Peer-review started: December 25, 2017
First decision: January 6, 2018
Revised: January 12, 2018
Accepted: February 4, 2018
Article in press: February 5, 2018
Published online: March 18, 2018
Processing time: 81 Days and 10.8 Hours
To investigate that the increased intracapsular pressure, during the delay period, can interrupt the blood flow to the femoral head.
An observational retrospective study included a group of 17 patients with traumatic hip dislocation, their ages at time of injury averaged 26 (range from 3 to 70) years. Outcomes were assessed clinically and radiographically at a period averaged 11.5 (range from 4 to 20) years.
Minor trauma caused dislocation in seven and severe trauma in ten patients. All dislocations were posterior, six isolated dislocation and 11 were associated with other injuries. The negligence period averaged 2.5 (ranged from 1 to 4) d. At the latest visit, the radiography revealed normal hip in 11 and avascular necrosis (AVN) in six patients. Clinically, eight patients were rated as excellent, three good, three fair and three poor.
We believe the factors that contribute to increased intracapsular pressure also increase the influence of delayed reduction toward the development of AVN.
Core tip: Factors influencing outcomes of traumatic hip dislocation include reduction time, the severity of trauma, patients’ ages and direction of dislocation. Although these factors have been thoroughly investigated, any of them was not assigned as the causative for the development of the avascular necrosis (AVN). Does the increased intracapsular pressure is the foremost factor? We believe that the factors as hemarthrosis, the position of the limb during the pre-reduction period particularly in posterior dislocation and traction in post-reduction period can increase the intracapsular pressure to a level sufficient for occlusion of intracapsular blood vessels. Delayed reduction accentuates influence of increased intracapsular pressure in favour of the development of AVN.
- Citation: Massoud EIE. Neglected traumatic hip dislocation: Influence of the increased intracapsular pressure. World J Orthop 2018; 9(3): 35-40
- URL: https://www.wjgnet.com/2218-5836/full/v9/i3/35.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i3.35
As the hip is an inherently stable joint, a substantial force is required for its dislocation. Therefore, associated injuries must be sought[1,2]. However, some biological factors can predispose to dislocation even with minor trauma, for instance, increased the head-shaft angle and diminished or increased femoral torsion[3-5]. In children, hip dislocates mostly after relatively trivial accidents such as slipping or tripping[2,6]. Consequently, the associated injuries are uncommon. The prominence of the associated injury or insignificance of the causative trauma leads to the negligence of hip dislocation[6,7].
There is almost a consensus regarding the prompt reduction of the dislocated hip in order to minimize the incidence of avascular necrosis (AVN)[6-9]. However, an experimental study reported that the reduction time did not consider a critical factor in the appearance of AVN[10].
Effusion of the hip joint was detected with traumatic dislocation at about 35 d post injury[11]. The effusion increases the intracapsular pressure to a level sufficient for tamponade of the retinacular blood vessels[2,11,12]. Likewise, placement of the injured limb in the particular positions during the pre and/or post-reduction periods can tighten the capsule, which increases the intracapsular pressure[13-15]. These reasons explain why some authors noted AVN despite early reduction[6,9].
Over a period of twenty-year, we observed a group of patients with missed traumatic hip dislocations. Although all hips were reduced late and received the same post reduction management, however, only about 35% developed AVN. Therefore, we hypothesized that the delayed reduction is not only the direct factor that contributes to the development of AVN. However, the factors that increase intracapsular pressure may play an important role in the development of AVN.
In order to investigate our hypothesis, we present this study using the patients’ records as a source of the outcomes.
Between February 1993 and March 2013, we have observed and followed a group of 17 patients with a neglected traumatic hip dislocation. Local Ethics Committee approved this retrospective study. Patients were not required to give informed consent to the study because the analysis used anonymous clinical data. The included patients are seven females and ten males their ages at time of injury averaged 26 (range from 3 to 70) years. Baseline details are listed in Table 1. The causative trauma was graded into minor trauma as running, tripping or falling and severe trauma as high-energy impact, crushing, excessive speed (cycling) or excessive force (football)[7]. Dislocation was classified according to the direction into anterior, posterior and central. Then the posterior dislocation was classified according to the Thompson-Epstein classification system[16]. Additionally, dislocation was classified as an isolated or associated with other injuries, which were then classified into polytrauma, or injuries related to the dislocated side as sciatic nerve injury, femoral fractures or knee injuries. Negligence period was estimated from time of the trauma to the time of the certain reduction.
| No. | Baseline data | Outcomes | ||||||||
| Age | Sex | NP in days | Trauma | Dislocation type | Associated injury | Follow-up period, yr | Clinical | Radiologic | ||
| Score | Rating | |||||||||
| 1 | 3 | M | 4 | Minor | T-E type 1 | Isolated | 20 | 18 point | Excellent | Normal |
| 2 | 33 | M | 3 | Severe | T-E type 1 | Polytrauma | 18 | 14 point | Fair | AVN |
| 3 | 5 | F | 3 | Minor | T-E type 1 | Isolated | 18 | 18 point | Excellent | Normal |
| 4 | 27 | M | 2 | Severe | T-E type 1 | Polytrauma | 16 | 12 point | Poor | AVN |
| 5 | 55 | M | 1 | Severe | T-E type 4 | Polytrauma | 15 | 14 point | Fair | AVN |
| 6 | 26 | M | 1 | Severe | T-E type 2 | Acetabular fracture | 15 | 16 point | Good | Normal |
| 7 | 19 | M | 2 | Severe | T-E type 3 | Acetabular fracture | 13 | 14 point | Fair | AVN |
| 8 | 6 | F | 2 | Minor | T-E type 1 | Isolated | 12 | 18 point | Excellent | Normal |
| 9 | 4 | M | 3 | Minor | T-E type 1 | Sciatic | 12 | 18 point | Excellent | Normal |
| 10 | 70 | F | 3 | Minor | T-E type 1 | Isolated | 9 | 18 point | Excellent | Normal |
| 11 | 36 | F | 4 | Severe | T-E type 4 | Polytrauma | 8 | 12 point | Poor | AVN |
| 12 | 4 | F | 3 | Minor | T-E type 1 | Isolated | 8 | 18 point | Excellent | Normal |
| 13 | 36 | M | 2 | Severe | T-E type 2 | Acetabular fracture | 8 | 17 point | Good | Normal |
| 14 | 24 | F | 2 | Severe | T-E type 2 | Acetabular fracture | 7 | 16 point | Good | Normal |
| 15 | 6 | F | 2 | Severe | T-E type 1 | Femoral fracture | 7 | 18 point | Excellent | Normal |
| 16 | 29 | M | 4 | Severe | T-E type 1 | Polytrauma | 6 | 12 point | Poor | AVN |
| 17 | 57 | M | 1 | Minor | T-E type 1 | Isolated | 4 | 18 point | Excellent | Normal |
All dislocations were reduced closed and received the same post reduction management, which consists of aspiration of the hip joint, skin or skeletal traction for three weeks followed by another three weeks of non-weight bearing. In case of the dislocations associated with fractures, full weight bearing was allowed when the fractures healed.
Follow-up reviews were undertaken at every other week for 6 wk, and then at three, six and twelve months. After first year, patients were re-evaluated twice per year for 3 years, and then they invited once per year. The follow-up period averaged 11.5 (range from 4 to 20) years.
Radiological assessment: In order to assess the stability of reduction, plain radiography was repeated every other week for 6 wk. Development of AVN was assessed every 6 mo for 3 years and then once per year. AVN was defined as the appearance of subchondral sclerosis or the presence of segmental collapse. Associated fractures were considered during the follow-up visits.
Clinical assessment: Clinical outcome was evaluated according to Matta clinical evaluation system[17] that evaluates with points the pain, walking and range of hip motion. The clinical scores were classified as excellent = 18 points, good = 15-17 points, fair = 13-14 points and poor ≤ 13 points[17].
The causative trauma was classified as minor in seven cases and severe trauma in ten cases. The direction of the hip dislocations was posterior in all cases. According to the Thompson-Epstein classification system[16], 11 cases were classified as a type 1, three cases type 2, one case type 3, and two cases type 4. Six cases were classified as isolated dislocation and 11 cases were associated with other injuries (Table 1). The negligence period averaged 2.5 (ranged from 1 to 4) d.
Post-reduction aspiration of the hip joints revealed hemarthrosis in six, synovial fluid in four, and negative aspiration in seven hip joints.
The normal appearance of the femoral head compared to the contralateral side was observed in 11 patients and AVN signs were observed in six patients.
According to Matta[17] eight patients were rated as excellent, three good, three fair and three poor (Table 1). The overall rating was good and the overall score averaged 16 (ranged from 12 to 18) points. No general complication was reported, the associated fractures healed in the accepted position and the injured sciatic nerve cured.
We have noticed a relationship between the patients’ ages and severity of the trauma on one hand and the outcomes on the other hand. Five patients with an average age of 4.4 years (range from 3-6 years) had hip dislocation due to minor trauma achieved excellent outcomes as well signs of AVN were not detected during the follow-up period. Similarly, a female patient 6-years old, although had dislocation due to severe trauma, however, has an excellent result with no AVN. Conversely, the patients who developed AVN their ages averaged 33 years (range: 19 to 55 years), had exposed to severe trauma and the post-reduction aspiration of the hip joints revealed hemarthrosis.
Factors influencing outcomes of traumatic hip dislocation include reduction time, severity of trauma, patients’ ages and direction of dislocation. Although these factors have been thoroughly investigated, any of them was not assigned as the causative for the development of the AVN. Does the increased intracapsular pressure is the foremost factor?
Diagnosis of traumatic hip dislocation is easy, many authors and we likewise have noticed missed cases. Prominence of the associated injuries or insignificance of the trauma really leads to delay of the diagnosis[6,7]. Although delayed reduction has been regularly linked to incidence of AVN, definition of negligence period is not clear in the literature[1,9]. Experimentally, AVN was produced in the capital femoral epiphysis of immature dogs after increasing the intracapsular pressure for six hours and in the adult dogs for 12 h[18,19]. Consequently, dislocation is considered neglected when the reduction was not achieved before 12 h of injury. In the present study, all cases were reduced at an average 2.5 d, only 35% of the cases developed AVN (Table 1). Sapkas et al[10] have considered the reduction time is not a critical factor in the appearance of AVN.
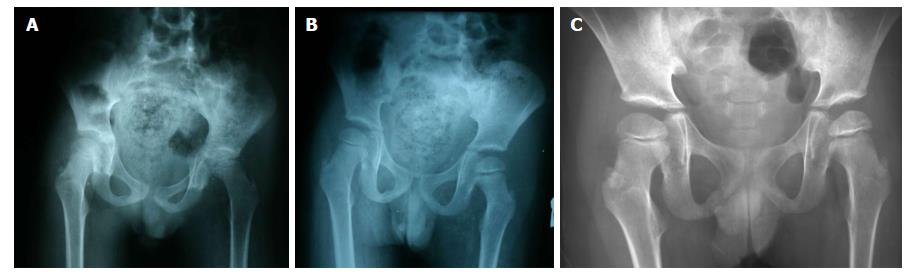
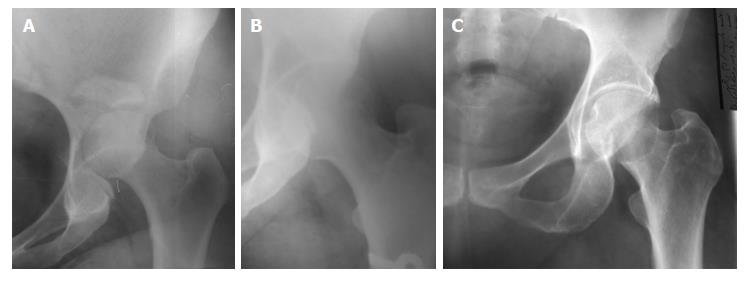
Minor trauma can dislocate the hip in children (Figure 1), likewise at any age in the presence of the biological predisposing factors[2-5]. Thus, it is not mostly associated with other injuries[6-8]. However, severe trauma at least associated with a hemarthrosis. Laorr et al[11], investigated 18 patients with traumatic hip dislocation and found hemarthrosis in all cases. This explains why many authors have linked severity of trauma to the incidence of AVN[7,10,20]. In the present study, we detected hemarthrosis in six, synovial fluid in four, and negative aspiration in seven hip joints. Additionally, the hips that were dislocated due to minor trauma have normal femoral heads, while most of those had dislocations due to severe trauma developed AVN during the follow-up period (Figures 1 and 2). However, the dislocations that associated with acetabular (Figure 3) or femoral shaft fractures have not developed AVN (cases No. 6, 13, 14 and 15 in Table 1). The associated femoral fractures, likely resulted from a substantial force sufficient for laceration of the hip capsule additionally[1]. Any of acetabular fracture or capsular laceration allowed for leakage of the hemarthrosis, and therefore, the intracapsular pressure has not increased.
The patient’s age can predict the outcomes through the severity of trauma on the one hand and the age-related changes of the femoral head circulation on the other hand. At age under 5 years, the acetabulum is primarily soft pliable cartilage as well as there is a generalized ligamentous laxity, therefore the minor trauma can dislocate the hip joint[2,6]. Additionally, it has been reported that the variations in the age-related sequelae of the traumatic hip dislocation have been in part attributed to the age-related changes in the hip circulation[2,8,12,21].
At the fourth year of age, the femoral head is supplied through a retinacular arterial system, which consists of multiple arteries. With age, the multiple small vessels of the young coalesce to a limited number of larger vessels. Thus, damage to a single blood vessel can have serious consequences[2]. Most authors suggest that the posterosuperior branch of the medial circumflex artery is the most likely site of vascular damage[10,21,22]. Nevertheless, such vessels have a more ability to accommodate the extreme posterior displacement of the femoral head[23]. This explains why many authors have reported the continuation of femoral head circulation after reduction of pure hip dislocation[8,22].
Direction of hip dislocation plays an important role in the development of AVN[8]. Generally, pure anterior dislocations have a better long-term prognosis than posterior dislocations[1,20]. In anterior dislocations, the capsule is disrupted anteriorly and inferiorly while in posterior dislocations the capsular tear either inferoposterior or directly posterior, depending on the amount of flexion present[1]. As the posterosuperior vessels is the most likely site of vascular damage[10,21,22], the posteriorly dislocated femoral head compress these vessels against the posterior acetabular rim and interrupt the femoral head circulation[22]. Position of the limb prior to reduction also plays a role in the development of AVN[13]. In posterior dislocations, the leg is flexed, adducted, and internally rotated while in anterior dislocations, the leg is externally rotated with varying amounts of flexion and abduction[1]. So, the deformity in anterior dislocation increases capacity of the hip capsule to accommodate pressure more than that in posterior dislocation[13-15]. Moreover, recognizable limb deformity in anterior dislocation renders negligence is less likely.
Hip joint is enclosed by a thick fibrous capsule[2]. Therefore, the trauma that has sufficient severity to dislocate the inherently stable joint, constantly results in hemarthrosis, which increases the intracapsular pressure to a level sufficient to tamponade of the retinacular blood vessels[2,11,12]. This was proved experimentally in two separate studies, as they produced AVN when the intracapsular pressure of the hip was increased for six or twelve hours[18,19]. Likewise, the tight repair of the hip capsule after surgical dislocation led to a drop in the perfusion of the femoral head[20,22]. Given that, the development of AVN must depend essentially upon the steadiness of interruption of blood flow[21]. Hence, the hemarthrosis that was detected at an average 13.2 d after injury will offer the circumstance sufficient for the development of avascular AVN even after prompt reduction[11,12].
Post reduction management plays a role in the development of AVN. Most surgeons recommend a period of traction until the patient’s initial pain has subsided. However, this position increases the intracapsular pressure[13-15,20,21]. Therefore, the best recommendations for post-reduction treatment are avoidance of strict immobilization and allow full weight bearing once the patient can control his leg in space[1,11-13]. Aspiration of the hip, if it has hemarthrosis, should be repeated during the first day and in the next days as long as the joint effusion persists.
The present study has many limitations: In part, the included data were retrospectively collected from a heterogeneous group of patients and in another part, lacked the use of the diagnostic tools as measuring of intracapsular pressure and MRI. However, heterogeneity provided an opportunity for studying of different age groups and different types of trauma, albeit in a small number of patients. Availability of patients for a considerable period of follow-up offered the data that warranted the building of the logical opinion.
We believe that the factors as hemarthrosis, the position of the limb during the pre-reduction period particularly in posterior dislocation and traction in post-reduction period can increase the intracapsular pressure to a level sufficient for occlusion of intracapsular blood vessels. Delayed reduction accentuates influence of increased intracapsular pressure in favour of the development of AVN.
In February 1993, a 3-years old boy present with the secondary inability to walk after fall during running since four days. Hip dislocation was detected and reduced immediately. In June 1995, a male 33-years-old had present with multiple traumas due to a motor car accident and a hip dislocation that was missed for three days. By the sixth-month post reduction, the second patient developed avascular necrosis (AVN). In the same week, I called the first patient for follow-up and radiological examination that revealed normal hips. At this moment I wondered, why the second patient developed AVN despite the delayed reduction was the common denominator? In subsequent years I started a study titled “Fixation of intracapsular femoral neck fractures: Effect of trans-osseous capsular decompression” (published). Therefore, the importance of the intracapsular pressure has resurfaced. Again I wondered, what the relationship between the age and the severity of the trauma regarding the hip dislocation? As well, what the influence of hemarthrosis on the development of AVN?
This study was conducted for answering of the inquiries that can be summarized in, “when we expect the development of the AVN after hip dislocation and how to avoid the predisposing factors”.
The objective of this study was the detection of the factor(s) that can accentuate hazardous of delayed reduction. We assumed increased intracapsular pressure is the concerned factor. Realizing this hypothesis will open the way for avoidance the complications resulted from hip joint effusion either due to trauma or disease.
This is an observational retrospective study depend on the analysis of patients records and reviewing of the literature in realizing of its objectives.
We have noticed a relationship between the patients’ ages and severity of the trauma regarding the incidence of the hip dislocation, as well the severity of trauma and development of AVN.
Increased intracapsular pressure can be a result of the combined effect of hip dislocation and traction of the limb in the post-reduction period. Complications of hip diseases that associated with hip effusion as infections or Perthes disease can be diminished through reduction of intracapsular pressure. The prompt reduction is not enough to avoid the development of the AVN. The interferences as traction of the limb for immobilization can increase the intracapsular pressure of hip joint. Influence of the intracapsular pressure varies according to the patient’s age. I suggest a prospective study using the advanced instruments for prediction of the development of AVN. The associated acetabular fractures allowed leakage of the hemarthrosis as well fracture of femoral shaft possibly lacerated the hip capsule and in both cases, we could not detect fluid through aspiration. The recommendations for post-reduction treatment are the aspiration of the hemarthrosis, avoidance of strict immobilization and allow full weight bearing once the patient can control his leg in space.
Despite the heterogeneity of the patients, however, it provided an opportunity for studying of different age groups and different types of trauma, albeit in a small number of patients. The future research should be directed toward the reduction of the complications of the diseases that associated with increased of the intracapsular pressure. The best method for the future research is a prospective randomized controlled study.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Egypt
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Mavrogenis AF S- Editor: Cui LJ L- Editor: A E- Editor: Li D
| 1. | Tornetta P 3rd, Mostafavi HR. Hip Dislocation: Current Treatment Regimens. J Am Acad Orthop Surg. 1997;5:27-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Blasier RD, Hughes LO. Fractures and traumatic dislocations of the hip in children. Fractures in Children, 5th ed. Philadelphia, PA: Lippincott Williams and Wilkins 2001; 913-940. |
| 3. | Hermanson M, Hägglund G, Riad J, Wagner P. Head-shaft angle is a risk factor for hip displacement in children with cerebral palsy. Acta Orthop. 2015;86:229-232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Upadhyay SS, Moulton A, Burwell RG. Biological factors predisposing to traumatic posterior dislocation of the hip. A selection process in the mechanism of injury. J Bone Joint Surg Br. 1985;67:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Mirovsky Y, Fischer S, Hendel D, Halperin N. Traumatic anterior dislocation of the hip joint with fracture of the acetabulum: a case report. J Trauma. 1988;28:1597-1599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Zrig M, Mnif H, Koubaa M, Abid A. Traumatic hip dislocation in children. Acta Orthop Belg. 2009;75:328-333. [PubMed] |
| 7. | Offierski CM. Traumatic dislocation of the hip in children. J Bone Joint Surg Br. 1981;63-B:194-197. [PubMed] |
| 8. | Durakbaşa O, Okan N, Canbora K, Görgeç M. [Factors affecting the results of treatment in traumatic dislocation of the hip]. Acta Orthop Traumatol Turc. 2005;39:133-141. [PubMed] |
| 9. | Hougaard K, Thomsen PB. Traumatic posterior dislocation of the hip--prognostic factors influencing the incidence of avascular necrosis of the femoral head. Arch Orthop Trauma Surg. 1986;106:32-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 108] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Sapkas G, Pantazopoulos T, Karanikas E, Hartofilakidis-Garofalidis G. Effect of hip dislocation on the blood supply to the femoral head. An experimental study in rabbits. Acta Orthop Scand. 1983;54:204-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Laorr A, Greenspan A, Anderson MW, Moehring HD, McKinley T. Traumatic hip dislocation: early MRI findings. Skeletal Radiol. 1995;24:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 51] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Rieger H, Pennig D, Klein W, Grünert J. Traumatic dislocation of the hip in young children. Arch Orthop Trauma Surg. 1991;110:114-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Massoud EIE. Fixation of intracapsular femoral neck fractures: Effect of trans-osseous capsular decompression. Dicle Med J. 2010;37:89-96 [DOI 10.5798/diclemedj.09.09.2010.02]. |
| 14. | Soto-Hall R, Johnson LH, Johnson RA. Variations in the intra-articular pressure of the hip joint in injury and disease, a probable factor in avascular necrosis. J Bone Joint Surg Am. 1964;46:509-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 61] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Strömqvist B, Nilsson LT, Egund N, Thorngren KG, Wingstrand H. Intracapsular pressures in undisplaced fractures of the femoral neck. J Bone Joint Surg Br. 1988;70:192-194. [PubMed] |
| 16. | Thompson VP, Epstein HC. Traumatic dislocation of the hip; a survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg Am. 1951;33-A:746-778; passim. [PubMed] |
| 17. | Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632-1645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Henard DC, Calandruccio RA. Experimental production of roentgenographic and histological changes in the capital femoral epiphysis following abduction, extension, and internal rotation of the hip. Surg Forum. 1971;22:442-444. [PubMed] |
| 19. | Woodhouse CF. Dynamic influences of vascular occlusion affecting the development of avascular necrosis of the femoral head. Clin Orthop Relat Res. 1964;32:119-129. [PubMed] |
| 20. | Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 633] [Cited by in RCA: 651] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 21. | Tucker FR. Arterial supply to the femoral head and its clinical importance. J Bone Joint Surg Br. 1949;31B:82-93. [PubMed] |
| 22. | Nötzli HP, Siebenrock KA, Hempfing A, Ramseier LE, Ganz R. Perfusion of the femoral head during surgical dislocation of the hip. Monitoring by laser Doppler flowmetry. J Bone Joint Surg Br. 2002;84:300-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 100] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Grose AW, Gardner MJ, Sussmann PS, Helfet DL, Lorich DG. The surgical anatomy of the blood supply to the femoral head: description of the anastomosis between the medial femoral circumflex and inferior gluteal arteries at the hip. J Bone Joint Surg Br. 2008;90:1298-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |