Peer-review started: November 11, 2017
First decision: December 11, 2017
Revised: December 21, 2017
Accepted: March 1, 2018
Article in press: March 2, 2018
Published online: April 18, 2018
Processing time: 158 Days and 15.5 Hours
To develop practical guidelines for diagnosis and treatment of the painful snapping elbow syndrome (SE).
Clinical studies were searched in the databases PubMed and Scopus for the phrases “SE”, “snapping triceps”, “snapping ulnar nerve” and “snapping annular ligament”. A total of 36 relevant studies were identified. From these we extracted information about number of patients, diagnostic methods, patho-anatomical findings, treatments and outcomes. Practical guidelines for diagnosis and treatment of SE were developed based on analysis of the data. We present two illustrative patient cases-one with intra-articular pathology and one with extra-articular pathology.
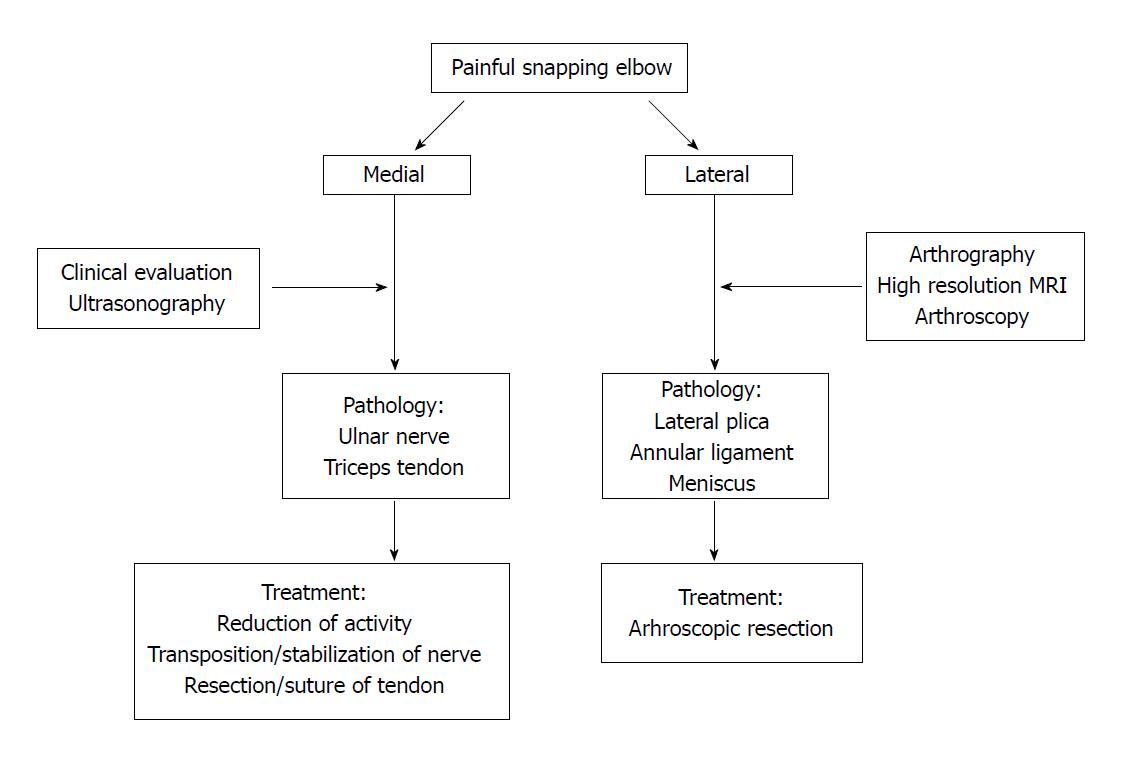
Snapping is audible, palpable and often visible. It has a lateral (intra-articular) or medial (extra-articular) pathology. Snapping over the medial humeral epicondyle is caused by dislocation of the ulnar nerve or a part of the triceps tendon, and is demonstrated by dynamic ultrasonography. Treatment is by open surgery. Lateral snapping over the radial head has an intra-articular pathology: A synovial plica, a torn annular ligament or a meniscus-like remnant from the foetal elbow. Pathology can be visualized by conventional arthrography, magnetic resonance (MR) arthrography, high resolution magnetic resonance imaging (MRI) and arthroscopy, while conventional MRI and radiographs often turn out normal. Treatment is by arthroscopic or eventual open resection. Early surgical intervention is recommended as the snapping can damage the ulnar nerve (medial) or the intra-articular cartilage (lateral). If medial snapping only occurs during repeated or loaded extension/flexion of the elbow (in sports or work) it may be treated by reduction of these activities. Differential diagnoses are loose bodies (which can be visualized by radiographs) and postero-lateral instability (demonstrates by clinical examination). An algorithm for diagnosis and treatment is suggested.
The primary step is establishment of laterality. From this follows relevant diagnostic measures and treatment as defined in this guideline.
Core tip: Elbow snapping is medial or lateral. Medial snapping is caused by dislocation of the ulnar nerve or a part of the triceps tendon, demonstrated clinically and by dynamic ultrasonography. Treatment is transposition of the nerve and/or resection of the snapping tendon. Lateral snapping is intra-articular by a synovial plica, a torn annular ligament or a meniscus-like remnant from the foetal elbow, demonstrated by arthrography, magnetic resonance arthrography, high resolution magnetic resonance imaging or arthroscopy. Treatment is arthroscopic resection. Early surgical intervention is recommended to reduce tissue damage. Medial snapping promoted by repeated, loaded activities might be treated by activity reduction.
- Citation: Bjerre JJ, Johannsen FE, Rathcke M, Krogsgaard MR. Snapping elbow-A guide to diagnosis and treatment. World J Orthop 2018; 9(4): 65-71
- URL: https://www.wjgnet.com/2218-5836/full/v9/i4/65.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i4.65
Snapping elbow (SE) is a rare condition, which can be confused with more common pathologies like an intra-articular free body, lateral epicondylitis or medial epicondylitis. Symptoms from SE occur during dynamic activities. Therefore, standard radiographs and magnetic resonance imaging (MRI) are often normal, leaving risk that the condition remains undiagnosed.
It is useful to distinguish between lateral and medial snapping, as pathology, diagnostic strategy and treatment are different in the two situations.
We suggest a practical guideline for diagnosis and treatment of SE, based on our own experience with three elbows in two patients and a review of the literature.
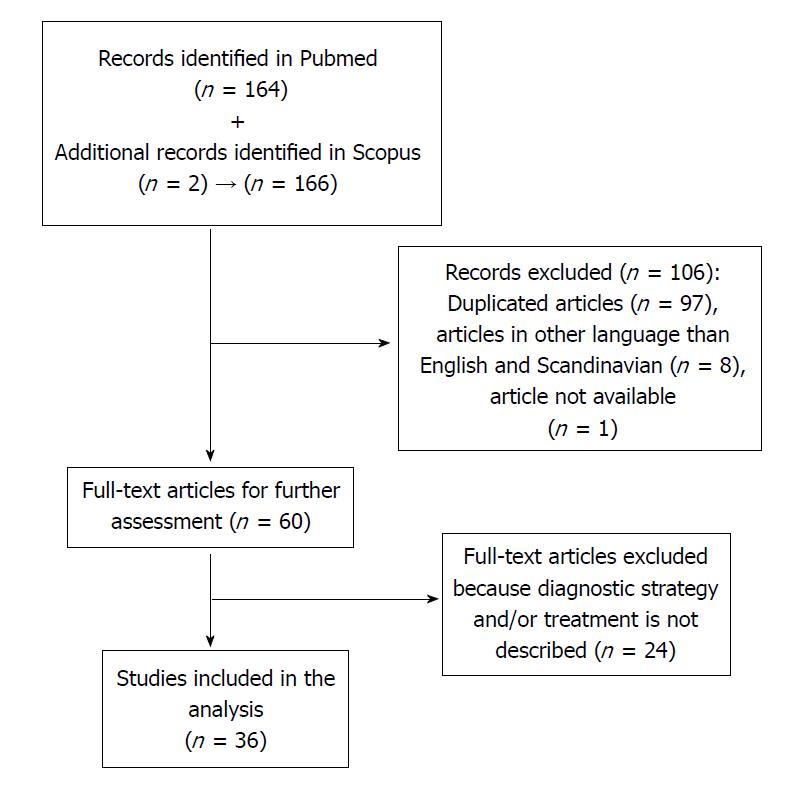
Literature was searched in Pubmed with four phrases: “SE” (resulting in 85 hits), “snapping triceps” (39 hits), “snapping ulnar nerve” (31 hits) and “snapping annular ligament” (9 hits). A similar search was performed in Scopus, and two additional, relevant articles were identified. We excluded papers that had no information about diagnostic strategy or treatment as well as articles in other languages than English or Scandinavian.
One article was not available online or from the author.
From the 36 remaining articles (Figure 1) information about number of patients, diagnostic method, patho-anatomical findings, treatments and outcomes was extracted.
We treated two cases with principally different reasons for snapping.
A 16-year-old boy with painful locking of the right elbow during 2-3 years. No trauma in history. Standard MR scanning and radiographs were normal. A sore clicking was found at the lateral epicondyle with 80°-90° of elbow flexion, and it was most painful with simultaneous pronation. He had similar but milder symptoms on the left side. Both elbows were stable and with normal range of motion.
Dynamic ultrasound raised suspicion of a tight, lateral part of the triceps tendon as the cause of snapping. However, extraarticular injection of 1 cc Carbocain plus 1 cc of Depomedrol® in this area did not relieve the symptoms.
At arthroscopy an inter-positioned lunar plica antero-laterally (video 1) was resected, and a tight chord of capsule in relation to the plica was loosened.
Pain and snapping disappeared after the operation. A similar condition was treated by artroscopy in the left elbow 6 wk later. At 3-years follow-up he felt a slight tenderness in the right elbow from time to time, but it was different from his preoperative pain and he had no snapping. The left elbow was symptom free.
A 16-year-old boy with painful medial elbow clicking bilaterally for over a year, in particular during heavy resistance training of the triceps muscle. The snapping was mildly painful, but he had post-exercise pain that forced him to reduce the training load. Popping of the triceps muscle over the medial epicondyle at 110° of flexion was suspected by clinical examination (video 2). There were no neurological symptoms and a negative Tinel’s test in relation to the ulnar nerve. Dynamic sonography visualized the popping tissue (video 3), but it was not possible to distinguish if this originated from the ulnar nerve or a part of the triceps tendon. The elbow appeared otherwise normal.
Open surgery showed that snapping was caused by dislocation of the ulnar nerve (video 4). The sulcus was therefore deepened 3 mm, the nerve was repositioned, and a part of the medial triceps tendon was trans-positioned to form a cover over the sulcus. This resolved the snapping condition, and the patient was able to exercise normally between two and five months postoperatively. Then a feeling of instability of the nerve during heavy resistance training occurred, but it was pain free. One year after the operation he stopped regular training and had no symptoms. This was still the case at 3-years follow-up. Both patients declared, that they were satisfied with the treatment, and with their present experience they would agree to be operated for SE again, if necessary.
The identified clinical reports of SE are summarized in the tables. They are divided into lateral, intra-articular cases (Table 1) and medial, extra-articular cases (Table 2) of SE. There are 105 cases of lateral snapping with a mean age of 39.7 years (range 11-66) and 42 cases of medial snapping with a mean age of 28.7 years (range 9-65). In some patients SE was presumably triggered by athletic performance (throwing and tennis typical for lateral snapping, and weightlifting, decathlon and dumbbell exercises for medial snapping). However, the majority of cases could not be connected to sports.
| Report and year | No. of patients | Snapping Pathology | Diagnostic procedure | Treatment | Results |
| Akagi et al[1], 1998 | One | Snapping plica | Arthrogram, arthroscopy | Open arthrotomy | Complete recovery |
| Antuna et al[2], 2001 | Fourteen | Snapping plica | MRI, arthroscopic examination | Arthroscopic resection | Ten complete recoveries, two partial recoveries, two failures |
| Aoki et al[3], 2003 | Two | Snapping annular ligament | Arthroscopic examination | One had arthroscopic resection | One complete recovery after resection |
| Chai et al[4], 2004 | One | Snapping annular ligament | Ultrasonography | Arthroscopic resection | Relief of snapping |
| Fukase et al[13], 2005 | One | Snapping plica | Special MRI1 | Open resection | Complete recovery |
| Huang et al[5], 2005 | One | Snapping meniscus | MR-arthrography | Arthroscopic resection | Complete recovery |
| Huang et al[6], 2005 | One | Snapping annular ligament | MRI, arthroscopic examination | Arthroscopic resection | Relief of snapping, less pain |
| Kang et al[7], 2010 | Two | Snapping meniscus | MRI, arthrography | Arthroscopic resection | Complete recovery |
| Maruyama et al[8], 2010 | One | Snapping annular ligament | Arthroscopy | Arthroscopic release of the ligament | Complete recovery |
| Brahe Pedersen et al[9], 2017 | Sixtyfour | Hypertrophic synovial plica | Clinical examination and ultrasound | Arthroscopic resection | Significant improvement in Oxford Elbow score after 3 and 22 mo |
| Shinohara et al[14], 2010 | One | Tight fibrous structure | MRI, arthroscopy | Arthroscopic resection | Complete recovery |
| Steinert et al[10], 2008 | Three | Hypertrophic synovial plica | Contrast MRI (in two), arthroscopy | Arthroscopic resection | Complete recovery |
| Tateishi et al[11], 2005 | One | Snapping plica | MRI, arthrogram | Open resection | Complete recovery |
| Report and year | No. of cases | Snapping pathology | Diagnostic procedure | Treatment | Results |
| Anand et al[16], 2012 | One | Snapping ulnar nerve | Open surgery | Transposition of nerve | Complete recovery, returned to elite sport |
| Cesmebasi et al[35], 2015 | Four | Snapping medial antebrachial cutaneous nerve (4), triceps (3) and ulnar nerve (3) | Open surgery/sonography | Open decompression, stabilization or transposition of nerves, resection of tendon | Improvement (mild persistent symptoms to complete recovery) |
| Chuang et al[17], 2016 | One | Snapping triceps and subluxing ulnar nerve | Dynamic sonography | NSAIDs and reduction in repetitive elbow flexion activities at work | Partial improvement |
| Dreyfuss et al[18], 1978 | Two | Snapping triceps | Open reinsertion of the snapping part of the triceps | Reinsertion of the snapping tendon | 1 complete recovery, 1 partial |
| Haws et al[30], 1995 | One | Snapping triceps | Open exploration | Open resection of tendon | Complete recovery |
| Hayashi et al[19], 1984 | One | Snapping triceps | Physical examination, radiographs, open surgery | Medial epicondylectomy and division of tendon | Complete recovery |
| Jacobson et al [20], 2001 | Three | Snapping ulnar nerve, snapping triceps | Dynamic sonography | Open “surgical treatment for each abnormality” | Not reported |
| Lasecki et al[21], 2014 | One | Snapping triceps and ulnar nerve | MRI and dynamic sonography | Not reported | Not reported |
| Minami et al[31], 1999 | One | Snapping triceps | Not reported | Open tendon resection | Complete recovery |
| Reis et al[22], 1980 | One | Snapping triceps | Open surgery | Open tendon resection | Complete recovery |
| Rolfsen[23], 1970 | One | Snapping triceps | Open surgery | Open tendon resection | Complete recovery |
| Spinner et al[32], 2001 | One | Snapping triceps | Physical examination | Open tendon Excision | Complete recovery |
| Spinner et al[24], 1999 | Two | Snapping triceps | Physical examination, MRI | Reduction in weight lifting | Symptoms only appeared during weight lifting |
| Spinner et al[33], 1999 | One | Snapping triceps lateral | Palpation and MRI | Open tendon resection | Complete recovery |
| Spinner et al[25], 2000 | Fifteen | Snapping triceps after operation for snapping ulnar nerve | Physical examination, MRI | Lateral transposition or excision of tendon (nine patients), six refused surgery | Complete relief of snapping in surgically treated patients. No relief in non-operated |
| Watts et al[34], 2009 | Three | Snapping triceps | Open exploration | Excision (two), tendon division (one) | Complete recovery |
| Xarchas et al[26], 2007 | Three | Snapping ulnar nerve | Palpation | Anterior nerve transposition (two), NSAIDS and change of job as waitress (one) | Complete recovery after surgery. Not reported for non-surgery |
This review does not allow to make an estimate of the incidence of SE, but based on the reported cases, the different pathologies can be ranked with intraarticular plica as the most common, followed by medially snapping triceps (rare), snapping ulnar nerve (rare), snapping annular ligament (very rare) and extremely rare pathologies: snapping medial antebrachial cutaneous nerve, intraarticular meniscus and laterally snapping triceps.
Intra-articular snapping is caused by annular ligament pathology, lateral meniscal remnants or hypertrophic synovial plicas[1-12]. Clicking due to dynamic impingement of these soft tissues is difficult to demonstrate with static MRI.
Three reports describe snapping caused by anomalous meniscal remnants[5,7]. Standard MRI did not reveal the pathology, but it was demonstrated by MRI- and radiographic arthrography, respectively.
In one report a plica was demonstrated by radiographic arthrography and MRI as a protruding shadow[11]. Contrast MRI was used to diagnose three cases of a snapping plica[10]. In one case conventional MRI raised suspicion of a small, pathological structure, which was diagnosed as a plica by high-resolution MRI[13].
By conventional MRI it was in most cases not possible to visualize lateral SE pathology, and diagnoses were established with MR-arthrography, high resolution MRI or radiographic arthrography. With arthroscopy the intra-articular snapping pathology can be visualized and treated in the same procedure by resection of the snapping tissue.
Arthroscopic resection of plicas or meniscus-like tissues was standard treatment, except in three cases of open resection. Reported results were good with either method (Table 1), as elbow function normalized in the majority of cases.
One patient who had postero-lateral rotatory elbow instability did not improve, but the snapping might have been caused by instability and not by intra-articular pathology[2].
Subluxation of either the ulnar nerve or a medial part of the triceps tendon, or of both can cause extra-articular snapping of the elbow[15-26]. In many cases it can be recognized by thorough physical examination. The ulnar nerve snaps in the interval 70-90 degrees of flexion, and the triceps around 115 degrees. These snaps are usually visible and audible[27]. By dynamic ultrasound and dynamic MRI[28] the snapping tissue can be visualized, but interpretation of the anatomical structures is not always conclusive, as described in our case 2[20,27,28]. Dislocation of the snapping structure is not visible on standard MRI with the elbow extended, but with the elbow flexed dislocation can often be demonstrated[29].
A snapping triceps can be treated by either resection[19,22-23,25,30-34] or by suture of the snapping part to the main tendon[18,25]. Medial epicondylectomy was used in one case[19]. Ulnar nerve dislocation was treated by anterior transposition[16,26,35] or fixation of the nerve in the deepened cubital tunnel[35].
One case series reported snapping of the medial antebrachial cutaneous nerve[35] that is medial to the medial humeral condyle (and not posterior as the ulnar nerve). There were no neurological symptoms reported from this nerve, and snapping was observed intra-operatively. In three of the four patients there was also snapping of triceps and the ulnar nerve. In retrospective review of the preoperative ultrasonography investigations, snapping of the medial antebrachial cutaneous nerve could be identified. In three patients the medial antebrachial cutaneous nerve was transpositioned and in one it was decompressed, while triceps- and ulnar nerve dislocation was also treated in three.
The most common symptoms were pain and painful snapping, and neurological symptoms from the ulnar nerve were rarely reported.
It is useful to divide snapping of the elbow joint into lateral and medial snapping, as these are caused by different pathological conditions and can easily be distinguished clinically (Figure 2).
Generally, intra-articular snapping pathology cannot be demonstrated by conventional MRI, and MR-arthrography, high resolution MRI or radiographic arthrography is necessary[1,6,9,13].
In a series with 14 patients treated for lateral, intra-articular plicas snapping over the radial head by arthroscopic resection[2], ten patients were completely relieved of their symptoms, two still experienced mild pain and one was asymptomatic for 4 years, but then experienced recurrence of symptoms. In one patient treatment failed, but he was subsequently diagnosed with postero-lateral instability as the possible cause of the snapping phenomenon. In the largest series reported[9] with 64 patients, there was a significant and clinically relevant increase in Oxford Elbow Score three and 22 mo after operation. Therefore, surgical treatment of the lateral SE is successful in the majority of cases, and it should preferably be performed arthroscopically, as this permits optimal visualization of the joint and minimize morbidity. Non-surgical treatment has not been described for lateral SE.
Dynamic ultrasonography is the best to visualize medial snapping, but it can be difficult to identify which anatomic structure that is snapping (as described in case 2)[20,25,27]. Fabrizio et al[36] reported a variation of the triceps brachii with a thin fourth muscular head inserting on the medial part of the olecranon as a cause of medial snapping. An accessory snapping triceps tendon can clinically be confused with snapping of the ulnar nerve, as the two structures are closely located at the medial epicondyle. Watts described this diagnostic pitfall in a report of three cases[34], of which two primary had transposition of the ulnar nerve and one a fixation of the nerve in the ulnar sulcus. In all three cases snapping persisted, and the cause was identified as a discrete accessory tendon originating from the triceps. The authors concluded from their series that a subluxing ulnar nerve does not snap, and that medial snapping is always caused by anterior sliding of a strip of the triceps tendon during elbow flexion.
Snapping of a medial part of the triceps muscle is recognized as a reason for continuous snapping after ulnar nerve transposition[22-23,25,30-32,34]. It is unclear in these cases if the snapping triceps was unrecognised during ulnar nerve surgery or if it was a complication to dissection of the tendon during release of the ulnar nerve. However, we and others present cases of medial snapping, treated successfully by ulnar nerve surgery[20,26]. Therefore, the triceps should always be inspected in flexion and extension of the elbow during surgery for ulnar nerve snapping.
It is unknown to which extend the medial antebrachial cutaneous nerve is involved in medial snapping, as there is only one case report of this nerve as snapping structure[35]. It is challenging to decide by ultrasonography which anatomical structure that causes medial snapping[35] and the final diagnosis is established during operation. All snapping pathologies should be addressed.
Medial snapping in persons with repeated or loaded activities involving elbow flexion and extension during work (e.g., a waitress, a postman) or sports (weightlifting, body building) can be treated by reduction of these activities[17,24,26]. In other cases, surgical intervention should preferably be early, as intra-articular pathologies can lead to damage of the cartilage, and snapping of the ulnar nerve can lead to neuropathy[12,25].
Intra-articular loose bodies and postero-lateral elbow instability can cause locking, which may be interpreted as lateral snapping[2,12]. Radiographs and CT are useful to identify intra-articular loose bodies, while postero-lateral instability is a clinical diagnosis. Also, lateral snapping is sometimes treated as epicondylitis, which is not a snapping condition.
In conclusion, SE is clinically divided into intra-articular (lateral) and extra-articular (medial) cases, based on the location of snapping. Intra-articular pathology is best visualized with high-resolution MRI, MR arthrography or radiographic arthrography. Arthroscopic or open resection of the pathological tissue is successful in most cases. Extra-articular pathology is best diagnosed by dynamic ultrasonography and during surgery. Solitary snapping of the ulnar nerve is extremely rare, and a triceps associated snapping tendon should always be suspected. Treatment is by open surgery.
Patients with snapping elbow (SE) are seen by orthopaedic surgeons, rheumatologists and physical therapists, but the diagnosis is rare.
Most health care workers have no clinical experience with SE, as it is a rare condition. Therefore, there is a risk of misdiagnosis and delay of relevant treatment. Snapping can be visible, audible and palpable, but usual diagnostic measures can fail to demonstrate pathology.
From a literature search combined with our own clinical experience we wanted to analyse what is known about SE, its diagnosis and its treatment. The main purpose was to present a guideline to identify the patho-anatomical cause of SE, its general binary categorization and the best treatment of each pathology.
Literature was searched in PubMed and Scopus and key points in diagnosis and treatment were identified. Two typical cases are described.
Our review indicates that SE should be clinically divided into lateral and medial, and that diagnosis and treatment is a logic consequence of this. Lateral, intra-articular pathology is best diagnosed with high-resolution MRI, MR-arthrography or radiographic arthrography. Surgical intervention is the treatment of choice and successful in the majority of the cases. Medial, extra-articular pathology is best diagnosed by dynamic ultrasonography and during surgery. It is most commonly caused by subluxation of a medial part of the triceps tendon or the ulnar nerve. Treatment is by open surgery, except in patients with repeated, loaded activities during flexion and extension (at work or during sports), in which case symptoms may resolve by reduction of this activity.
This guideline suggests a standardized approach to diagnosis and treatment of patients with SE. As early surgical intervention is recommended because the snapping can damage nerve (medial) or cartilage (lateral), this guideline is a tool for better patient care.
There are no randomized studies on treatment of SE, but the largest series of 64 cases is on lateral SE, meaning that randomized controlled studies could be performed regarding treatment of this pathology. The other pathologies are too rare. There are probably many undiagnosed cases, and studies on incidence would describe the magnitude of this health problem.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Denmark
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kodde IF, Papachristou GC, Sinha A S- Editor: Cui LJ L- Editor: A E- Editor: Li D
| 1. | Akagi M, Nakamura T. Snapping elbow caused by the synovial fold in the radiohumeral joint. J Shoulder Elbow Surg. 1998;7:427-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Antuna SA, O’Driscoll SW. Snapping plicae associated with radiocapitellar chondromalacia. Arthroscopy. 2001;17:491-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 85] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Aoki M, Okamura K, Yamashita T. Snapping annular ligament of the elbow joint in the throwing arms of young brothers. Arthroscopy. 2003;19:E4-E7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Chai JW, Kim S, Lim HK, Bae KJ. Ultrasonographic diagnosis of snapping annular ligament in the elbow. Ultrasonography. 2015;34:71-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 5. | Huang GS, Lee CH, Lee HS, Chen CY. A meniscus causing painful snapping of the elbow joint: MR imaging with arthroscopic and histologic correlation. Eur Radiol. 2005;15:2411-2414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Huang GS, Lee CH, Lee HS, Chen CY. MRI, arthroscopy, and histologic observations of an annular ligament causing painful snapping of the elbow joint. AJR Am J Roentgenol. 2005;185:397-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Kang ST, Kim TH. Lateral sided snapping elbow caused by a meniscus: two case reports and literature review. Knee Surg Sports Traumatol Arthrosc. 2010;18:840-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Maruyama M, Takahara M, Kikuchi N, Ito K, Watanabe T, Ogino T. Snapping elbow with congenital radial head dislocation: case report. J Hand Surg Am. 2010;35:981-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Brahe Pedersen J, Kristensen PK, Mønsted P, Thillemann TM. Short-term results after arthroscopic resection of synovial plicae in the radiohumeral joint: a case series of 64 procedures. SICOT J. 2017;3:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Steinert AF, Goebel S, Rucker A, Barthel T. Snapping elbow caused by hypertrophic synovial plica in the radiohumeral joint: a report of three cases and review of literature. Arch Orthop Trauma Surg. 2010;130:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Tateishi K, Tsumura N, Matsumoto T, Fujioka H, Kokubu T, Kuroda R, Shiba R, Kurosaka M. Bilateral painful snapping elbows triggered by daily dumbbell exercises: a case report. Knee Surg Sports Traumatol Arthrosc. 2006;14:487-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Ruch DS, Papadonikolakis A, Campolattaro RM. The posterolateral plica: a cause of refractory lateral elbow pain. J Shoulder Elbow Surg. 2006;15:367-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Fukase N, Kokubu T, Fujioka H, Iwama Y, Fujii M, Kurosaka M. Usefulness of MRI for diagnosis of painful snapping elbow. Skeletal Radiol. 2006;35:797-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Shinohara T, Horii E, Tatebe M, Yamamoto M, Okui N, Hirata H. Painful snapping elbow in patients with congenital radioulnar synostosis: report of two cases. J Hand Surg Am. 2010;35:1336-1339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Kang JH, Joo BE, Kim KH, Park BK, Cha J, Kim DH. Ultrasonographic and Electrophysiological Evaluation of Ulnar Nerve Instability and Snapping of the Triceps Medial Head in Healthy Subjects. Am J Phys Med Rehabil. 2017;96:e141-e146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Anand A, Campion NJ, Chakraverty R, Pimpalnerkar A. Bilateral snapping ulnar nerve syndrome in a professional decathlete – a rare case report and a review of the literature. Eur Orthop Traumatol. 2012;3:263-266. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Chuang HJ, Hsiao MY, Wu CH, Özçakar L. Dynamic Ultrasound Imaging for Ulnar Nerve Subluxation and Snapping Triceps Syndrome. Am J Phys Med Rehabil. 2016;95:e113-e114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Dreyfuss U, Kessler I. Snapping elbow due to dislocation of the medial head of the triceps. A report of two cases. J Bone Joint Surg Br. 1978;60:56-57. [PubMed] |
| 19. | Hayashi Y, Kojima T, Kohno T. A case of cubital tunnel syndrome caused by the snapping of the medial head of the triceps brachii muscle. J Hand Surg Am. 1984;9A:96-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 42] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Jacobson JA, Jebson PJ, Jeffers AW, Fessell DP, Hayes CW. Ulnar nerve dislocation and snapping triceps syndrome: diagnosis with dynamic sonography--report of three cases. Radiology. 2001;220:601-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 121] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 21. | Łasecki M, Olchowy C, Pawluś A, Zaleska-Dorobisz U. The Snapping Elbow Syndrome as a Reason for Chronic Elbow Neuralgia in a Tennis Player - MR, US and Sonoelastography Evaluation. Pol J Radiol. 2014;79:467-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Reis ND. Anomalous triceps tendon as a cause for snapping elbow and ulnar neuritis: a case report. J Hand Surg Am. 1980;5:361-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Rolfsen L. Snapping triceps tendon with ulnar neuritis. Report on a case. Acta Orthop Scand. 1970;41:74-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 43] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Spinner RJ, Wenger DE, Barry CJ, Goldner RD. Episodic snapping of the medial head of the triceps due to weightlifting. J South Orthop Assoc. 1999;8:288-292. [PubMed] |
| 25. | Spinner RJ, O’Driscoll SW, Jupiter JB, Goldner RD. Unrecognized dislocation of the medial portion of the triceps: another cause of failed ulnar nerve transposition. J Neurosurg. 2000;92:52-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Xarchas KC, Psillakis I, Koukou O, Kazakos KJ, Ververidis A, Verettas DA. Ulnar nerve dislocation at the elbow: review of the literature and report of three cases. Open Orthop J. 2007;1:1-3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Spinner RJ, Goldner RD. Snapping of the medial head of the triceps: diagnosis and treatment. Tech Hand Up Extrem Surg. 2002;6:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Guillin R, Marchand AJ, Roux A, Niederberger E, Duvauferrier R. Imaging of snapping phenomena. Br J Radiol. 2012;85:1343-1353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Spinner RJ, Hayden FR Jr, Hipps CT, Goldner RD. Imaging the snapping triceps. AJR Am J Roentgenol. 1996;167:1550-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Haws M, Brown RE. Bilateral snapping triceps tendon after bilateral ulnar nerve transposition for ulnar nerve subluxation. Ann Plast Surg. 1995;34:550-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Minami A, Kato H, Iwasaki N. Snapping of Triceps Tendon After Anterior Nerve Transposition for Recurrent Subluxation of the Ulnar Nerve. Hand Surg. 1999;4:193-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Spinner RJ, Gabel GT. Latrogenic snapping of the medial head of the triceps after ulnar nerve transposition. J South Orthop Assoc. 2001;10:236-240. [PubMed] |
| 33. | Spinner RJ, Goldner RD, Fada RA, Sotereanos DG. Snapping of the triceps tendon over the lateral epicondyle. J Hand Surg Am. 1999;24:381-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 34. | Watts AC, McEachan J, Reid J, Rymaszewski L. The snapping elbow: a diagnostic pitfall. J Shoulder Elbow Surg. 2009;18:e9-e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Cesmebasi A, O’driscoll SW, Smith J, Skinner JA, Spinner RJ. The snapping medial antebrachial cutaneous nerve. Clin Anat. 2015;28:872-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 36. | Fabrizio PA, Clemente FR. Variation in the triceps brachii muscle: a fourth muscular head. Clin Anat. 1997;10:259-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |