Peer-review started: September 24, 2017
First decision: November 6, 2017
Revised: January 6, 2018
Accepted: January 23, 2018
Article in press: January 23, 2018
Published online: February 18, 2018
Processing time: 39 Days and 20 Hours
To determine which of the common used incision techniques has the lowest chance of iatrogenic damage to the nerves which at risk are the superficial branch of the radial nerve (SBRN) and the Lateral Antebrachial Cutaneous Nerve (LABCN).
Twenty embalmed arms were dissected and the course of the SBRN and the LABCN in each individual arm was marked and the distance between the two branches of the SBRN at the location of the First Extensor Compartment (FEC) was measured. This data was used as input in a visualization tool called Computer Assisted Anatomy Mapping (CASAM) to map the course of the nerves in each individual arm.
This image visualizes that in 90% of the arms, one branch of the SBRN crosses the FEC and one branch runs volar to the compartment. The distance between the two branches was 7.8 mm at the beginning of the FEC and 10.2 mm at the end. Finally the angle of incision at which the chance of damage to the nerves is lowest, is 19.4 degrees volar to the radius.
CASAM shows the complexity of the course of the SBRN over the FEC. None of the four widely used incision techniques has a significantly lower chance of iatrogenic nerve damage. Surgical skills are paramount to prevent iatrogenic nerve damage.
Core tip: Although many incision techniques can be found in literature no consensus on the best incision technique has been established. The study shows a large variation in the course of the superficial branch of the radial nerve over the first extensor compartment. However no complete safe zone can be defined. The choice of incision remains surgeons’ preference and surgical skills are paramount to prevent iatrogenic nerve damage.
- Citation: Poublon AR, Kleinrensink GJ, Kerver AL, Coert JH, Walbeehm ET. Optimal surgical approach for the treatment of Quervains disease: A surgical-anatomical study. World J Orthop 2018; 9(2): 7-13
- URL: https://www.wjgnet.com/2218-5836/full/v9/i2/7.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i2.7
A study regarding de Quervains disease (QD) performed in the UK showed a prevalence of 0.5% in men and 1.3% in women[1]. The study also showed a higher prevalence in workers and black people. Since its first description in 1895 by Fritz de Quervain, various treatment options have been described, varying from non-invasive techniques, such as splinting[2-7], to more invasive techniques such as injection[3,8-13] or even an operation one very debilitating complication after surgery for de Quervains disease, is nerve damage.
In previous studies four incision types have been suggested when applying surgical treatment: Transverse, longitudinal, lazy “s” or even specific angle technique. The transverse incision is designed to follow the lines of Langer and provide a superior cosmetic result[14,15]. The skin is incised transversely for 0.5 to 1 cm and the underlying tissue is bluntly dissected down to the extensor retinaculum overlying the first extensor compartment. The retinaculum is opened longitudinally and the first extensor compartment is released.
The longitudinal incision has been emphasized as being the safest incision[16,17]. The skin is incised longitudinally for 1.5 to 2 cm over the first extensor compartment and the underlying tissue is bluntly dissected down to the extensor retinaculum. The extensor retinaculum is opened longitudinally and the first extensor compartment is released.
The “lazy S” incision has been described[18]. The skin is incised with a stretched S over a length of 2 cm over the first extensor compartment. As with the other techniques, the underlying tissue is bluntly dissected down to the extensor retinaculum and the extensor retinaculum is opened longitudinally to release the first extensor compartment.
Another technique, is an incision under a specific angle as described[19]. Firstly a line is drawn down the mid-shaft of the first metacarpal and secondly a line is drawn perpendicular to the first line one finger width proximal to the base of the first metacarpal. From the intersection of these two lines, a 1-1.5 cm long incision is directed proximally and directed towards the ulna at a 30 to 45-degree angle.
However until now no consensus has been established on a “golden standard” for the incision type used for surgical treatment of the de Quervains Disease. The ideal incision should provide the best exposure with minimal scar tissue formation, a low recurrence rate and a minimal chance of iatrogenic damage to anatomical structures, i.e. the superficial nerves.
The structures most at risk in case of surgical treatment of QD are the SBRN and the Lateral Antebrachial Cutaneous Nerve (LABCN). The course of these nerves has been described in many previous studies (ref anatomy). The course of these nerves makes them very susceptible to iatrogenic damage. Some form of Superficial nerve damage has been estimated to occur in 0.5% to 30% of release[15,20-25].
As postulated in an earlier study[26], iatrogenic nerve damage to these nerves can lead do debilitating neuropathic pain symptoms[27].
The aim of this study is to identify, out of the four operative techniques described above, the technique with the lowest risk of iatrogenic damage to the nerve.
By using a new anatomical tool called Computer Assisted Anatomy Mapping (CASAM) it was possible to visualize statistics on the course of the nerves most at risk, such as the SBRN and LABCN.
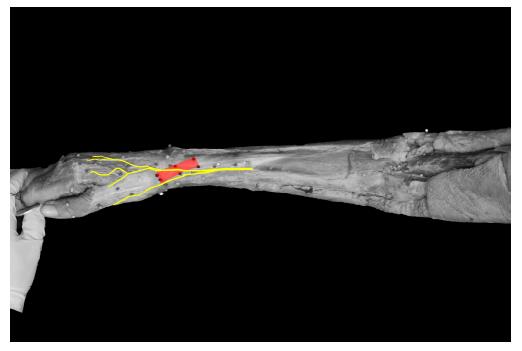
CASAM is a tool that made it possible to visually map the course of the two branches of the SBRN and the course of the LABCN in each of the twenty arms that were dissected. By enlarging and/or reducing the size of all twenty individual visual images to the size of the average length of all twenty arms and then layering all individual images over each other, a visual image was created that represents the jointly course of the nerves in the average arm[28,29] (see the CASAM paragraph below).
This image, created by using CASAM, shows the complexity of the course and density of the nerves at risk in the operative area and thus providing a tool to evaluate the four incision techniques when operating.
Twenty embalmed arms were dissected and the course of the SBRN and LABCN were identified and marked using colored pins. All arms [9 male, 11 female; mean age 79.35 (range 61-90); 15 Right, 5 Left] were embalmed using the anubifix embalming solution. The dissections were then performed under a magnifying loupe with a 2.5 times magnification.
A standardized dissection technique was used. An incision was made from approximately 10 cm above the elbow down to the Metacarpo phalangeal (MCP) joint. At the proximal and distal end of the first incision, two perpendicular incisions were placed, by making these incisions a skin flap was created which could be removed laterally and medially. The Musculocutaneous Nerve was identified under the biceps and the LABCN was followed down to the MCP. At the distal 1/3 of the arm, the brachioradialis muscle was identified and bluntly dissected from the underlying tissue. The SBRN was found running under to the brachioradialis muscle (BR). Once the SBRN was found deep to the BR its course was followed to the muscle tendon transition from where the SBRN runs a superficial course. The SBRN was dissected distally to the Metacarpal joint and the nerve was identified using colored pins. After the SBRN was dissected down to the MCP the first extensor compartment was identified and the contour was marked using colored pins. Each arm was photographed with a Nikon D 60 with Sigma 50 mm 1:2.8 DG MACRO lens using a standardized setup[29]. The camera was positioned perpendicular to the specimen at a fixed distance and the arms were placed in specially designed clamps to ensure standard alignment.
The width and length of the first extensor compartment was measured using digital calipers. Also, the distance between the first two branches of the SBRN was measured at 5 mm intervals. Finally, the angle was measured in which an incision would pose a minimal threat to the SBRN.
Since the dissected arms vary in size, making comparisons is difficult. By using CASAM it is possible to compare digital images of all dissected arm directly by warping them to an average dimension.
CASAM is based on the fact that the bony landmarks, such as Lister’s tuberculum, are relatively constant in the same position in every arm. These are called “bony landmarks” (BL). From “bony landmarks” so called “shape defining landmarks” (SDL) were calculated, to mark the outline of each arm, by dividing the space between two BL’s into equal parts. The BL’s and SDL’s were used to define the shape of each arm and average locations for these landmarks were computed, thus creating an “average” arm. All arms were then warped to the dimensions of the “average” arm making is possible to compare all the arms directly. The “scaled” course of the SBRN and the LABCN of all individual arms could then be compared directly. In the near future, the data collected in the anatomical study will be stored in a database which is made accessible via the internet. Then, a digital picture of a patient can be uploaded and warped to the “average”arm of the CASAM database to predict the course of the SBRN making more precise, individual preoperative planning possible.
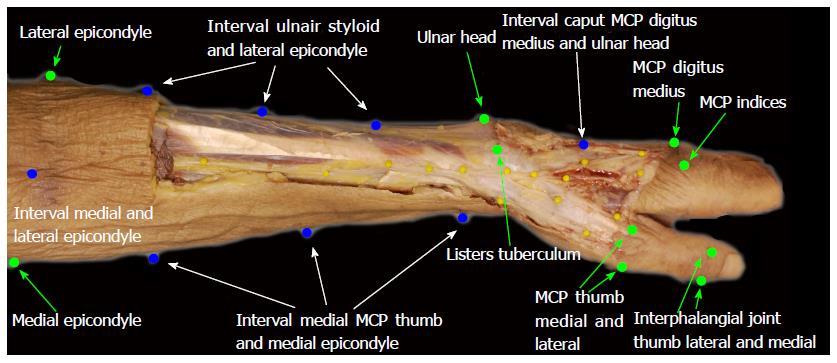
The “bony landmarks” and “shape defining landmarks”used in this study can be found in Figure 1 (green marks and blue marks). An image is then created of each arm with average dimensions of all specimen. This shows the average course of the SBRN.
The mean distance between a line through the lateral and medial epicondyle and Lister’s tuberculum, was 239.15 mm (range 209-281 mm), this distance was used as the reference length of the arm.
The course of the SBRN and LABCN was traced using Photoshop CS4, furthermore the shape of the first extensor compartment was also traced in photoshop. These photoshop layers could then be compiled into one picture for further analysis.
The four incision types could then be superimposed on the database of nerves and the proximity to nerve fibers could be assessed.
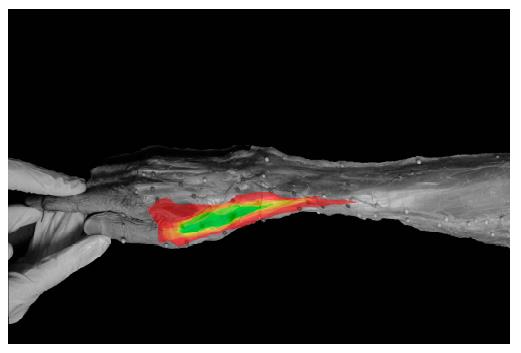
The area between the first and second branch of the SBRN was defined and subsequently ‘filled’ with a color with 5% opacity. By compiling all 20 arms, an area could be defined in which the nerve was present in 5% of all cases and subsequently an area can be identified in which the nerve is present in 10% of cases etc. In this fashion a colored gradient map could be produced showing the 0 to 100% safe zone.
The first extensor compartment can be found at a distance of 8 mm proximal to Lister’s tuberculum and has a mean length of 26.6 mm (SD 5.3) and a mean width of 8.2 mm (SD 1.1). The mean angle between the first extensor compartment and the radius was 19.4° (SD 4.4). In all twenty specimens one or two branches of the SBRN ran across the first extensor compartment. The first branching of the SBRN was found 43.8 mm (SD 18.6) proximal to Lister’s tuberculum.
CASAM shows that in 90% of all cases one branch of the SBRN (SR 2) runs across the first extensor compartment in a longitudinal direction. Also, a second branch (SR 1) runs volar to the first extensor compartment (Figure 2). In the present 20 specimen, no complete safe zone (a zone in which no nerve fibers are present) could be identified near the first extensor compartment. However, the CASAM images (Figure 2) show that the direction of the SBRN over the first extensor compartment is at an angle of 19.4 degrees volar to the radius. Also one of the images created in CASAM shows a very small safe zone in which none of the nerves in the 20 specimen are present over the FEC (Figure 3).
The distance between the two branches of the SBRN crossing the first extensor compartment is 7.8 mm (SD 3.6) at the beginning of the first extensor compartment. 10.2 mm (SD 2.7) halfway down the first extensor compartment and 12.6mm (SD 2.7) at the end of the first extensor compartment (Figure 4). The branch running through the first extensor compartment divides in two more branches crossing the path of longitudinal path. The mean distance between the first branching point and the second is 43.5mm (SD 19.17), e.g., the maximum length of a longitudinal incision.
During dissection it was not possible to follow the LABCN over the first extensor compartment because the nerve runs mostly intradermally. Furthermore, the course of the LABCN varies tremendously and no correlations between the courses of the LABCN could be found (Figure 5). No recommendation to prevent damage to the LABCN during Quervains disease surgery could be made. Therefore, the LABCN was left out. However as seen in earlier studies[26] the close relation between the LABCN and SBRN could be a major contributor to the cause of neuropathic pain in the distal wrist.
Since the description of the first surgical treatment of Quervains disease, many surgeons have tried to perfect the operating technique and hence tried to minimize the complications. This study focusses on aspects of the incision. However, this treatment modality too has its complications. Recurrent tendovaginosis is a complication which occurs and often requires a second operation[30,31]. Also (iatrogenic) nerve damage is frequently seen, varying from neurapraxia to total transection of the nerve, are reported in literature[20,22-25].
The surgical treatment of Quervains disease is the treatment of choice after conservative measures have failed. To operate safely in the area of the dorso-radial part of the distal radius and the first metacarpus immediately introduces the problem of crossing and intertwining superficial branches of the radial nerve and the lateral cutaneous nerves (branches of the musculocutaneous nerve).
Three types of incisions are used to operate in this region; the transverse, the longitudinal and the “lazy S” type incision. Each of which has its advantages and disadvantages and no best practice (‘golden standard’) could be found in literature. In the present study an attempt is made to make an inventory of the course of the surgically relevant nerves related to the four incision types. Data was visualized using CASAM to give the surgeon concise information that allows him to make a choice between the four incisions.
The transverse technique offers a good exposure while keeping the scar small and provides the best esthetic result[14,15]. Also because the skin incision is perpendicular to the first extensor compartment, contraction of scar tissue is less likely to cause compression of the first extensor compartment and thus is less likely to cause a recurrence of the symptoms of Quervains disease. However, the transverse direction of the skin incision implicates a high risk of iatrogenic nerve damage demonstrated by the images provided by CASAM (Figure 5). Furthermore, the distance between the two branches of the SBRN is 11.4 mm (0-26.3), therefore a transverse incision not only increases risk of injury to one branch but to the second branch as well.
The longitudinal techniques offers more exposure than a transverse incision[16,17,32] with a lower chance of iatrogenic nerve damage[33]. However this technique offers a suboptimal cosmetic result and because the scar is directly over the first extensor compartment the retraction of scar tissue could cause compression of the first extensor compartment and recurrence of the symptoms of Quervains disease. The average length for the incision placed between the first two branches of the SBRN is 43.5 mm (SD 18.2). The nerve remains at risk due to its location over the first extensor compartment.
The “lazy S” technique has both advantages and disadvantages. The incision offers a good exposure and less chance of iatrogenic damage than the transverse incision[17,18]. However the scar as a result of this incision is not as cosmetic as the transverse incision and the incision has a greater chance of iatrogenic damage to the nerves than the longitudinal incision.
This technique offers a good exposure and minimizes the chance of iatrogenic damage to the nerve. It also offers a relatively cosmetically acceptable scar. However the determination of the angle of the incision takes time and is labor-intensive.
The technique described by[19] suggests a relatively acute angle to the radius which introduces a relatively high risk of damage to the SBRN. The present study shows that this risk can be significantly reduced by using a less acute angle.
The present study was performed using embalmed specimen which always means that the measurements cannot be extrapolated directly to the normal situation. However, since this concerns only relative measurements, the conclusions can be seen as representative. Furthermore by using Anubifix™ the shrinkage of tissue due to embalming is minimized and comparable to the fresh frozen specimen, the next best situation when compared with the in vivo situation.
Two- dimensional pictures are used in CASAM to warp the arms, but when operating the arm is a three-dimensional object. However, by taking the pictures in the same plane as the surgeon would use to make the incision, the third dimension is less relevant.
By using CASAM it was possible to virtually compare the incision techniques on the same arms. All techniques described above for the treatment of Quervains disease have their own advantages and disadvantages. The choice of which technique to use, depends on the priorities set by the surgeon. The main goal of this study was to identify the technique where iatrogenic damage to the SBRN is minimal. The conclusion that can be taken from the data is that despite the technique used, is that the retinaculum of the first dorsal compartment needs to be exposed by careful blunt dissection and divided under direct vision, so that the surgeon can see that the superficial nerves are not damaged. For beginning surgeons the longitudinal offers good exposure and less chance of iatrogenic nerve damage.
Surgery is a widely applied as a treatment for the de Quervains Disease (QD). However, in 0.5 to 30% of cases, damage to the neurological structures have been reported this study was performed to try and provide a better understanding of the anatomy of the forearm to be able to decrease iatrogenic damage to the nerves of the forearm.
In this study the goal was to fins the optimal incision technique for the first dorsal compartment release for the Quervains disease. Up till now 4 main incision techniques have been described and no golden standard has been established. By using a new visualization technique the goal was to identify the best technique in order to prevent iatrogenic nerve damage during the first extensor compartment release procedure.
The goal of this study is to determine which of the common used incision techniques has the lowest chance of iatrogenic damage to the nerves. The nerves at risk are the superficial branch of the Radial Nerve (SBRN) and the Lateral Antebrachial Cutaneous Nerve (LABCN).
20 anubifix embalmed arms were dissected in a standardized way. Then the outline of the arm was marked and the arm was photographed in order to process it in the CASAM system. By using this system all arms could be rescaled to the dimensions of the average of the 20 embalmed arms. This ensures that the 20 nerve courses could be compared directly. Besides using CASAM the distance between the two branches of the SBRN running over de First Extensor Compartment (FEC) was measured.
The image created in CASAM showed that in 90% of the arms, one branch of the SBRN crosses the FEC and one branch runs volar to the compartment. The distance between the two branches was 7.8 mm at the beginning of the FEC and 10.2 mm at the end. Finally the angle of incision at which the chance of damage to the nerves is lowest, is 19.4 degrees volar to the radius.
The study shows a large variation in the course of the superficial branch of the radial nerve over the first extensor compartment. However no complete safe zone can be defined. The choice of incision remains surgeons’ preference and surgical skills are paramount to prevent iatrogenic nerve damage. The pre-study hypothesis was that there was a safe zone in which an incision for the Quervains disease could be made without chance of iatrogenic damage to the superficial branch of the radial nerve. This however was found not to be the case.
Although many incision techniques can be found in literature no consensus on the best incision technique has been established. The study shows a large variation in the course of the superficial branch of the radial nerve over the first extensor compartment. However no complete safe zone can be defined. The choice of incision remains surgeons’ preference and surgical skills are paramount to prevent iatrogenic nerve damage. A randomized control trail comparing the incision techniques and their outcome could provide more evidence for the best possible incision technique in the future.
The authors would especially like to thank Y. Steinvoort and B.J. Kompanje for all the help in providing room for dissection and all specimens.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Netherlands
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Angoules A S- Editor: Cui LJ L- Editor: A E- Editor: Li RF
| 1. | Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum. 2004;51:642-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 367] [Cited by in RCA: 396] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 2. | Mehdinasab SA, Alemohammad SA. Methylprednisolone acetate injection plus casting versus casting alone for the treatment of de Quervain’s tenosynovitis. Arch Iran Med. 2010;13:270-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 3. | Richie CA 3rd, Briner WW Jr. Corticosteroid injection for treatment of de Quervain’s tenosynovitis: a pooled quantitative literature evaluation. J Am Board Fam Pract. 2003;16:102-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 90] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Moore JS. De Quervain’s tenosynovitis. Stenosing tenosynovitis of the first dorsal compartment. J Occup Environ Med. 1997;39:990-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 70] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Avci S, Yilmaz C, Sayli U. Comparison of nonsurgical treatment measures for de Quervain’s disease of pregnancy and lactation. J Hand Surg Am. 2002;27:322-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 70] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Menendez ME, Thornton E, Kent S, Kalajian T, Ring D. A prospective randomized clinical trial of prescription of full-time versus as-desired splint wear for de Quervain tendinopathy. Int Orthop. 2015;39:1563-1569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Lane LB, Boretz RS, Stuchin SA. Treatment of de Quervain’s disease:role of conservative management. J Hand Surg Br. 2001;26:258-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 70] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Ilyas AM. Nonsurgical treatment for de Quervain’s tenosynovitis. J Hand Surg Am. 2009;34:928-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Peters-Veluthamaningal C, van der Windt DA, Winters JC, Meyboom-de Jong B. Corticosteroid injection for de Quervain’s tenosynovitis. Cochrane Database Syst Rev. 2009;Jul 8:CD005616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Peters-Veluthamaningal C, Winters JC, Groenier KH, Meyboom-DeJong B. Randomised controlled trial of local corticosteroid injections for de Quervain’s tenosynovitis in general practice. BMC Musculoskelet Disord. 2009;10:131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Earp BE, Han CH, Floyd WE, Rozental TD, Blazar PE. De Quervain tendinopathy: survivorship and prognostic indicators of recurrence following a single corticosteroid injection. J Hand Surg Am. 2015;40:1161-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Mardani-Kivi M, Karimi Mobarakeh M, Bahrami F, Hashemi-Motlagh K, Saheb-Ekhtiari K, Akhoondzadeh N. Corticosteroid injection with or without thumb spica cast for de Quervain tenosynovitis. J Hand Surg Am. 2014;39:37-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Rowland P, Phelan N, Gardiner S, Linton KN, Galvin R. The Effectiveness of Corticosteroid Injection for De Quervain’s Stenosing Tenosynovitis (DQST): A Systematic Review and Meta-Analysis. Open Orthop J. 2015;9:437-444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Altay MA, Erturk C, Isikan UE. De Quervain’s disease treatment using partial resection of the extensor retinaculum: A short-term results survey. Orthop Traumatol Surg Res. 2011;97:489-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Suresh SS, Zaki H. De quervain disease: Ibri technique to avoid superficial radial nerve injury. Tech Hand Up Extrem Surg. 2009;13:113-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Gundes H, Tosun B. Longitudinal incision in surgical release of De Quervain disease. Tech Hand Up Extrem Surg. 2005;9:149-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Bruner JM. Optimum skin incisions for the surgical relief of stenosing tenosynovitis in the hand. Plast Reconstr Surg. 1966;38:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Bouras Y, El Andaloussi Y, Zaouari T, Touil N, Fnini S, Chikhaoui N, Largab A. Surgical treatment in De Quervain’s tenosynovitis. About 20 cases. Ann Chir Plast Esthet. 2010;55:42-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Ostric SA, Martin WJ, Derman GH. Intersecting the intersection: a reliable incision for the treatment of de Quervain’s and second dorsal compartment tenosynovitis. Plast Reconstr Surg. 2007;119:2341-2342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Mellor SJ, Ferris BD. Complications of a simple procedure: de Quervain’s disease revisited. Int J Clin Pract. 2000;54:76-77. [PubMed] |
| 21. | Scheller A, Schuh R, Hönle W, Schuh A. Long-term results of surgical release of de Quervain’s stenosing tenosynovitis. Int Orthop. 2009;33:1301-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (1)] |
| 22. | Arons MS. de Quervain’s release in working women: a report of failures, complications, and associated diagnoses. J Hand Surg Am. 1987;12:540-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 42] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Rask MR. Superficial radial neuritis and De Quervain’s disease. Report of three cases. Clin Orthop Relat Res. 1978;176-182. [PubMed] |
| 24. | Braidwood AS. Superficial radial neuropathy. J Bone Joint Surg Br. 1975;57:380-383. [PubMed] |
| 25. | Kang HJ, Hahn SB, Kim SH, Choi YR. Does endoscopic release of the first extensor compartment have benefits over open release in de Quervain’s disease? J Plast Reconstr Aesthet Surg. 2011;64:1306-1311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Poublon AR, Walbeehm ET, Duraku LS, Eilers PH, Kerver AL, Kleinrensink GJ, Coert JH. The anatomical relationship of the superficial radial nerve and the lateral antebrachial cutaneous nerve: A possible factor in persistent neuropathic pain. J Plast Reconstr Aesthet Surg. 2015;68:237-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Stokvis A, van der Avoort DJ, van Neck JW, Hovius SE, Coert JH. Surgical management of neuroma pain: a prospective follow-up study. Pain. 2010;151:862-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 93] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 28. | Kerver AL, Carati L, Eilers PH, Langezaal AC, Kleinrensink GJ, Walbeehm ET. An anatomical study of the ECRL and ECRB: feasibility of developing a preoperative test for evaluating the strength of the individual wrist extensors. J Plast Reconstr Aesthet Surg. 2013;66:543-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Kerver AL, van der Ham AC, Theeuwes HP, Eilers PH, Poublon AR, Kerver AJ, Kleinrensink GJ. The surgical anatomy of the small saphenous vein and adjacent nerves in relation to endovenous thermal ablation. J Vasc Surg. 2012;56:181-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | Alegado RB, Meals RA. An unusual complication following surgical treatment of deQuervain’s disease. J Hand Surg Am. 1979;4:185-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 32] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Picart P. Symposium on the examination of equilibration function. Functional exploration of the vestibular apparatus. J Fr Otorhinolaryngol Audiophonol Chir Maxillofac. 1967;16:475-477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Menné T, Hjorth N. Routine patch testing with paraben esters. Contact Dermatitis. 1988;19:189-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Kumar K. Outcome of longitudinal versus transverse incision in de Quervain’s disease and its implications in Indian population. Musculoskelet Surg. 2016;100:49-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |