Peer-review started: January 11, 2018
First decision: February 9, 2018
Revised: March 16, 2018
Accepted: May 13, 2018
Article in press: May 13, 2018
Published online: June 18, 2018
Processing time: 155 Days and 1.1 Hours
To compare the measurements of knee rotation laxity by non-invasive skin pointer with a knee rotation jig in cadaveric knees against a skeletally mounted marker.
Six pairs of cadaveric legs were mounted on a knee rotation jig. One Kirscher wire was driven into the tibial tubercle as a bone marker and a skin pointer was attached. Rotational forces of 3, 6 and 9 nm applied at 0°, 30°, 45°, 60° and 90° of knee flexion were analysed using the Pearson correlation coefficient and paired t-test.
Total rotation recorded with the skin pointer significantly correlated with the bone marker at 3 nm at 0° (skin pointer 23.9 ± 26.0° vs bone marker 16.3 ± 17.3°, r = 0.92; P = 0.0), 30° (41.7 ± 15.5° vs 33.1 ± 14.7°, r = 0.63; P = 0.037), 45° (49.0 ± 17.0° vs 40.3 ± 11.2°, r = 0.81; P = 0.002), 60° (45.7 ± 17.5° vs 34.7 ± 9.5°, r = 0.86; P = 0.001) and 90° (29.2 ± 10.9° vs 21.2 ± 6.8°, r = 0.69; P = 0.019) of knee flexion and 6 nm at 0° (51.1 ± 37.7° vs 38.6 ± 30.1°, r = 0.90; P = 0.0), 30° (64.6 ± 21.6° vs 54.3 ± 15.1°, r = 0.73; P = 0.011), 45° (67.7 ± 20.6° vs 55.5 ± 9.5°, r = 0.65; P = 0.029), 60° (62.9 ± 22.4° vs 45.8 ± 13.1°, r = 0.65; P = 0.031) and 90° (43.6 ± 17.6° vs 31.0 ± 6.3°, r = 0.62; P = 0.043) of knee flexion and at 9 nm at 0° (69.7 ± 40.0° vs 55.6 ± 30.6°, r = 0.86; P = 0.001) and 60° (74.5 ± 27.6° vs 57.1 ± 11.5°, r = 0.77; P = 0.006). No statistically significant correlation with 9 nm at 30° (79.2 ± 25.1° vs 66.9 ± 15.4°, r = 0.59; P = 0.055), 45° (80.7 ± 24.7° vs 65.5 ± 11.2°, r = 0.51; P = 0.11) and 90° (54.7 ± 21.1° vs 39.4 ± 8.2°, r = 0.55; P = 0.079). We recognize that 9 nm of torque may be not tolerated in vivo due to pain. Knee rotation was at its maximum at 45° of knee flexion and increased with increasing torque.
The skin pointer and knee rotation jig can be a reliable and simple means of quantifying knee rotational laxity with future clinical application.
Core tip: We describe a cadaveric study utilising a knee rotation jig paired with a skin pointer for the measurement of knee rotation laxity which has the potential for clinical application.
- Citation: Puah KL, Yew AKS, Chou SM, Lie DTT. Comparison of a simplified skin pointer device compared with a skeletal marker for knee rotation laxity: A cadaveric study using a rotation-meter. World J Orthop 2018; 9(6): 85-91
- URL: https://www.wjgnet.com/2218-5836/full/v9/i6/85.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i6.85
With increased interest in rotational stability with anterior cruciate ligament reconstruction as seen with the anatomical anterior cruciate ligament (ACL) reconstruction and the double-bundle ACL reconstruction, the need for an objective measurement of knee rotation arises in order to compare subjective clinical scores with rotational stability[1]. Registry data currently do not show any significant difference in knee outcome scores between single-bundle and double-bundle ACL reconstructions though proponents of the double-bundle technique recommend it as it is considered to be able to restore both rotational stability and anterior-posterior stability[1,2]. Stress radiography with the use of Roentgen Stereophotogrammetric Analysis (RSA) has been described previously with accuracy as high as 10-250 μm and 0.03-0.6° for translations and rotations, respectively, though it is an invasive procedure[3,4]. With variability of the pivot shift test amongst even trained orthopaedic surgeons, it becomes imperative that a non-invasive objective instrument be available to assess a patient’s knee rotational stability[5]. There is a need for a portable, non-invasive yet simple to use device to measure knee rotation laxity in the clinic.
Almquist et al[6-8] has described a Rottometer which is a modified chair with the foot strapped to a rotating plate with measurements taken off a goniometer at the foot plate. However there was difference in the Rottometer readings compared to RSA at 90° flexion with 6 nm of torque and this has been attributed to be due to the measurements being taken at the foot which would thus include ankle rotation. To negate the effect of ankle rotation, we propose taking measurements off a fixed point more proximal and closer to the knee joint at the tibial tubercle with a non-invasive skin pointer while immobilizing the ankle in a foam boot. We designed a cadaveric study to assess the reliability of taking measurements off a non-invasive skin pointer placed over the tibial tubercle against that of a skeletally-mounted nail using a novel knee rotation jig modified from the Rottometer with a view to extending this to in-vivo testing.
To compare a non-invasive method of measuring knee rotation using a skin pointer against a nail fixed to the tibial tuberosity of a cadaveric knee specimen mounted on a knee rotation jig.
Six pairs of cadaveric legs were mounted individually on a prototype knee rotation jig modified from the Rottometer described by Almquist et al[7] with a locking mechanism to set knee flexion at several predetermined flexion angles (Figure 1). These cadaveric legs were stored frozen and were thawed prior to use in this study. The jig, which is collapsible, foldable and portable, was securely clamped to a table using vice clamps. Each specimen was anchored to the jig at the femur with bolts for stability and at the foot and ankle with an Aircast® Foam Walker (Aircast, Summit, NJ, United States) attached to a rotating baseplate (Figure 2). The Aircast® Foam Walker was mounted to the baseplate to negate the effect of ankle rotation by immobilizing the ankle and foot. The jig features two adjustable metal side plates with Velcro straps which will be used for in-vivo testing subsequently. One Kirscher wire was driven into the apex of the tibial tubercle as a bone marker for reference and a skin pointer was attached above the tibial tubercle using a Velcro strap.
A torque wrench was attached to the baseplate and each knee was pre-conditioned prior to taking the first measurement against a mounted protractor. Using the torque wrench, a rotational force of 3, 6 and 9 nm was then applied at 0°, 30°, 45°, 60° and 90° of knee flexion. This was repeated 3 times at each torque and knee flexion for both internal and external rotation for each specimen. The respective readings of the bone marker and skin pointer were recorded and analysed using SPSS for Windows using the Pearson correlation coefficient and the paired t-test.
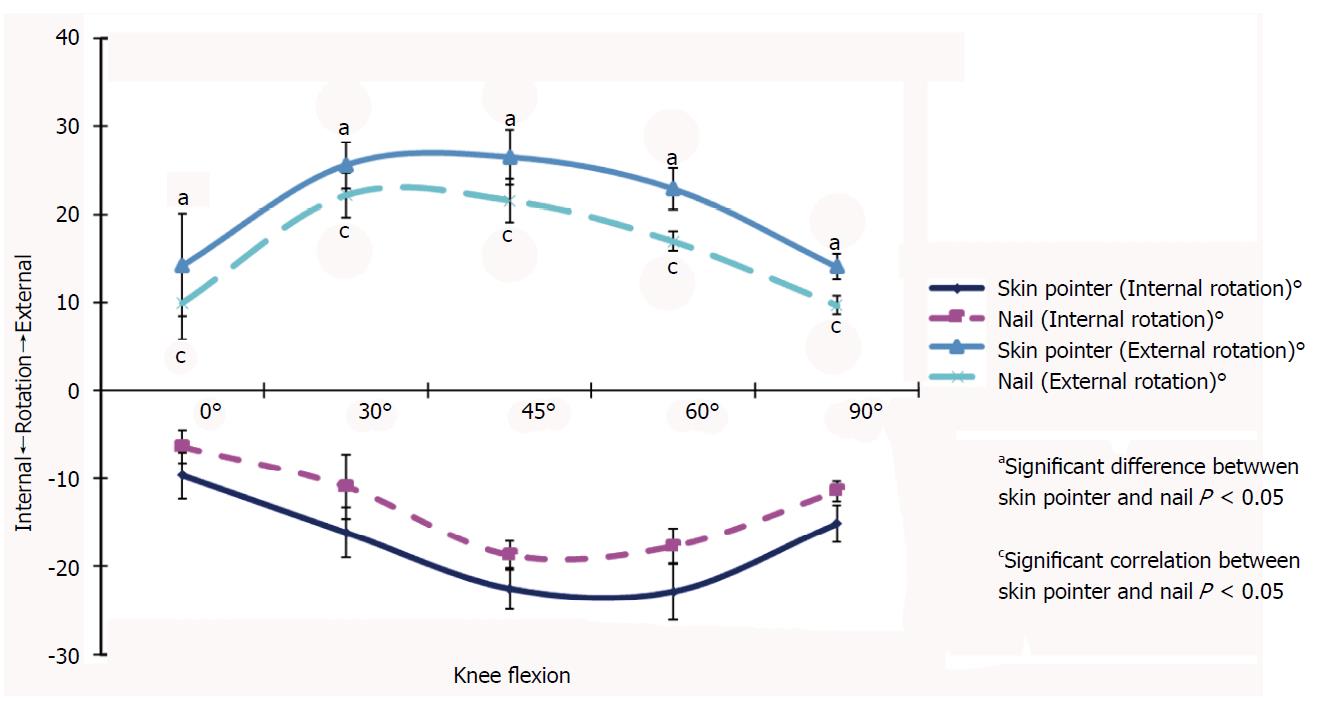
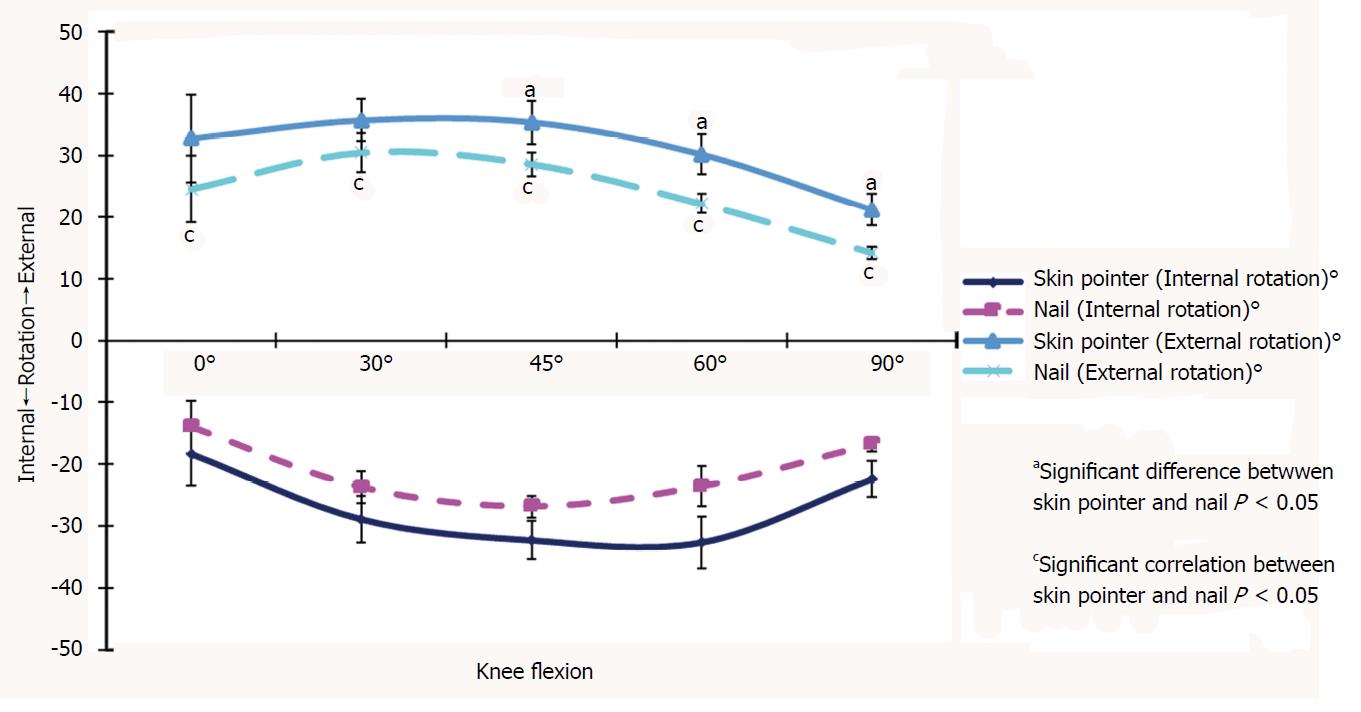
The readings for total rotation obtained with the skin pointer significantly correlated with that of the bone marker at 3 nm at 0°, 30°, 45°, 60°, and 90° of knee flexion (Table 1 and Figure 3). Similarly the readings for total rotation obtained with the skin pointer significantly correlated with that of the bone marker at 6 nm at 0°, 30°, 45°, 60° and 90° of knee flexion (Table 2 and Figure 4). However, although the readings between the skin pointer and bone marker correlated significantly at 3 nm of torque, there was a significant difference on paired t-test between the two readings through all degrees of flexion. With 6 nm of torque, there was a significant difference between the readings at 45°, 60° and 90° of flexion.
| Total rotation (°) | |||||
| Knee flexion (°) | Skin pointer | Nail | Pearson's r | r P-value | t-test P-value |
| 0 | 23.88 ± 25.99 | 16.33 ± 17.32 | 0.92 | 0.000 | 0.032 |
| 30 | 41.70 ± 15.49 | 33.06 ± 14.66 | 0.63 | 0.037 | 0.042 |
| 45 | 48.97 ± 16.97 | 40.30 ± 11.20 | 0.81 | 0.002 | 0.030 |
| 60 | 45.73 ± 17.45 | 34.70 ± 9.45 | 0.86 | 0.001 | 0.008 |
| 90 | 29.21 ± 10.89 | 21.15 ± 6.75 | 0.69 | 0.019 | 0.016 |
| Total rotation (°) | |||||
| Knee flexion (°) | Skin pointer | Nail | Pearson's r | r P-value | t-test P-value |
| 0 | 51.12 ± 37.73 | 38.61 ± 30.07 | 0.90 | 0 | 0.064 |
| 30 | 64.64 ± 21.61 | 54.27 ± 15.11 | 0.73 | 0.011 | 0.051 |
| 45 | 67.73 ± 20.60 | 55.48 ± 9.45 | 0.65 | 0.029 | 0.019 |
| 60 | 62.85 ± 22.43 | 45.79 ± 13.05 | 0.65 | 0.031 | 0.006 |
| 90 | 43.61 ± 17.56 | 30.97 ± 6.25 | 0.62 | 0.043 | 0.007 |
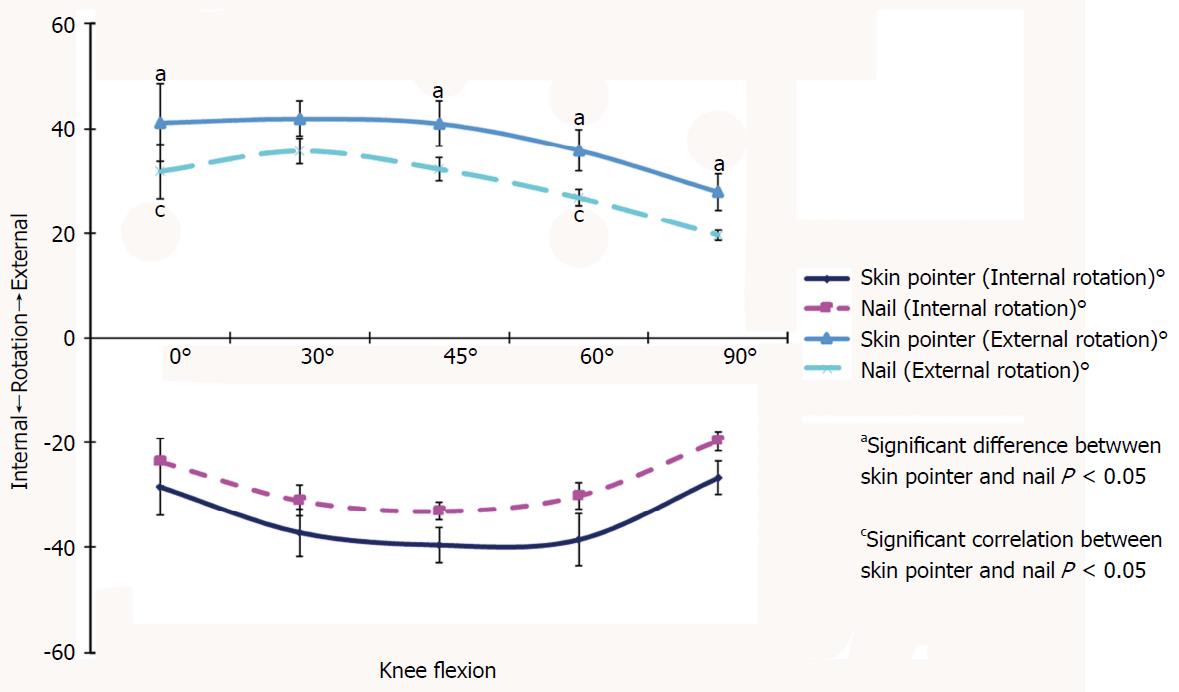
With 9 nm of torque, there was a statistically significant correlation at 0° and 60° but no statistically significant correlation at 30° and 90° of knee flexion though there was a similar trend to 3 and 6 nm of torque (Table 3 and Figure 5). With 9 nm of torque, there was a significant difference between the readings at 45°, 60° and 90° of flexion. We found that at 9 nm torque, the cadaveric specimen would not return to the neutral starting position, suggestive of deformation of the specimen.
| Total rotation (°) | |||||
| Knee flexion (°) | Skin pointer | Nail | Pearson's r | r P-value | t-test P-value |
| 0 | 69.67 ± 39.91 | 55.61 ± 30.61 | 0.86 | 0.001 | 0.046 |
| 30 | 79.18 ± 25.14 | 66.91 ± 15.42 | 0.59 | 0.055 | 0.072 |
| 45 | 80.67 ± 24.65 | 65.48 ± 11.23 | 0.51 | 0.112 | 0.040 |
| 60 | 74.52 ± 27.57 | 57.09 ± 11.50 | 0.77 | 0.006 | 0.017 |
| 90 | 54.70 ± 21.05 | 39.39 ± 8.22 | 0.55 | 0.079 | 0.018 |
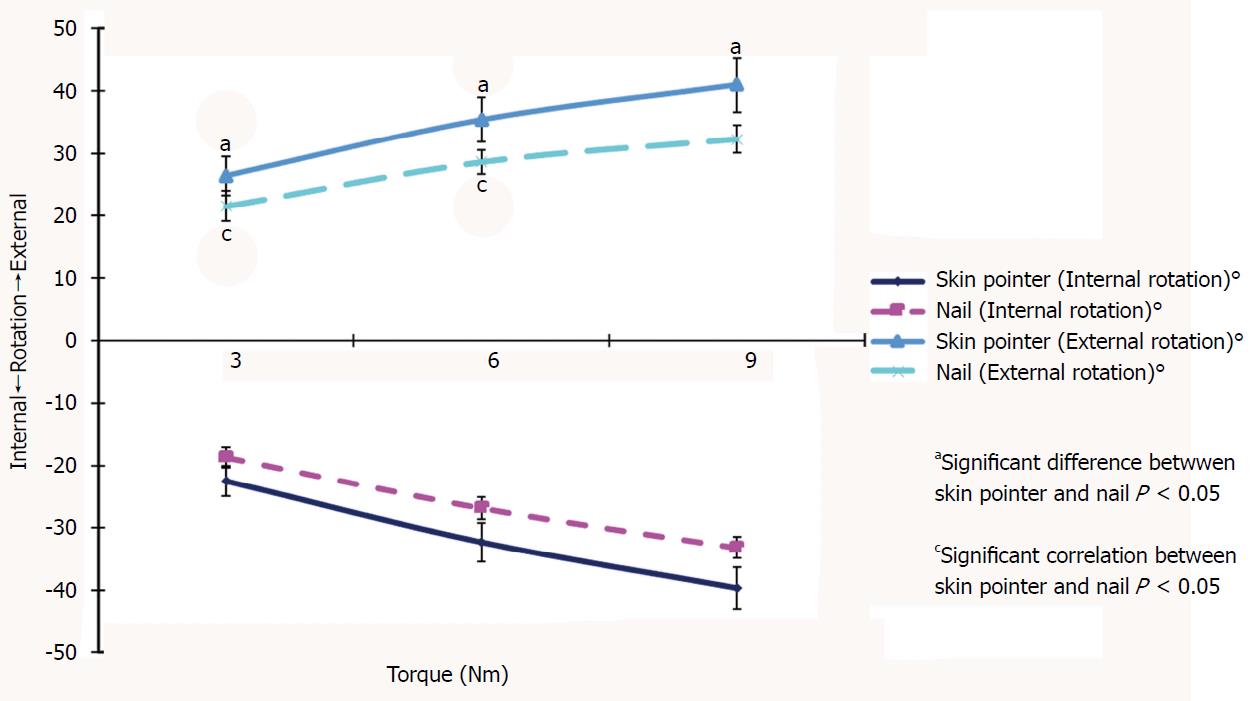
The skin pointer exaggerated the amount of rotation compared to the bone marker at all torques and angles of knee flexion with the maximum difference of 15.6° at 45° knee flexion with 9 nm of torque. For both the skin pointer and the bone marker, knee rotation increased with increasing knee flexion with maximum rotation at 45° flexion with subsequent decrease in rotation till 90° of knee flexion was reached (Figures 3-5). With increasing torque at a fixed flexion, knee rotation increased (Figure 6).
Apart from stress radiography with the use of RSA which is an invasive procedure, other instruments have been described to measure knee rotation including Almquist’s Rottometer from which our prototype jig is based on, Lars Rotational Laxiometer, Vermont Knee Laxity Device, Tsai et al[9]’s rotational knee laxity measurement device and Ahrens’ torsiometer[7,10-12].
Almquist’s Rottometer includes a chair where measurements were taken from the foot which may have contributed to its reported inaccuracy as ankle and foot rotation could still contribute to movement and readings[6,7]. The use of an Aircast® Foam Walker boot to immobilize the foot and ankle and the use of a skin pointer close to the knee joint as in our study would help to minimize systematic error from foot and ankle movement. Mouton et al[13,14] used a prototype rottometer with a similar ski boot and delivered the torque through a rotational handle bar and measured rotation through an inclinometer attached to the bar. Tsai’s device utilized a magnetic tracking system with an Aircast® Foam Walker boot with reliable results[9]. Ahrens’ utilized a torsiometer with Schanz pins to mount the cadaveric limbs skeletally with a potentiometer to measure rotation and demonstrated that cadaveric knees with arthroscopically resected ACLs had greater rotation than cadaveric knees with the ACL intact[12].
Robotic arm technology has also been described to deliver the rotational force to mimic the dial test[15,16]. The Rotab® device measures medial knee rotation when delivering an anterior translation force to measure anteromedial knee instablility[17]. A similar device which measures passive medial knee rotation with anterior translation of the tibia was described by Kurimura et al[18].
Hoshino et al[19] described a motion capture method using skin markers to measure the anterior translation of the distal femur in anaesthetised patients undergoing the pivot shift test.
Computer assisted surgery (CAS) devices which use motion-tracking technology and bony reference points can be used too but are invasive and are best used in the operating theatre during surgery[20,21]. The benefit of our setup is that it is simple to set-up, portable and does not rely on bulky electronic equipment allowing it to be used in the clinic and possibly at sports training grounds where a controlled environment with a ready electrical source may not be available.
Our study shows that our simple non-invasive skin pointer used in combination with our knee rotation jig can measure knee rotation similar to that of a skeletally placed marker with our knee rotation jig. We recognize that the skin pointer would exaggerate the amount of rotation compared to the bone marker due to movement of the soft tissue and skin overlying the bone. Hence although the readings between the skin pointer and the bone marker were significantly correlated with a similar trend, with higher torque and greater knee flexion, there were significant different between the individual measurements. We recognize too that 9 nm of torque may be not be well-tolerated in live human subjects due to pain. The effect of soft tissue causing an exaggeration of results has been reported previously[22]. Furthermore, 9 nm of torque may have caused deformation of our specimens affecting our results as a limitation of our use of cadavers which we may not observe in vivo.
Our jig and measurements assume a global single-axis of rotation of the knee, not taking into account translation of the knee which may occur in vivo with live subjects where rigid skeletal mounting to the jig will not be feasible. Hence off-axis movements may not be accurately measured as compared to a system where measurements are taken at both the femur and tibia taking into account movement of the subject in the jig. We recognize that the rotation axis of the tibia changes with knee as reported by Matsumoto and that our simple all-mechanical jig and measurement system may not be able to account for this change in axis[23]. Similar to Matsumoto’s study, we found that the magnitude of knee rotation increases as the knee is flexed which then decreases as flexion reaches 90°. Knee rotation was observed to be at its maximum at 45° of knee flexion and it increased with increasing torque. Similar to other previously described instruments, our device measures rotation without the effect of weight-bearing[7,9-11].
Our study compared the use of a skin pointer in combination with our knee rotation jig against a skeletally mounted marker which showed significant correlation between the two readings. We recognise the significant difference between the absolute values of the two different measurement methods due to soft tissue movement over the bone and that the soft tissue in a cadaver which has been frozen and thawed will have different properties compared to that of a live subject. Similar experiments with Rotatometers/Rottometers using only live subjects with no skeletally mounted reference for comparison demonstrate high inter- and intra-observer reliability[24,25].
Objective measurement for anterior-posterior laxity using the KT-1000 Arthrometer is well accepted[26-28]. Our aim is to eventually develop a portable and user-friendly device analogous to the KT-1000 which can be used for objective measurement of knee rotation in a non-invasive manner. The investigation of the utility of our rotation jig mated with a robotic arm for kinematic measurements is currently ongoing which may negate the effect of translation of the knee in vivo. Our next phase is to collect data on volunteers with uninjured knees followed by patients with knee injuries and patients after surgery to document changes in knee rotational laxity with pathology and treatment.
In conclusion, the skin pointer combined with a knee rotation jig can be a reliable and simple means of quantifying knee rotation in the cadaveric knee with potential application in vivo as a non-invasive means of measuring knee rotation in the clinic.
With double-bundle and anatomical single-bundle anterior cruciate ligament reconstruction for restoration of rotational knee kinematics, the need for objective clinical measurement of knee rotational laxity arises. Evaluation of knee rotation remains a challenge with intra-observer variability in the pivot shift test.
We aim to compare a non-invasive skin pointer with a knee rotation jig in cadaveric knees against a skeletally mounted marker.
Six pairs of cadaveric legs were mounted on a knee rotation jig. One Kirscher wire was driven into the tibial tubercle as a bone marker and a skin pointer was attached. Rotational forces of 3, 6 and 9 nm applied at 0°, 30°, 45°, 60° and 90° of knee flexion. Results were analysed using the Pearson correlation coefficient and paired t-test.
Total rotation recorded with the skin pointer significantly correlated with the bone marker at 3 nm at 0° (skin pointer 23.9 ± 26.0° vs bone marker 16.3 ± 17.3°, r = 0.92; P = 0.0), 30° (41.7 ± 15.5° vs 33.1 ± 14.7°, r = 0.63; P = 0.037), 45° (49.0 ± 17.0° vs 40.3 ± 11.2°, r = 0.81; P = 0.002), 60° (45.7 ± 17.5° vs 34.7 ± 9.5°, r = 0.86; P = 0.001) and 90° (29.2 ± 10.9° vs 21.2 ± 6.8°, r = 0.69; P = 0.019) of knee flexion and 6 nm at 0° (51.1 ± 37.7° vs 38.6 ± 30.1°, r = 0.90; P = 0.0), 30° (64.6 ± 21.6° vs 54.3 ± 15.1°, r = 0.73; P = 0.011), 45° (67.7 ± 20.6° vs 55.5 ± 9.5°, r = 0.65; P = 0.029), 60° (62.9 ± 22.4° vs 45.8 ± 13.1°, r = 0.65; P = 0.031) and 90° (43.6 ± 17.6° vs 31.0 ± 6.3°, r = 0.62; P = 0.043) of knee flexion and at 9 nm at 0° (69.7 ± 40.0° vs 55.6 ± 30.6°, r = 0.86; P = 0.001) and 60° (74.5 ± 27.6° vs 57.1 ± 11.5°, r = 0.77; P = 0.006). No statistically significant correlation with 9 nm at 30° (79.2 ± 25.1° vs 66.9 ± 15.4°, r = 0.59; P = 0.055), 45° (80.7 ± 24.7° vs 65.5 ± 11.2°, r = 0.51; P = 0.11) and 90° (54.7 ± 21.1° vs 39.4 ± 8.2°, r = 0.55; P = 0.079). We recognize that 9 nm of torque may be not tolerated in vivo due to pain.
We have measured knee rotation on a cadaveric knee utilising a knee rotation jig paired with a skin pointer against that of a skeletally mounted bone marker and have found a significant correlation between the two methods for the same magnitude of torque and knee flexion. We recognise that the use of the skin pointer introduces error due to movement of the soft tissue which increases with increasing torque.
Our aim is to eventually develop a portable and user-friendly device which can be used for objective measurement of knee rotation laxity in a non-invasive manner. This may entail the use of accelerometers or robotic arms to measure kinematics.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Singapore
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Angoules A S- Editor: Cui LJ L- Editor: A E- Editor: Tan WW
| 1. | Ahldén M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40:2230-2235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 293] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 2. | Araki D, Kuroda R, Kubo S, Fujita N, Tei K, Nishimoto K, Hoshino Y, Matsushita T, Matsumoto T, Nagamune K. A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop. 2011;35:439-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 3. | Kärrholm J. Roentgen stereophotogrammetry. Review of orthopedic applications. Acta Orthop Scand. 1989;60:491-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 269] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 4. | Selvik G. Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Acta Orthop Scand Suppl. 1989;232:1-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 421] [Cited by in RCA: 398] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 5. | Musahl V, Hoshino Y, Ahlden M, Araujo P, Irrgang JJ, Zaffagnini S, Karlsson J, Fu FH. The pivot shift: a global user guide. Knee Surg Sports Traumatol Arthrosc. 2012;20:724-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Almquist PO, Ekdahl C, Isberg PE, Fridén T. Knee rotation in healthy individuals related to age and gender. J Orthop Res. 2013;31:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Almquist PO, Arnbjörnsson A, Zätterström R, Ryd L, Ekdahl C, Fridén T. Evaluation of an external device measuring knee joint rotation: an in vivo study with simultaneous Roentgen stereometric analysis. J Orthop Res. 2002;20:427-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Almquist PO, Ekdahl C, Isberg PE, Fridén T. Measurements of knee rotation-reliability of an external device in vivo. BMC Musculoskelet Disord. 2011;12:291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Tsai AG, Musahl V, Steckel H, Bell KM, Zantop T, Irrgang JJ, Fu FH. Rotational knee laxity: reliability of a simple measurement device in vivo. BMC Musculoskelet Disord. 2008;9:35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Bleday RM, Fanelli GC, Giannotti BF, Edson CJ, Barrett TA. Instrumented measurement of the posterolateral corner. Arthroscopy. 1998;14:489-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Uh BS, Beynnon BD, Churchill DL, Haugh LD, Risberg MA, Fleming BC. A new device to measure knee laxity during weightbearing and non-weightbearing conditions. J Orthop Res. 2001;19:1185-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Ahrens P, Kirchhoff C, Fischer F, Heinrich P, Eisenhart-Rothe Rv, Hinterwimmer S, Kirchhoff S, Imhoff AB, Lorenz SG. A novel tool for objective assessment of femorotibial rotation: a cadaver study. Int Orthop. 2011;35:1611-1620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Mouton C, Theisen D, Seil R. Objective measurements of static anterior and rotational knee laxity. Curr Rev Musculoskelet Med. 2016;9:139-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Mouton C, Seil R, Agostinis H, Maas S, Theisen D. Influence of individual characteristics on static rotational knee laxity using the Rotameter. Knee Surg Sports Traumatol Arthrosc. 2012;20:645-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Branch T, Stinton S, Sternberg M, Hutton W, Lavoie F, Guier C, Neyret P. Robotic axial lower leg testing: repeatability and reproducibility. Knee Surg Sports Traumatol Arthrosc. 2015;23:2892-2899. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Stinton SK, Siebold R, Freedberg H, Jacobs C, Branch TP. The use of a robotic tibial rotation device and an electromagnetic tracking system to accurately reproduce the clinical dial test. Knee Surg Sports Traumatol Arthrosc. 2016;24:815-822. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Senioris A, Rousseau T, L’Hermette M, Gouzy S, Duparc F, Dujardin F. Validity of rotational laxity coupled with anterior translation of the knee: A cadaveric study comparing radiostereometry and the Rotab®. Knee. 2017;24:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Kurimura M, Matsumoto H, Fujikawa K, Toyama Y. Factors for the presence of anteromedial rotatory instability of the knee. J Orthop Sci. 2004;9:380-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Hoshino Y, Araujo P, Irrgang JJ, Fu FH, Musahl V. An image analysis method to quantify the lateral pivot shift test. Knee Surg Sports Traumatol Arthrosc. 2012;20:703-707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Colombet P, Robinson J, Christel P, Franceschi JP, Djian P. Using navigation to measure rotation kinematics during ACL reconstruction. Clin Orthop Relat Res. 2007;454:59-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 150] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 21. | Musahl V, Voos JE, O’Loughlin PF, Choi D, Stueber V, Kendoff D, Pearle AD. Comparing stability of different single- and double-bundle anterior cruciate ligament reconstruction techniques: a cadaveric study using navigation. Arthroscopy. 2010;26:S41-S48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Alam M, Bull AM, Thomas Rd, Amis AA. Measurement of rotational laxity of the knee: in vitro comparison of accuracy between the tibia, overlying skin, and foot. Am J Sports Med. 2011;39:2575-2581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Matsumoto H, Seedhom BB, Suda Y, Otani T, Fujikawa K. Axis location of tibial rotation and its change with flexion angle. Clin Orthop Relat Res. 2000;371:178-182. [PubMed] |
| 24. | Lorbach O, Wilmes P, Theisen D, Brockmeyer M, Maas S, Kohn D, Seil R. Reliability testing of a new device to measure tibial rotation. Knee Surg Sports Traumatol Arthrosc. 2009;17:920-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Chung JH, Ryu KJ, Lee DH, Yoon KH, Park YW, Kim HJ, Kim JH. An analysis of normative data on the knee rotatory profile and the usefulness of the Rotatometer, a new instrument for measuring tibiofemoral rotation: the reliability of the knee Rotatometer. Knee Surg Sports Traumatol Arthrosc. 2015;23:2727-2733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Robnett NJ, Riddle DL, Kues JM. Intertester reliability of measurements obtained with the KT-1000 on patients with reconstructed anterior cruciate ligaments. J Orthop Sports Phys Ther. 1995;21:113-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Sernert N, Kartus J, Köhler K, Ejerhed L, Karlsson J. Evaluation of the reproducibility of the KT-1000 arthrometer. Scand J Med Sci Sports. 2001;11:120-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Pugh L, Mascarenhas R, Arneja S, Chin PY, Leith JM. Current concepts in instrumented knee-laxity testing. Am J Sports Med. 2009;37:199-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 108] [Article Influence: 6.8] [Reference Citation Analysis (0)] |