Published online Nov 18, 2018. doi: 10.5312/wjo.v9.i11.245
Peer-review started: July 12, 2018
First decision: August 2, 2018
Revised: August 7, 2018
Accepted: October 10, 2018
Article in press: October 10, 2018
Published online: November 18, 2018
Processing time: 126 Days and 18.4 Hours
Posterior instability of the shoulder is a rare condition and represents about 10% of shoulder instability. It has become more frequently recognized in the last year, even though it is more difficult to diagnose than anterior shoulder instability. As this form of shoulder pathology is somewhat rare, biomechanical knowledge is limited. The purpose of our study was to perform an extensive literature search, including PubMed and Medline, and to give an overview of the current knowledge on the biomechanics of posterior shoulder instability. The PubMed/Medline databases were utilized, and all articles related to posterior shoulder instability and biomechanics were included to form a comprehensive compilation of current knowledge. A total of 93 articles were deemed relevant according to our inclusion and exclusion criteria. As expected with any newly acknowledged pathology, biomechanical studies on posterior shoulder instability remain limited in the literature. Current biomechanical models are performed in a static manner, which limits their translation for explaining a dynamic pathology. Newer models should incorporate dynamic stabilization of both the rotator cuff and scapulothoracic joint. There is a current lack of knowledge with regards to the pathomechanism of posterior shoulder instability, with no consensus on appropriate treatment regimens. Further investigation is therefore required at both basic science and clinical levels.
Core tip: Posterior shoulder instability is an infrequent type of injury, and there is limited discussion of this topic within the literature. Other authors have acknowledged the current paucity of papers on this topic. To our knowledge, no comparable literature review has been performed showing the interactions of the individual shoulder parts, including the osseous structures, capsule, labrum, ligaments and muscles[1]. This article aspires to help develop new protocols to investigate shoulder instability and inform clinicians about the importance of this topic in daily practice.
- Citation: Bäcker HC, Galle SE, Maniglio M, Rosenwasser MP. Biomechanics of posterior shoulder instability - current knowledge and literature review. World J Orthop 2018; 9(11): 245-254
- URL: https://www.wjgnet.com/2218-5836/full/v9/i11/245.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i11.245
The shoulder joint is the least congruent joint in the human body and thus has a tremendous potential range of motion with daily activities. These movements are a well-balanced and complex interplay between the osseous structures (scapula, humeral head and clavicle) and the surrounding soft tissue, consisting of shoulder capsule, ligamentous, labral and muscular stabilizers. Dysfunction of one or more of these components through injury, degeneration or congenital abnormalities may lead to shoulder instability with concomitant pain and dysfunction. Anterior laxity or dislocation occurs more commonly than the posterior equivalent and is thus more discussed in the literature. However, posterior instability is an equally important cause of patients pain and loss of shoulder function.
The first reported case of posterior shoulder instability was published by White et al in 1741[2], followed by a case study in 1839[3] and a clinical case series in 1855[4]. A variety of pathologies have been described regarding posterior shoulder instability, such as atraumatic lesions in ligamentous laxity, repetitive microtrauma (especially in overhead-throwing athletes or the active duty military population) and traumatic posterior luxation[5,6]. In repetitive microtrauma, shearing forces may cause a loss of chondrolabral containment (e.g., frank labral tear)[7,8].
Classifications for recurrent posterior subluxation have been established according its anatomical and biomechanical properties. It can be distinguished between volitional (ability to subluxate the shoulder using abnormal patterns of muscular activity), dysplastic (due to glenoid retroversion or humeral head retrotorsion) and acquired posterior shoulder dislocation (caused by soft tissue deficiency, bony deficiency or scapula-thoracic dysfunction)[5,9].
A comprehensive literature search was conducted using PubMed/MEDLINE databases (US National Library of Medicine, National Institutes of Health) for shoulder instability and biomechanics/anatomy of the shoulder between 1957 and 2017. The search terms were intentionally broad to maximize capture of the relevant literature. The following keywords were used: “posterior shoulder instability” (n = 1026), “shoulder biomechanics” (n = 1389) and “posterior shoulder instability anatomy” (n = 295). Articles in English, German and French were included. All papers that both evaluated the biomechanics on posterior shoulder instability as well as described the anatomy in patients who suffered from posterior shoulder instability were included. Exclusion criteria included duplicate results, non-relevant articles that did not involve posterior shoulder instability or biomechanical studies, and letters to the editors or comments.
In total, 2710 abstracts were reviewed, of which 40 articles were duplicates and further 2542 did not investigate shoulder instability or the biomechanics of the shoulder complex. One hundred-twenty-eight full text articles were reviewed, of which 35 studies were excluded as these ones did not meet inclusion criteria. Finally, leaving 93 studies for our review. These included papers describing the biomechanics of anterior and posterior shoulder instability), the anatomy of the shoulder complex, as well as the clinical aspects.
The incidence of posterior shoulder instability is between 2%-5% of all shoulder dislocations[10]. According to the literature, it may be under- or mis-diagnosed due to the lack of both awareness and experience of treating physicians. A significant proportion (62.5%) of patients who failed surgery and suffered from ongoing instability were diagnosed with unidirectional, posterior shoulder instability. Those patients demonstrated signs of inferior or multi-directional instability prior to revision surgery, which may be related to the capsular laxity. This appears to be an underestimation - 75% of these patients did not show labral tear, yet would have required more aggressive stabilization[11].
In the beginning of the investigation, the mechanism was simply believed to be the counterpart to anterior shoulder instability[12-14]. Later on, this paradigm was questioned by several researchers, who described the posterior shoulder instability as a unique injury condition[15-17].
Generally, posterior shoulder dislocation has been described in the setting of 90° forward elevation, adduction and internal rotation of the humerus[17-19]. Assumingly, the humerus then dislocates either posteriorly through rupture of the posterior band of the inferior glenohumeral ligament (IGHL) or posterior inferiorly through rupture of the whole posterior IGHL[20]. Unfortunately, the exact biomechanical mechanism of posterior shoulder instability is not well understood or described to date.
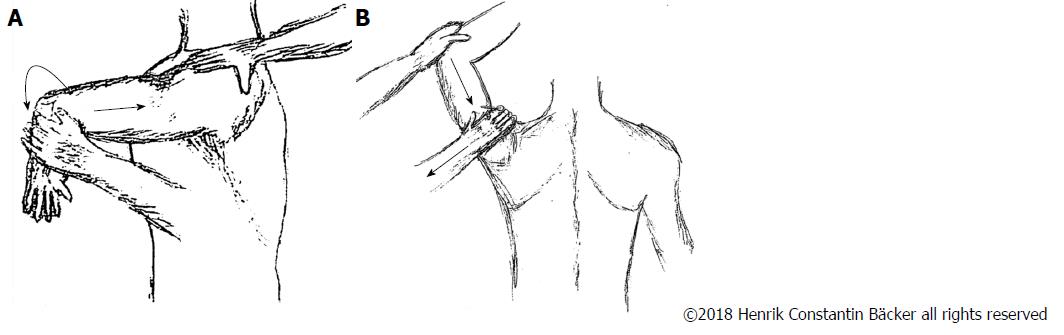
Posterior shoulder dislocation patients present with generalized symptoms about the shoulder and commonly include an intense discomfort with inability to mobilize the shoulder joint. This may be related to excessive stretching of the muscles or the joint capsule during the dislocation itself[21]. For clinical examination, the Kim test shows the highest sensitivity of 80% and specificity of 90%. Further examinations like the Jerk test, posterior apprehension test and stress test are useful to estimate the stability and dislocation tendency. The Jerk test is the most reliable diagnostic examination, however may only be pathologic in 4 of 50 patients suffering from posterior shoulder instability[22]. When performing the anterior apprehension test, patients may feel inconvenienced with a slight anterior subluxation. However, this test is neither sensitive nor specific[23]. The Kim test and Jerk test are illustrated in Figure 1.
X-ray and computed tomography: To exclude any osseous lesions and diagnose posterior shoulder dislocation, an anteroposterior, lateral and axillary radiograph should be performed. Furthermore, computed tomography (CT) may help identify injuries of the shoulder complex, such as reverse Bankart lesions or, when performing with intraarticular contrast, labral lesions. Displacement of the humeral head in relation to the glenoid, reverse Hill Sachs lesions or posterior Bankart/glenoid lesions may be pathognomonic for posterior shoulder instability but not necessarily present in all cases.
Magnetic resonance imaging: Magnetic resonance imaging (MRI) is an invaluable tool to assess soft tissue lesions about the shoulder. In patients who have suffered a posterior shoulder dislocation, a labral tear of the posterior wall or edema in the posterior humeral head is typically present. Furthermore, other pathological conditions can be excluded, such as superior, anterior posterior labral lesions or rotator cuff tears masquerading as posterior instability (Figure 2 provided by Dr. Charles M. Jobin). When comparing conventional MRI with MR arthrography, MR arthrography is superior to assess glenohumeral pathology, Perthes lesions and labral tears[24].
The rigor of MRI and CT arthrograms in posterior shoulder instability is summarized in Table 1.
| CT arthrography | MRI arthrography | |
| Sensitivity | 82%-100%[75] | 48%-89%[76,77] |
| Specificity | 96%-100%[75] | 93%[77] |
| Advantage Disadvantage | Identifying bony lesions, severity of fractures, assessing humeral and glenoid version[78] lower inter-examiner reliability[79] | Identifying the soft tissue from labrum to the rotator cuff[80], good for preoperative classification of labroligamentous injuries[81] Limited in elderly patients[80] |
| Radiation | ||
| Pathologies | Small soft tissue lesions[82] | |
| Bony lesions/ fractures (Bankart fragments, Hill-Sachs Lesion)[82,83] | Avulsion of posterior periosteum[82] | |
| Accurate in labroligamentous, cartilaginous lesions[75] | Medial displacement of the labrum (posterior labro-scapular sleeve avulsion)[84] | |
| Kim lesion - incomplete and concealed superficial tear in the posterior glenoid labrum | ||
| Glenoid rim articular divot lesion[7] | ||
| Chondral loose bodies[85] |
The glenohumeral, scapulothoracic, acromioclavicular and sternoclavicular joints can be summarized as the shoulder complex. A full range of motion, including protraction/retraction, elevation/depression, anterior/posterior tilt, internal/external and upward/downward rotation can only be achieved in combination with each individual joint[25]. The complex can be divided into osseous and soft tissue structures, enabling stability and facilitating anatomic motion.
Scapula: The scapula lies on ribs two through seven and has a triangular shape[26,27]. It is solely stabilized by soft tissue restraints through a series of bursal and muscular planes. Its position is obliquely in between the frontal and sagittal planes. Besides a slight abduction by 3°, it is located 30°-45° anterior to the coronal plane, with a slight anterior tilt between 9°-20° in the sagittal plane in relation to the vertical line of the spine[25].
Multiaxial articulation can be enabled by the scapulothoracic joint between the humerus and the thorax. When elevating the humerus above 90° in the coronal plane, the scapular mainly rotates laterally in the coronal plane with less protraction in all three planes. At 30° and 40° of humeral elevation, a significant backward tilt occurs in the sagittal plane.
The glenoid cavity, which forms the articular surface of the glenohumeral joint, is concave in shape and slightly retroverted 6.2°[28]. An abnormal glenoid shape, such as higher retroversion or smaller cavities, leads to a higher glenohumeral index (the relationship between the humeral head and glenoid). This may predispose posterior shoulder instability[29-31], although some authors were unable to reproduce this finding[32].
The most important osseous feature of the scapula is the coracoid process, which is tilted approximately 120°-160° anterolaterally[33]. It has several attachments, which have major impact on posterior instability: the coracobrachial muscle, the short head of the biceps brachii muscle, the pectoralis minor muscle, the coracohumeral ligament (although in a few cases they insert in the pectoralis minor muscle[34]), the coracoacromial ligament, as well as the coracoclavicular ligament. The individual function and mechanism of stabilization are discussed in full detail below.
The most frequent osseous lesion of the scapula involved during a posterior shoulder dislocation is the reverse Bankart lesion. It is located mainly in the posterior-inferior quarter of the glenoid (86%), and leads to an 86% increase in posterior translation and 31% increase in inferior translation of the humerus in the sulcus position. In patients with posterior capsular tears or posterior Bankart lesions, a bidirectional instability must be suspected[35].
In large glenoid defects, a posterior bone block transfer can be performed to extend the glenoid surface rather than reconstruct the glenoid anatomically. Additional indications for posterior bone block transfer include glenoid erosions, failure of primary capsular plication or congenital abnormalities. This procedure can be considered the counterpart to the Latarjet procedure, and was first described by Hindenach in 1947[36].
Overall, the posterior bone block transfer procedure shows poor results, with a high rate of osteoarthritis in long-term follow-up, although three of 11 patients were pleased with it[36].
In patients who suffer from higher glenoid retroversion (more than 15°-20°) with intact soft tissue, an open wedge osteotomy may be the treatment of choice. DeLong et al[37] performed a systematic literature review, stating that posterior glenoid osteotomy does not show any good results in terms of return to pre-injury athletic level[22,38].
Humeral head: The humeral head presents anatomically with a retroversion of 25°-35° (related to the condyles of the elbow) and an inclination of about 130° related to the shaft[39,40]. It consists of hyaline cartilage (thickest in the center) and forms a true sphere[41,42]. Tendinous and ligamentous attachments form a ring to tighten and centralize the humeral head, placing it in the middle of the glenoid cavity[43,44]. Even though no data exist, it is likely that retroversion of > 35° in the humeral head may predispose posterior luxation, similar to retroversion of the glenoid.
Glenohumeral joint: The glenohumeral joint permits movement with many degrees of freedom, including flexion-extension, abduction-adduction, circumduction and medial-lateral rotation. Humeral motion is possible in the frontal, coronal/sagittal and scapular planes[25,45].
Damage of articular cartilage and reverse Hill Sachs lesions, also called Malgaigne fractures, are rather infrequent complications of posterior shoulder instability. In high traumatic injuries, Malgainge fractures may lead to painful clicking or catching in movements, which may worsen the damage and lead to further injuries.
Surgical correction of a reverse Hill Sachs lesion includes the McLaughlin procedure, where the subscapularis tendon is transferred into the bony defect. Other procedures include implantation of bone allograft or humeral osteotomy when the retroversion may be suspected to predispose the instability. Rotational osteotomies have shown fair results, and one paper demonstrated a 50% return to a pre-injury level of activity[46].
Clavicle: The clavicle is less important than the scapula for posterior shoulder instability. Nevertheless, the S-shape bone does provide some elasticity, some component of shock absorption and forms a strut holding the glenohumeral joint in the parasagittal plane. At rest, it is tilted slightly superior by 10°-12°[25]. Major impact on the rotation in the coronal plane could be observed which increases from 3°-20° to 21°-150° of humeral elevation. Clavicle posterior rotation was increased by elevation in the sagittal plane between 20° at 90° to 27° at 150° of elevation as well as protraction from -17° to -45°[47].
The acromioclavicular joint is a synovial joint allowing anterior/posterior and internal/external rotation over the lateral end of the clavicle[48]. The sternoclavicular joint enables elevation and depression of the clavicle as well as protraction and retraction[48,49].
In an intact clavicle, the degree of freedoms are external rotation, upward rotation and posterior tilting, which are greatest in the sagittal plane, thus enabling more stabilization and support in glenohumeral joint motion[50].
According to Poppen et al[45], the relation between the glenohumeral and scapulothoracic movement has a ratio of 4.3:1, with an upward translation of 3 mm. When abducting the humerus, a counterclockwise rotation of the scapula in the frontal plane is accompanied. Hereby, a rotation of the clavicle can be noted up to a taut costoclavicular ligament. After initial abduction by 30°, the glenohumeral and scapulothoracic joint movements occur simultaneously and facilitate elevation. Approximately 40° of abduction is enabled by the sternoclavicular joint, and 20° by the acromioclavicular joint[25,51].
With regards to the pathology of posterior shoulder instability, resistance to injury is provided substantially by the soft tissue. Most important are the subscapularis muscle, the coracohumeral ligament in neutral rotation, the coracohumeral ligament and the posterior band of the IGHL in internal rotation[20].
Shoulder capsule: It is believed that posterior instability is initiated by insufficiency of the capsule, which secondarily leads to laxity of the joint. Various angles of humerus abduction have been investigated, and emphasize the importance of the posterior capsule and the IGHL as significant stabilizers[52,53]. About 90% of patients show a rupture of the posterior capsule mainly on the scapular side after posterior shoulder dislocation. Ovesen et al[17,54] noted that between 40°-90° of abduction of the major stability is conferred by the entire posterior capsule. When sectioning posterior structures such as the teres minor, infraspinatus muscles and proximal half of the posterior capsule, there was a significant increase in posterior displacement.
Tears of the lower and proximal half of the posterior capsule have only little impact on stability in internal rotation (mainly above 40° of abduction). An entire rupture of the posterior capsule increases displacement in the last part of abduction, though not significantly. In cases of posterior structure trauma, an increase in anterior instability can also be seen[54].
On the other hand, lesions of the anterior capsule show even more impact on the posterior stability. The anterior capsule strengthens the glenohumeral ligaments by close adherence of the coracohumeral ligaments (superiorly), as well as the teres minor and infraspinatus tendons (posteriorly), and tightens in various positions. When sectioning the entire anterior capsule, posterior displacement significantly increases in abduction between 0°-90°[17].
Labrum: The labrum is a circumferential soft tissue extension of the bony glenoid rim, which is loosely attached to the surrounding capsule. It allows compressing forces, called “concavity compression”, for stabilization and enables centralization of the humeral head[55]. In 52%-66%, a posterior labrum defect (also called posterior/reverse Bankart lesion) can be found after traumatic posterior shoulder dislocation[56]. No consensus exists on the association between posterior capsular laxity and reverse Bankart lesions[53,57].
Ligaments: There are several ligaments that provide passive glenohumeral stabilization and help control the external forces on glenohumeral articulation.
The coracohumeral ligament is divided into a superficial and deep layer. The deep layer inserts into the rotator interval. It consists of fibers originating from the coracoid process and crisscrossing the supraspinatus and subscapularis muscles. These fibers form the pulley system that stabilizes the long head of the biceps at the entrance into the sulcus bicipitalis[57,58]. It allows external rotation and resists inferior and posterior translation in the suspended shoulder, which enables resistance to posterior subluxation in the neutral position[20,58].
Three main strands build the glenohumeral ligament: the superior, middle and IGHL. The influence of the IGHL on shoulder stability is well-described. It is a thickening of the capsule with a prominent anterior band (between 2-4 o’clock)[59] and a less prominent posterior branch. Typically, the posterior band or IGHL ruptures (posterior inferior part) in posterior dislocation (23 Blasier 1997), which can be provoked by elevation to 90° and abduction of internal rotation.
Today, most stabilization procedures are performed arthroscopically and target the capsulolabral complex. Surgical techniques can be divided into those inclusive or exclusive of suture anchor capsulolabral repair.
Bradley et al[60] suggests using suture-anchor capsulolabral repair in completely- or partially-detached labral injury patterns. He stated a success rate of 92% and 68%, respectively, returning to baseline sport when using suture anchors; otherwise, 84% and 48%, respectively, without suture anchors. The overall satisfaction is stated to be 94%, as measured using the American Shoulder and Elbow Surgeons Shoulder (ASES) score[60]. Savoie et al[53] published a study stating that the success rate was 97% based on the Neer Foster rating scale in 92 patients after arthroscopically capsulolabral repair. The overall satisfaction in those patients who returned to sport at a pre-injury level was approximately 63.5%, and the mean ASES score improved from 45.9 to 85.1[53,60]. Unfortunately, arthroscopic methods are somewhat limited, as the technique is not able to address severe erosions of the glenoid bone or retroversion of the glenoid exceeding 15°-20°, nor volitional instability[30,61].
A rather infrequent method is capsulorrhaphy, which shows good to excellent results in 73.3%; however 3 patients experienced recurrent instability according to Bisson et al[62]. It should be noted that surgical indications in this study were very closely controlled, as only patients with isolated posterior instability without labral detachment underwent this technique.
Muscles: There are 17 muscles with origins or insertions at the scapula, and these can be classified according to their function and location. Three main groups exist: Scapular stabilizers (n = 6), Rotator cuff (n = 4) and Scapulohumeral muscles (n = 6). The omohyoid muscle is not included in this simple classification, as it originates from the superior border of the scapula yet functionally depresses the larynx and hyoid. All tendons of the rotator cuff interact intricately with the fibrous capsule, which allows dynamic stabilization and movement of the glenohumeral joint. This group includes the infraspinatus, subscapularis, supraspinatus and teres minor. After posterior shoulder dislocation, a rupture of the teres minor and infraspinatus tendon is present in most of the cases (90% partial, 10% total rupture)[25].
Biomechanical investigations after teres minor tenotomy demonstrate an increase of internal rotation by 7° at 30°-40° of humeral abduction compared to an intact glenohumeral joint. Similarly, infraspinatus tenotomies show a significant increase in internal rotation between 0° and 30°-50° of abduction[32,54,63].
The scapular stabilizers include the levator scapulae (elevates and rotates the scapula), the pectoralis minor (protracts, rotates downwards and depresses the scapula), the major and minor rhomboid muscles (retract and elevate the scapula to depress the glenoid cavity, the serratus anterior (performs protraction and upward scapular rotation) and the trapezius muscle (a passive and dynamic scapular stabilizer, active elevator of the lateral scapular angle, scapular retractor and rotator). The pectoralis major, which does not attach the scapula, potentiates the scapulothoracic stabilization of the latissimus dorsi and deltoid muscle. This leads to a space in scapulothoracic articulation between the surface of the posterior thoracic cage and the subscapular fossa[25,58], thus facilitating gliding movement.
The last group includes the scapulohumeral muscles, which are responsible for stabilizing the humeral head. The biceps brachii muscle attaches with both heads to the scapula, the long and short head which work as elbow flexors and forearm supinators. Its antagonist muscle is the triceps brachii muscle long head, which extends the elbow as well as acts as an adductor of the elbow and of the humerus. Flexion and adduction of the humerus is performed by the coracobrachial muscle, and the prime mover of the glenohumeral abduction, flexion, extension and adduction of the humerus is the deltoid muscle. The latissimus dorsi and teres major muscles perform adduction, internal rotation of the humerus, rotation of the trunk (latissimus dorsi) and extension of the humerus (teres major)[44,64].
In the literature, several different treatment algorithms have been developed based on bony defects, osteoarthritis and the physical state of patients[65-68]. In athletes, authors tend to be a bit more aggressive in terms of surgical procedures. Guehring et al[69] additionally considers the time interval between trauma and surgery. Conservative therapy is a reasonable initial treatment, as one study demonstrated a subjective improvement after 6 mo in 70%-89% of patients. To avoid repetitive dislocation, certain exercises (internal rotation and horizontal adduction) and activities should be avoided for life[70-72].
Directly after trauma, the shoulder should be kept in slight external or neutral rotation to avoid any stress to the posterior capsule. In physical therapy, a general strengthening of the dynamic muscular stabilizers is essential. This includes the rotator cuff (with focus on external rotation), infraspinatus muscle, teres minor, periscapular muscles (for scapulohumeral rhythm) and posterior deltoid muscle[73]. The aim of physiotherapeutic exercises is to compensate for the injured static structures of bone and tissue[68,74].
For postoperative care, various protocols have been described. The shoulder is immobilized with an orthosis in 30° of abduction and 0° of rotation to prevent internal rotation. Cryotherapy is recommended and active elevation should be avoided for at least 4 wk. In the following weeks, passive and active assisted movements are recommended, followed by full passive and active range of motion 2 to 3 mo after. When the muscle strength is at least 80% of the contralateral side, a sport-specific rehabilitation program can be pursued, which is generally 6 mo post-operatively[36,60,74].
As there are only a few evidence-based studies regarding treatment protocols and techniques, it is difficult to develop a uniform algorithm. The different treatment options, such as conservative and operative treatment, and success rates are summarized in Table 2.
| Procedure | Consideration | Success rate |
| Conservative | Leads to loss of rotation and deformity of the shoulder, mainly performed in elderly patients | 68%-77%, however only in isolated posterior shoulder instability; recurrence rate up to 96%[38,86] |
| Capsular-labral repair (i.e., post. - inf. capsular shift) or reverse Bankart repair | In isolated unidirectional posterior instability | 96% in post. - inf. capsular shift[73] 91% in posterior capsulorrhaphy in isolated post. instability[5] Posterior Bankart repair – 93%[87] |
| Other procedures not/or rarely performed: | ||
| Thermal capsulorrhaphy | High recurrence rate | 57%, capsular insufficiency 33%[88,89] |
| Posterior bone block or posterior wedge osteotomy | After failed capsular plication, or congenital formations | Posterior glenoid transfer: 53%; 41% complication rate[22,90] Posterior bone block: 45%; 36% osteoarthritis[36] |
| McLaughlin’s procedure | In patients with locked posterior shoulder dislocation from reverse Hill-Sachs lesions | improvement in average constant scoring system from 16 preoperatively to 72 postoperatively[91] |
| Humeral head allograft | Alternative option to McLauglin’s procedure | Complication rate between 25%-50%[92,93] |
Posterior shoulder instability seems to be underdiagnosed due to its complexity and limited diagnostic examinations in general practice. So far, no real consensus on classification of posterior shoulder instability exists. Moreover, the correct mechanism of injury is not well understood, which has led to a lack of consensus regarding treatment regimens and general awareness by physicians.
Posterior shoulder instability can be provoked according to the Kim/Jerk test in forward flexion, adduction and internal rotation. A variety of reasons for posterior shoulder instability have been described. The most important ones are capsular lesions, especially anterior ones as well as ruptures of the IGHL. Patients who suffered from posterior shoulder dislocation mostly suffer from a rupture of the posterior capsule, loosening of the posterior labrum, and a rupture of the teres minor and/or infraspinatus tendon. This increases the risk of recurrent posterior shoulder instability, especially in abduction between 0°-90°. Further predisposing conditions, which have not yet been well investigated, include retroversion of the glenoid or humeral head.
Current treatment options vary in outcome in long-term follow-up. Currently, the best results have been observed using arthroscopic capsulolabral repair in conjunction with a careful postoperative management, with a delay in return to sport of about 4-6 mo.
With regards to the current biomechanical literature describing posterior shoulder dislocations, the predominant form of experimentation has used a static glenohumeral model. To our knowledge, no dynamic model yet exists to investigate the entire shoulder complex, including the scapulothoracic joint.
The authors would like to thank Dr. Charles M Jobin for his assistance and for providing the MR arthrography and intraoperative imaging, as well as Lee Ann Finno for her administrative support.
Manuscript source: Unsolicited Manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Guerado E; Malik H; Emara KM S- Editor: Dou Y L- Editor: Filipodia E- Editor: Wu YXJ
| 1. | Xu W, Huang LX, Guo JJ, Jiang DH, Zhang Y, Yang HL. Neglected posterior dislocation of the shoulder: A systematic literature review. J Orthop Translat. 2015;3:89-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Loebenberg MI, Cuomo F. The treatment of chronic anterior and posterior dislocations of the glenohumeral joint and associated articular surface defects. Orthop Clin North Am. 2000;31:23-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 54] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Cooper A. On the dislocations of the os humeri upon the dorsum scapulae and upon fractures near the shoulder joint. A Guys Hosp Rep. 1839;4:265-284. |
| 4. | Malgaigne JF. Traité des fractures et des luxations. Paris: JB Bailliere. 1855;. |
| 5. | Fronek J, Warren RF, Bowen M. Posterior subluxation of the glenohumeral joint. J Bone Joint Surg Am. 1989;71:205-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 180] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Nho SJ, Frank RM, Van Thiel GS, Wang FC, Wang VM, Provencher MT, Verma NN. A biomechanical analysis of shoulder stabilization: posteroinferior glenohumeral capsular plication. Am J Sports Med. 2010;38:1413-1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Kim SH, Ha KI, Yoo JC, Noh KC. Kim’s lesion: an incomplete and concealed avulsion of the posteroinferior labrum in posterior or multidirectional posteroinferior instability of the shoulder. Arthroscopy. 2004;20:712-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Provencher MT, King S, Solomon DJ, Bell SJ, Mologne TS. Recurrent Posterior Shoulder Instability: Diagnosis and Management. Oper Tech Sports Med. 2005;13:196-205. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Lamar DS, Williams GR, Iannotti JP, Ramsey ML. Posterior Instability of the Glenohumeral Joint: Diagnosis and Management. The University of Pennsylvania Orthopaedic Journal. 2001;14:5-14. |
| 10. | Steinmann SP. Posterior shoulder instability. Arthroscopy. 2003;19 Suppl 1:102-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Bradley JP, Baker CL 3rd, Kline AJ, Armfield DR, Chhabra A. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders. Am J Sports Med. 2006;34:1061-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 12. | Harryman DT 2nd, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA 3rd. Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72:1334-1343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 606] [Cited by in RCA: 498] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 13. | Lippitt SB, Vanderhooft JE, Harris SL, Sidles JA, Harryman DT 2nd, Matsen FA 3rd. Glenohumeral stability from concavity-compression: A quantitative analysis. J Shoulder Elbow Surg. 1993;2:27-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 298] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 14. | Wuelker N, Brewe F, Sperveslage C. Passive glenohumeral joint stabilization: A biomechanical study. J Shoulder Elbow Surg. 1994;3:129-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Harryman DT 2nd, Sidles JA, Harris SL, Matsen FA 3rd. The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992;74:53-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 524] [Cited by in RCA: 404] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 16. | Helmig P, Søjbjerg JO, Sneppen O, Loehr JF, Ostgaard SE, Suder P. Glenohumeral movement patterns after puncture of the joint capsule: An experimental study. J Shoulder Elbow Surg. 1993;2:209-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Ovesen J, Nielsen S. Anterior and posterior shoulder instability. A cadaver study. Acta Orthop Scand. 1986;57:324-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 95] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Michaelis LS. Internal rotation dislocation of the shoulder; report of a case. J Bone Joint Surg Br. 1950;32-B:223-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Rockwood CA. Posterior dislocation of the shoulder. Philadelphia: JB Lippincott: Rockwood, C.A., Green, D.P 1984; . |
| 20. | Blasier RB, Soslowsky LJ, Malicky DM, Palmer ML. Posterior glenohumeral subluxation: active and passive stabilization in a biomechanical model. J Bone Joint Surg Am. 1997;79:433-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 107] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Hawkins RJ, McCormack RG. Posterior shoulder instability. Orthopedics. 1988;11:101-107. [PubMed] |
| 22. | Hawkins RJ, Koppert G, Johnston G. Recurrent posterior instability (subluxation) of the shoulder. J Bone Joint Surg Am. 1984;66:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 152] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 23. | Schwartz E, Warren RF, O’Brien SJ, Fronek J. Posterior shoulder instability. Orthop Clin North Am. 1987;18:409-419. [PubMed] |
| 24. | Pavic R, Margetic P, Bensic M, Brnadic RL. Diagnostic value of US, MR and MR arthrography in shoulder instability. Injury. 2013;44 Suppl 3:S26-S32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 25. | Peat M. Functional anatomy of the shoulder complex. Phys Ther. 1986;66:1855-1865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 70] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Terry GC, Chopp TM. Functional anatomy of the shoulder. J Athl Train. 2000;35:248-255. [PubMed] |
| 27. | Steindler A. Kinesiology of the Human Body under Normal and Pathological Conditions. Springfield, IL: Charles C Thomas 1955; . |
| 28. | Fuchs B, Jost B, Gerber C. Posterior-inferior capsular shift for the treatment of recurrent, voluntary posterior subluxation of the shoulder. J Bone Joint Surg Am. 2000;82:16-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 141] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 29. | Inui H, Sugamoto K, Miyamoto T, Yoshikawa H, Machida A, Hashimoto J, Nobuhara K. Glenoid shape in atraumatic posterior instability of the shoulder. Clin Orthop Relat Res. 2002;87-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Brewer BJ, Wubben RC, Carrera GF. Excessive retroversion of the glenoid cavity. A cause of non-traumatic posterior instability of the shoulder. J Bone Joint Surg Am. 1986;68:724-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 160] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 31. | Saha AK. Dynamic stability of the glenohumeral joint. Acta Orthop Scand. 1971;42:491-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 293] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 32. | Weber SC, Caspari RB. A biomechanical evaluation of the restraints to posterior shoulder dislocation. Arthroscopy. 1989;5:115-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 51] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 33. | Aggarwal A, Wahee P, Harjeet , Aggarwal AK, Sahni D. Variable osseous anatomy of costal surface of scapula and its implications in relation to snapping scapula syndrome. Surg Radiol Anat. 2011;33:135-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 34. | Yang HF, Tang KL, Chen W, Dong SW, Jin T, Gong JC, Li JQ, Wang HQ, Wang J, Xu JZ. An anatomic and histologic study of the coracohumeral ligament. J Shoulder Elbow Surg. 2009;18:305-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 35. | Wellmann M, Blasig H, Bobrowitsch E, Kobbe P, Windhagen H, Petersen W, Bohnsack M. The biomechanical effect of specific labral and capsular lesions on posterior shoulder instability. Arch Orthop Trauma Surg. 2011;131:421-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 36. | Meuffels DE, Schuit H, van Biezen FC, Reijman M, Verhaar JA. The posterior bone block procedure in posterior shoulder instability: a long-term follow-up study. J Bone Joint Surg Br. 2010;92:651-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 37. | DeLong JM, Bradley JP. Posterior shoulder instability in the athletic population: Variations in assessment, clinical outcomes, and return to sport. World J Orthop. 2015;6:927-934. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 38. | Hurley JA, Anderson TE, Dear W, Andrish JT, Bergfeld JA, Weiker GG. Posterior shoulder instability. Surgical versus conservative results with evaluation of glenoid version. Am J Sports Med. 1992;20:396-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 121] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 39. | Cyprien JM, Vasey HM, Burdet A, Bonvin JC, Kritsikis N, Vuagnat P. Humeral retrotorsion and glenohumeral relationship in the normal shoulder and in recurrent anterior dislocation (scapulometry). Clin Orthop Relat Res. 1983;8-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 40. | Iannotti JP, Gabriel JP, Schneck SL, Evans BG, Misra S. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am. 1992;74:491-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 395] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 41. | O’Brien SJ, Allen AA, Fealy S. Developmental anatomy of the shoulder and anatomy of the glenohumeral joint. In: Rockwood CA Jr, Matsen FA 111. The Shoulder Philadelphia. WB Saunders 1998; . |
| 42. | Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 754] [Cited by in RCA: 590] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 43. | Jobe CM. Gross anatomy of the shoulder. In: Rockwood CA Jr, Matsen FA 111. The Shoulder Philadelphia. WB Saunders 1998; . |
| 44. | Halder AM, Itoi E, An KN. Anatomy and biomechanics of the shoulder. Orthop Clin North Am. 2000;31:159-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 90] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 45. | Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 660] [Cited by in RCA: 538] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 46. | Surin V, Blåder S, Markhede G, Sundholm K. Rotational osteotomy of the humerus for posterior instability of the shoulder. J Bone Joint Surg Am. 1990;72:181-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 47] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 47. | Fung M, Kato S, Barrance PJ, Elias JJ, McFarland EG, Nobuhara K, Chao EY. Scapular and clavicular kinematics during humeral elevation: a study with cadavers. J Shoulder Elbow Surg. 2001;10:278-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 48. | Moseley HF. The clavicle: its anatomy and function. Clin Orthop Relat Res. 1968;58:17-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 19] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 49. | Frankel VH, Nordin M. Basic Biomechanics of the Skeletal System. Philadelphia, PA. Lea Febiger. 1980;. |
| 50. | Matsumura N, Nakamichi N, Ikegami H, Nagura T, Imanishi N, Aiso S, Toyama Y. The function of the clavicle on scapular motion: a cadaveric study. J Shoulder Elbow Surg. 2013;22:333-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 51. | Inman VT, Saunders JB, Abbott LC. Observations of the function of the shoulder joint.1944. Clin Orthop Relat Res. 1996;3-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 205] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 52. | Itoi E, Hsu HC, An KN. Biomechanical investigation of the glenohumeral joint. J Shoulder Elbow Surg. 1996;5:407-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 49] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 53. | Savoie FH 3rd, Holt MS, Field LD, Ramsey JR. Arthroscopic management of posterior instability: evolution of technique and results. Arthroscopy. 2008;24:389-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 98] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 54. | Ovesen J, Nielsen S. Posterior instability of the shoulder. A cadaver study. Acta Orthop Scand. 1986;57:436-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 55. | Bahk M, Keyurapan E, Tasaki A, Sauers EL, McFarland EG. Laxity testing of the shoulder: a review. Am J Sports Med. 2007;35:131-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 69] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 56. | Saupe N, White LM, Bleakney R, Schweitzer ME, Recht MP, Jost B, Zanetti M. Acute traumatic posterior shoulder dislocation: MR findings. Radiology. 2008;248:185-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 57. | Mair SD, Zarzour RH, Speer KP. Posterior labral injury in contact athletes. Am J Sports Med. 1998;26:753-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 81] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 58. | Lugo R, Kung P, Ma CB. Shoulder biomechanics. Eur J Radiol. 2008;68:16-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 108] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 59. | O'Brien SJ, Neves MC, Arnoczky SP, Rozbruck SR, Dicarlo EF, Warren RF, Schwartz R, Wickiewicz TL. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18:449-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 520] [Cited by in RCA: 381] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 60. | Bradley JP, McClincy MP, Arner JW, Tejwani SG. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 200 shoulders. Am J Sports Med. 2013;41:2005-2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 121] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 61. | Yanke AB, G.S. VT, LeClere LE, Solomon DJ, Bach BR, Provencher MT, Bach BR. Diagnosis and Arthroscopic Management of Posterior Shoulder Instability. American Academy of Orthopaedic Surgeons. Available from: Orthopaedic Knowledge Online 2011; 9: http://orthoportal.aaos.org/oko/article.aspx?article=OKO_SHO043. |
| 62. | Bisson LJ. Thermal capsulorrhaphy for isolated posterior instability of the glenohumeral joint without labral detachment. Am J Sports Med. 2005;33:1898-1904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 63. | Ovesen J, Söjbjerg JO. Posterior shoulder dislocation. Muscle and capsular lesions in cadaver experiments. Acta Orthop Scand. 1986;57:535-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 64. | Frank RM, Ramirez J, Chalmers PN, McCormick FM, Romeo AA. Scapulothoracic anatomy and snapping scapula syndrome. Anat Res Int. 2013;2013:635628. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 65. | Paul J, Buchmann S, Beitzel K, Solovyova O, Imhoff AB. Posterior shoulder dislocation: systematic review and treatment algorithm. Arthroscopy. 2011;27:1562-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 66. | Habermeyer P, Lichtenberg S. [Diagnosis and treatment of anterior and posterior shoulder dislocation. II. Treatment]. Chirurg. 2003;74:1178-1194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 67. | Cunningham G, Hoffmeyer P. [Posterior dislocation of the shoulder, challenges in diagnosis and management]. Rev Med Suisse. 2011;7:2489-2493. [PubMed] |
| 68. | Tannenbaum E, Sekiya JK. Evaluation and management of posterior shoulder instability. Sports Health. 2011;3:253-263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 69. | Guehring M, Lambert S, Stoeckle U, Ziegler P. Posterior shoulder dislocation with associated reverse Hill-Sachs lesion: treatment options and functional outcome after a 5-year follow up. BMC Musculoskelet Disord. 2017;18:442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 70. | Tibone JE, Bradley JP. The treatment of posterior subluxation in athletes. Clin Orthop Relat Res. 1993;124-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 71. | Burkhead WZ Jr, Rockwood CA Jr. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am. 1992;74:890-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 435] [Cited by in RCA: 301] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 72. | Engle RP, Canner GC. Posterior shoulder instability: approach to rehabilitation. J Orthop Sports Phys Ther. 1989;10:1-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 73. | Pollock RG, Bigliani LU. Recurrent posterior shoulder instability. Diagnosis and treatment. Clin Orthop Relat Res. 1993;85-96. [PubMed] |
| 74. | Seppel G, Braun S, Imhoff AB. Surgical Management of Posterior Shoulder Instability. ISAKOS: Brockmeier SF 2013; . |
| 75. | Acid S, Le Corroller T, Aswad R, Pauly V, Champsaur P. Preoperative imaging of anterior shoulder instability: diagnostic effectiveness of MDCT arthrography and comparison with MR arthrography and arthroscopy. AJR Am J Roentgenol. 2012;198:661-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 76. | Cvitanic O, Tirman PF, Feller JF, Bost FW, Minter J, Carroll KW. Using abduction and external rotation of the shoulder to increase the sensitivity of MR arthrography in revealing tears of the anterior glenoid labrum. AJR Am J Roentgenol. 1997;169:837-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 135] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 77. | Smith TO, Drew BT, Toms AP. A meta-analysis of the diagnostic test accuracy of MRA and MRI for the detection of glenoid labral injury. Arch Orthop Trauma Surg. 2012;132:905-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 78. | van de Bunt F, Pearl ML, Lee EK, Peng L, Didomenico P. Glenoid version by CT scan: an analysis of clinical measurement error and introduction of a protocol to reduce variability. Skeletal Radiol. 2015;44:1627-1635. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 79. | Kodali P, Jones MH, Polster J, Miniaci A, Fening SD. Accuracy of measurement of Hill-Sachs lesions with computed tomography. J Shoulder Elbow Surg. 2011;20:1328-1334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 80. | Rowan KR, Keogh C, Andrews G, Cheong Y, Forster BB. Essentials of shoulder MR arthrography: a practical guide for the general radiologist. Clin Radiol. 2004;59:327-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 81. | Castagna A, Nordenson U, Garofalo R, Karlsson J. Minor shoulder instability. Arthroscopy. 2007;23:211-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 82. | Shah N, Tung GA. Imaging signs of posterior glenohumeral instability. AJR Am J Roentgenol. 2009;192:730-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 83. | Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from "engaging/non-engaging" lesion to "on-track/off-track" lesion. Arthroscopy. 2014;30:90-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 413] [Cited by in RCA: 468] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 84. | Yu JS, Ashman CJ, Jones G. The POLPSA lesion: MR imaging findings with arthroscopic correlation in patients with posterior instability. Skeletal Radiol. 2002;31:396-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 85. | Ruiz Santiago F, Martínez Martínez A, Tomás Muñoz P, Pozo Sánchez J, Zarza Pérez A. Imaging of shoulder instability. Quant Imaging Med Surg. 2017;7:422-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 86. | Kirkley A, Griffin S, Richards C, Miniaci A, Mohtadi N. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder. Arthroscopy. 1999;15:507-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 237] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 87. | Garcia JC Jr, Maia LR, Fonseca JR, Zabeu JL, Garcia JP. Evaluation of arthroscopic treatment of posterior shoulder instability. Acta Ortop Bras. 2015;23:134-137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 88. | Hawkins RJ, Krishnan SG, Karas SG, Noonan TJ, Horan MP. Electrothermal arthroscopic shoulder capsulorrhaphy: a minimum 2-year follow-up. Am J Sports Med. 2007;35:1484-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 89. | Wong KL, Williams GR. Complications of thermal capsulorrhaphy of the shoulder. J Bone Joint Surg Am. 2001;83-A Suppl 2 Pt 2:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 178] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 90. | Norwood LA, Terry GC. Shoulder posterior subluxation. Am J Sports Med. 1984;12:25-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 64] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 91. | Delcogliano A, Caporaso A, Chiossi S, Menghi A, Cillo M, Delcogliano M. Surgical management of chronic, unreduced posterior dislocation of the shoulder. Knee Surg Sports Traumatol Arthrosc. 2005;13:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 92. | Gerber C, Lambert SM. Allograft reconstruction of segmental defects of the humeral head for the treatment of chronic locked posterior dislocation of the shoulder. J Bone Joint Surg Am. 1996;78:376-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 199] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 93. | Martinez AA, Navarro E, Iglesias D, Domingo J, Calvo A, Carbonel I. Long-term follow-up of allograft reconstruction of segmental defects of the humeral head associated with posterior dislocation of the shoulder. Injury. 2013;44:488-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |