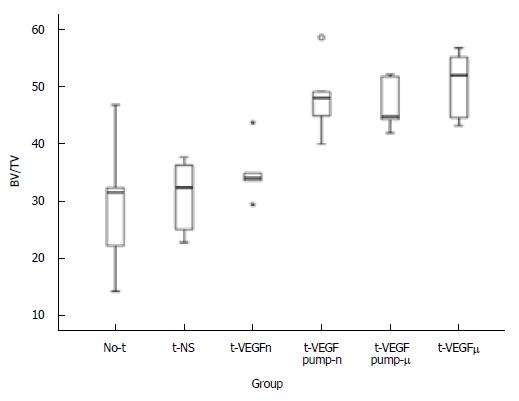
Group t-VEGFμ had significantly better BV/TV ratio and higher TbTh when compared to the untreated group (No-t) (P = 0.002 and P = 0.161 respectively) and the control t-NS group (P = 0.004 and P = 0.151 respectively) (Table 1, Figure 2A and B). Analogous differences were found for the groups t-VEGFpump-μ (P = 0.011 and P = 0.088 respectively for comparison with the No-t group; P = 0.023 and P = 0.082 respectively for comparison with the t-NS group) (Figure 3A and B) and t-VEGFpump-n (P = 0.006 and P = 0.380 respectively for comparison with the No-t group; P = 0.013 and P = 0.361 respectively for comparison with the t-NS group). The only group with different behaviour was the t-VEGFn group with similar responses to the No-t group for the BV/TV ratio and the TbTh (P = 0.823 and P = 1 respectively) and the control t-NS group (P = 0.937 and P = 1 respectively) (Table 1, Figures 4 and 5).
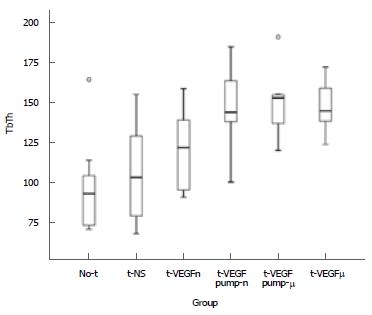
When the different VEGF treatment groups were compared to each other, there was a hierarchic response concerning the BV/TV ratio as following: t-VEGFμ > t-VEGFpump-n > t-VEGFpump-m > t-VEGFn, with a significant difference between the t-VEGFμ and t-VEGFn groups (P = 0.036) (Table 1). Analysis of the totality of specimens enhanced the aforementioned differences and also revealed significant differences also in the comparison of the TbTh (Table 2).
| N | mean | SD | P-value vs No-t | P-value vs t-NS | P-value vs t-VEGF-n | |
| BV/TV | ||||||
| No-t | 7 | 26739 | 11135 | - | NS | NS |
| t-NS | 5 | 30902 | 6672 | NS | - | NS |
| t-VEGFn | 7 | 38853 | 7591 | NS | NS | - |
| t-VEGFpump-n | 7 | 47485 | 7009 | < 0.001 | 0.011 | NS |
| t-VEGFpump-μ | 7 | 44634 | 6638 | 0.002 | 0.053 | NS |
| t-VEGFμ | 7 | 48005 | 6573 | < 0.001 | 0.008 | 0.27 |
| Total | 40 | 39863 | 11013 | |||
| TbTh | ||||||
| No-t | 7 | 97891 | 33316 | - | NS | NS |
| t-NS | 5 | 107149 | 35711 | NS | - | NS |
| t-VEGFn | 7 | 120315 | 26799 | NS | NS | - |
| t-VEGFpump-n | 7 | 147738 | 28295 | 0.020 | 0.145 | NS |
| t-VEGFpump-μ | 7 | 149884 | 22642 | 0.014 | 0.111 | NS |
| t-VEGFμ | 7 | 148194 | 16770 | 0.018 | 0.137 | 0.42 |
| Total | 40 | 129597 | 33360 | |||
Group t-VEGFμ had significantly higher BV/TV ratio and TbTh when compared to the untreated group (No-t) (P = 0.000 and P = 0.018 respectively). When compared to the control t-NS group the differences were higher or significantly higher (P = 0.008 and P = 0.137 respectively for the BV/TV and TbTh) (Figure 2A and B). Analogous differences were found for the groups t-VEGFpump-μ (P = 0.02 and P = 0.014 respectively for comparison with the No-t group; P = 0.053 and P = 0.111 respectively for comparison with the t-NS group) (Figure 3A and B) and t-VEGFpump-n (P = 0.000 and P = 0.020 respectively for comparison with the No-t group; P = 0.011 and P = 0.145 respectively for comparison with the t-NS group). The t-VEGFn group had with similar responses to the No-t group for the BV/TV ratio and the TbTh (P = 0.067 and P = 0.649 respectively) and the control t-NS group (P = 0.520 and P = 0.962 respectively) (Table 2, Figures 6 and 7). The hierarchic responses were the same with the decalcified analysis (Table 2).
Osteonecrosis of the FH is a multifactorial disease affecting mostly young individuals (average age 35-50), leading to a subchondral bone infarct and to FH collapse and finally to the destruction of the hip joint. Among all controversial pathogenic mechanisms of ON, ischemic injury, which results from interruption of the blood supply and lack of oxygen, appears to be the most convincing. Decreased blood flow is followed by death of bone and marrow elements. A process of repair is then initiated by fibrovascular tissue invasion and osteoclasts activation, followed by a temporary osteoblastic activity, but unless the lesion is small, this repair process is usually ineffective leading to eventual collapse of the architectural bony structure of the FH and loss of hip joint function[1,2,4].
Core decompression is considered the gold standard technique for the treatment of pre-collapse, early stage ON (ARCO I-II) of the FH and reveals superior clinical outcome in comparison with non-operative treatment alternatives[6,10]. Other surgical options may include rotational osteotomy, non-vascularized and vascularized bone grafting, which might be enhanced with the use of growth and differentiation factors and anterograde osteochondral reconstruction in advanced, post-collapse, stages of ON (ARCO III-IV)[6-11,28]. As the treatment of osteochondral defects in advanced stages of ON remains an unresolved issue in orthopedic surgery most young patients usually resulting in the terminal option of the total hip arthroplasty[6,12].
In order to overcome the disadvantages of traditional therapies, scientists promote bone tissue engineering techniques for achieving effective bone regeneration and successful osteoinduction. It has been well established that the growth, development and maintenance of bone are highly regulated processes, which at the cellular level involve the coordinated regulation of osteoblasts and osteoclasts. Several molecular pathways regulate the balance between osteoclasts and osteoblasts and determine the role of bone remodeling. Osteoclastic activity appears to be modulated by cytokines released by osteoblasts. Numerous osteogenic growth factors such as BMPs, TGF-β1, erythropoietin (EPO), platelet - derived growth factor (PDGF) and granulocyte colony-stimulating factor (G-CSF) have been proposed as target molecules for enhancing the osteoinduction[10,11,29,30].
Blood supply is undoubtedly the absolute goal for any tissue engineering manipulation of the musculoskeletal system and osteonecrotic bone[22,31]. It is well understood that the reconstruction of the local microcirculation is prerequisite for effective bone regeneration[18]. Since angiogenesis and osteogenesis are highly coupled and VEGF is one of the most important growth factors for the regulation of vascular development we can easily recognize it as a pivotal regulator of bone repair[32]. VEGF as a proinflammatory, angiogenic and osteogenic cytokine regulates osteoblastic activity by stimulating crosstalk between endothelial, osteoblastic and hematopoietic cells in a paracrine manner and it directly affects osteoblast functions via autocrine mechanisms[18,33]. Moreover, the multipotent role of the VEGF in the bone environment includes the regulation of maturation and differentiation of osteoclasts, the recruitment of MSCs and osteoprogenitor cells, the promotion of the osteogenic differentiation of MSCs and finally cartilage formation and resorption[22,34]. All these studies demonstrate that the bone regeneration process in the osteonecrotic microenvironment could be affected by manipulation of VEGF levels (Figure 8).
In the present study the influence of the commonly accepted as an angiogenic factor-VEGF on osteogenesis was investigated in an experimental model of ONFH, in mature beagles. Our results indicate that the experimental model of osteonecrosis is reliable and leads to uniform and reproducible osteonecrosis of the FH in the canines[26]. The surgical technique is relatively easy and minimally invasive, leading to decreased duration of the procedure and for that is well tolerated by the animals. Other benefits of this canine animal model are the low costs of rearing, the nature of the species as a representative of mammals, their body size that allows accurate surgical treatment and radiographic guidance or surveillance and the fact that can be achieved histological patterns which are similar to those of humans.
Moreover, we demonstrated that the use of the VEGF affects in a positive and dose dependent manner the necrotic bone and induces the process of osseous regeneration. Since now it is well established by numerous studies that there are strong indications of a cellular and molecular pattern of angiogenic-osteogenic coupling[18,19,22]. The restoration of bone vascularity is an absolute parameter in the process of osteoinduction, which is the target of any therapeutic agent against osteonecrosis in the FH. As VEGF acted in a dose dependent manner we conclude that the optimal amounts of VEGF are critical for the therapeutic outcome and probably depend on the size of the necrotic area. The levels of exogenous VEGF for its adequate activity are probably determined by both the type of cells in which it acts and the production of endogenous VEGF in them.
Taking into account that the analysis of the totality of specimens (decalcified and non-decalcified) magnified the differences between the subgroups we conclude that the healing interaction of the VEGF over the osseous tissue refers not only to the organic but to the inorganic fraction of the bone matrix too. This is important as the bone matrix serves as a reservoir for osteogenic growth factors which are pivotal collaborators of VEGF during bone repair[10,35]. It is essential for every therapeutic agent against ONFH to achieve a good quality of bone tissue during osseous regeneration.
Traditional administration of growth factors is limited by their relatively short half-lives and potential side effects[34]. VEGF has a short half-life of 6-8 h, which means that controlled and more sustained delivery could be required to ensure its efficient activity[19]. Under all these considerations we administered VEGF continuously in the necrotic FH with the use of an osmotic micropump over a period of 14 d but without transcendent outcome in comparison with single dose injection. It seems that a high single, initial dose is superior for the bone defect repair in this animal model and that may reveal that VEGF has a nodal role at early stages of the osteonecrotic bone healing procedure. The optimal delivery model of VEGF needs to be further studied. Utilizing a well-designed delivery system, like specific slow release scaffolds or gene delivery projects may better achieve bone regeneration and improve its therapeutic effect by stabilizing it against rapid degradation[22,35-37].
The results of previous studies supported that the vascular network induced by VEGF alone is immature[29,38]. There is obviously a wide network of molecules regulating bone regeneration such as BMPs, leptin, HIF, TGF, IGF and EPO. Even if VEGF is sufficient to improve revascularization, recently scientists introduced the use of a combination of growth factors and manipulated progenitor cells to enhance bone repair and bone renewal[15,22-24,35,39,40].
In summary, in an experimental model of ONFH in mature beagles it was found that the treatment with VEGF leads to bone tissue remodeling and new bone formation at the osteonecrotic site and subsequently to reversal of ON. This study however, has some limitations; it is an experimental study in canines, and in addition, the induction and treatment of ONFH (with local infusion of VEGF) are almost simultaneous procedures. Although local VEGF administration is known to promote angiogenesis and enhanced new bone formation in ONFH in our study, future studies should further investigate, in a variety of experimental conditions, the role of VEGF as a key molecule and essential player for therapeutic strategies targeting bone reconstruction, so that an even transition to clinical trials may be achieved.
Numerous studies have emphasized the association of multiple risk factors, including alcohol consumption, glucocorticoids, trauma, autoimmune diseases, thrombophilia, genetic and metabolic components with secondary osteonecrosis (ON). ON of the femoral head (FH) is a debilitating disease that usually leads to osteoarthritis of the hip joint in young adults and up to now total hip replacement is predestinate in the long term.
Early diagnosis and management aims to suspend the process of joint destruction through enhancement of bone repair and bone renewal. In the early stages of ONFH there are surgical alternatives to restrain the progressive destruction of the subchondral bone such as core decompression, osteotomy, non-vascularized or vascularized bone grafting. This study extended the prospect of use growth and angiogenic factors for the process of repair at the necrotic trabeculae of the FH.
The main aim of this research project was to evaluate the treatment of ONFH with the use of vascular endothelial growth factor (VEGF).
An experimental model of cryosurgically-induced ONFH in canines was used to assess the power of our hypothesis that VEGF could be a crucial therapeutic factor for bone tissue remodeling and reversal of osseous degradation during the treatment of ON. VEGF (2 different doses of 500 μg and 500 ng) was either injected in a single dose or administered continuously in the necrotic area with the use of an osmotic micropump, while in a control group 0.9% sodium chloride (NS) was injected in the necrotic area.
The untreated group had signs of ONFH, whereas the treatment groups with VEGF revealed reversal of the osteonecrosis, except the group treated with NS, that served as control. These findings demonstrate that the bone regeneration process in the osteonecrotic microenvironment could be affected by manipulation of VEGF levels.
We demonstrated that the use of the VEGF affects in a positive and dose dependent manner the necrotic bone and induces the process of osseous regeneration. Since now it is well established by numerous studies that there are strong indications of a cellular and molecular pattern of angiogenic-osteogenic coupling. The restoration of bone vascularity is an absolute parameter in the process of osteoinduction, which is the target of any therapeutic agent against ONFH.
In a reproducible experimental model of ONFH in mature beagles it was found that the treatment with VEGF leads to bone tissue remodeling and new bone formation at the osteonecrotic site and subsequently to reversal of ON. Besides that, the optimal delivery model of VEGF needs to be further studied. Utilizing a well-designed delivery system, like specific slow release scaffolds or gene delivery projects, may potentially lead to better bone regeneration and improve VEGFs therapeutic effect by stabilizing it against rapid degradation. Even if VEGF is sufficient to improve revascularization, recently scientists introduced the use of a combination of growth factors and manipulated progenitor cells to enhance bone repair and bone renewal. Although local VEGF administration is known to enhance new bone formation in ONFH in our study, future studies should further investigate, in a variety of experimental conditions, the role of VEGF as a key molecule and essential player for therapeutic strategies targeting bone reconstruction, so that an even transition to clinical trials may be achieved.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cheung WH, Cui Q, Tarnawski AS S- Editor: Ji FF L- Editor: A E- Editor: Song H
| 1. | Guerado E, Caso E. The physiopathology of avascular necrosis of the femoral head: an update. Injury. 2016;47 Suppl 6:S16-S26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 2. | Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77:459-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 842] [Cited by in RCA: 748] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 3. | Zalavras C, Dailiana Z, Elisaf M, Bairaktari E, Vlachogiannopoulos P, Katsaraki A, Malizos KN. Potential aetiological factors concerning the development of osteonecrosis of the femoral head. Eur J Clin Invest. 2000;30:215-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 67] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Seamon J, Keller T, Saleh J, Cui Q. The pathogenesis of nontraumatic osteonecrosis. Arthritis. 2012;2012:601763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 125] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 5. | Aldridge JM 3rd, Urbaniak JR. Avascular necrosis of the femoral head: etiology, pathophysiology, classification, and current treatment guidelines. Am J Orthop (Belle Mead NJ). 2004;33:327-332. [PubMed] |
| 6. | Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, Rajadhyaksha AD, Urbaniak JR. Osteonecrosis of the hip: management in the 21st century. Instr Course Lect. 2003;52:337-355. [PubMed] |
| 7. | Soucacos PN, Beris AE, Malizos K, Koropilias A, Zalavras H, Dailiana Z. Treatment of avascular necrosis of the femoral head with vascularized fibular transplant. Clin Orthop Relat Res. 2001;386:120-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 68] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Urbaniak JR, Coogan PG, Gunneson EB, Nunley JA. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting. A long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am. 1995;77:681-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 272] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 9. | Calori GM, Mazza E, Colombo M, Mazzola S, Mineo GV, Giannoudis PV. Treatment of AVN using the induction chamber technique and a biological-based approach: indications and clinical results. Injury. 2014;45:369-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Rackwitz L, Eden L, Reppenhagen S, Reichert JC, Jakob F, Walles H, Pullig O, Tuan RS, Rudert M, Nöth U. Stem cell- and growth factor-based regenerative therapies for avascular necrosis of the femoral head. Stem Cell Res Ther. 2012;3:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 69] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Papanagiotou M, Malizos KN, Vlychou M, Dailiana ZH. Autologous (non-vascularised) fibular grafting with recombinant bone morphogenetic protein-7 for the treatment of femoral head osteonecrosis: preliminary report. Bone Joint J. 2014;96-B:31-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | McGrory BJ, York SC, Iorio R, Macaulay W, Pelker RR, Parsley BS, Teeny SM. Current practices of AAHKS members in the treatment of adult osteonecrosis of the femoral head. J Bone Joint Surg Am. 2007;89:1194-1204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Müller I, Vaegler M, Holzwarth C, Tzaribatchev N, Pfister SM, Schütt B, Reize P, Greil J, Handgretinger R, Rudert M. Secretion of angiogenic proteins by human multipotent mesenchymal stromal cells and their clinical potential in the treatment of avascular osteonecrosis. Leukemia. 2008;22:2054-2061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Samara S, Dailiana Z, Varitimidis S, Chassanidis C, Koromila T, Malizos KN, Kollia P. Bone morphogenetic proteins (BMPs) expression in the femoral heads of patients with avascular necrosis. Mol Biol Rep. 2013;40:4465-4472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Yang C, Yang S, Du J, Li J, Xu W, Xiong Y. Vascular endothelial growth factor gene transfection to enhance the repair of avascular necrosis of the femoral head of rabbit. Chin Med J (Engl). 2003;116:1544-1548. [PubMed] |
| 16. | Hoeben A, Landuyt B, Highley MS, Wildiers H, Van Oosterom AT, De Bruijn EA. Vascular endothelial growth factor and angiogenesis. Pharmacol Rev. 2004;56:549-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1424] [Cited by in RCA: 1361] [Article Influence: 64.8] [Reference Citation Analysis (0)] |
| 17. | Ferrara N. Vascular endothelial growth factor: basic science and clinical progress. Endocr Rev. 2004;25:581-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2468] [Cited by in RCA: 2567] [Article Influence: 122.2] [Reference Citation Analysis (0)] |
| 18. | Saran U, Gemini Piperni S, Chatterjee S. Role of angiogenesis in bone repair. Arch Biochem Biophys. 2014;561:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 269] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 19. | Kaigler D, Wang Z, Horger K, Mooney DJ, Krebsbach PH. VEGF scaffolds enhance angiogenesis and bone regeneration in irradiated osseous defects. J Bone Miner Res. 2006;21:735-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 236] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 20. | Gerber HP, Vu TH, Ryan AM, Kowalski J, Werb Z, Ferrara N. VEGF couples hypertrophic cartilage remodeling, ossification and angiogenesis during endochondral bone formation. Nat Med. 1999;5:623-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1501] [Cited by in RCA: 1465] [Article Influence: 56.3] [Reference Citation Analysis (0)] |
| 21. | Hong GJ, Lin N, Chen LL, Chen XB, He W. Association between vascular endothelial growth factor gene polymorphisms and the risk of osteonecrosis of the femoral head: Systematic review. Biomed Rep. 2016;4:92-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Li B, Wang H, Qiu G, Su X, Wu Z. Synergistic Effects of Vascular Endothelial Growth Factor on Bone Morphogenetic Proteins Induced Bone Formation In Vivo: Influencing Factors and Future Research Directions. Biomed Res Int. 2016;2016:2869572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 23. | Zhou L, Jang KY, Moon YJ, Wagle S, Kim KM, Lee KB, Park BH, Kim JR. Leptin ameliorates ischemic necrosis of the femoral head in rats with obesity induced by a high-fat diet. Sci Rep. 2015;5:9397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Fan L, Li J, Yu Z, Dang X, Wang K. The hypoxia-inducible factor pathway, prolyl hydroxylase domain protein inhibitors, and their roles in bone repair and regeneration. Biomed Res Int. 2014;2014:239356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 25. | Fan L, Li J, Yu Z, Dang X, Wang K. Hypoxia-inducible factor prolyl hydroxylase inhibitor prevents steroid-associated osteonecrosis of the femoral head in rabbits by promoting angiogenesis and inhibiting apoptosis. PLoS One. 2014;9:e107774. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Dailiana Z, Fink Ch, Baust J, Seaher AV, Urbaniak JR. A new canine model of osteonecrosis with the use of cryosurgery. JACS. 2000;191:S91-S91. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Revell PA. Histomorphometry of bone. J Clin Pathol. 1983;36:1323-1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 64] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Huffman KM, Bowers JR, Dailiana Z, Huebner JL, Urbaniak JR, Kraus VB. Synovial fluid metabolites in osteonecrosis. Rheumatology (Oxford). 2007;46:523-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Lieberman JR, Daluiski A, Einhorn TA. The role of growth factors in the repair of bone. Biology and clinical applications. J Bone Joint Surg Am. 2002;84-A:1032-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 700] [Cited by in RCA: 635] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 30. | Xu T, Jin H, Lao Y, Wang P, Zhang S, Ruan H, Mao Q, Zhou L, Xiao L, Tong P. Administration of erythropoietin prevents bone loss in osteonecrosis of the femoral head in mice. Mol Med Rep. 2017;16:8755-8762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Jain RK, Au P, Tam J, Duda DG, Fukumura D. Engineering vascularized tissue. Nat Biotechnol. 2005;23:821-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 585] [Cited by in RCA: 581] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 32. | Coultas L, Chawengsaksophak K, Rossant J. Endothelial cells and VEGF in vascular development. Nature. 2005;438:937-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 726] [Cited by in RCA: 728] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 33. | Hu K, Olsen BR. Osteoblast-derived VEGF regulates osteoblast differentiation and bone formation during bone repair. J Clin Invest. 2016;126:509-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 468] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 34. | Aldridge SE, Lennard TW, Williams JR, Birch MA. Vascular endothelial growth factor receptors in osteoclast differentiation and function. Biochem Biophys Res Commun. 2005;335:793-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 78] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 35. | Almubarak S, Nethercott H, Freeberg M, Beaudon C, Jha A, Jackson W, Marcucio R, Miclau T, Healy K, Bahney C. Tissue engineering strategies for promoting vascularized bone regeneration. Bone. 2016;83:197-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 138] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 36. | Jung YJ, Kim KC, Heo JY, Jing K, Lee KE, Hwang JS, Lim K, Jo DY, Ahn JP, Kim JM. Induction of Angiogenesis by Matrigel Coating of VEGF-Loaded PEG/PCL-Based Hydrogel Scaffolds for hBMSC Transplantation. Mol Cells. 2015;38:663-668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 37. | Zhang C, Ma J, Li M, Li XH, Dang XQ, Wang KZ. Repair effect of coexpression of the hVEGF and hBMP genes via an adeno-associated virus vector in a rabbit model of early steroid-induced avascular necrosis of the femoral head. Transl Res. 2015;166:269-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 38. | Blau HM, Banfi A. The well-tempered vessel. Nat Med. 2001;7:532-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 87] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 39. | Kasten P, Beverungen M, Lorenz H, Wieland J, Fehr M, Geiger F. Comparison of platelet-rich plasma and VEGF-transfected mesenchymal stem cells on vascularization and bone formation in a critical-size bone defect. Cells Tissues Organs. 2012;196:523-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 40. | Hernigou P, Trousselier M, Roubineau F, Bouthors C, Chevallier N, Rouard H, Flouzat-Lachaniette CH. Stem Cell Therapy for the Treatment of Hip Osteonecrosis: A 30-Year Review of Progress. Clin Orthop Surg. 2016;8:1-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 101] [Article Influence: 11.2] [Reference Citation Analysis (0)] |