Published online Oct 18, 2018. doi: 10.5312/wjo.v9.i10.185
Peer-review started: July 2, 2018
First decision: July 19, 2018
Revised: July 29, 2018
Accepted: August 4, 2018
Article in press: August 5, 2018
Published online: October 18, 2018
Processing time: 111 Days and 0.6 Hours
Pelvic instrumentation for neuromuscular scoliosis has been part of neuromuscular scoliosis surgery since the era of the Luque Galveston construct. Unit Rod (Medtronic Sofamor-Danek, Nashville, TN) instrumentation brought with it the concept of cantilever correction by placing the implants in the pelvis and then gradually bringing the rod to the spine by sequentially tightening the sublaminar wires, with the goal of creating a level pelvis over a straight spine. More recently surgeons have utilized pedicle screw constructs in which the corrective strategies have varied. Challenges with pelvic fixation using iliac screws linked to the spinal rod have led to the development of the S2-alar-iliac technique (S2AI) in which the spinal rod connects to the pelvic screw. The screw is placed in the S2 ala, crosses the sacro-iliac joint and into the ilium through a large column of supra-acetabular bone. This column is the same area used for anterior inferior iliac spine external fixation frames used in trauma surgery. S2AI screw placement can be technically difficult and can require experienced radiology technologists to provide the appropriate views. Additionally, although the technique was originally described being placed via freehand technique with intra-operative flouroscopy, the freehand technique suffers from the anatomic anomalies present in the pelvis in neuromuscular scoliosis. As such, we prefer to place them using intra-operative navigation for all pediatric spinal deformity cases. Below in detail we report our intra-operative technique and an illustrative case example.
Core tip: S2-alar-iliac technique (S2AI) screws are used commonly in 2018 in posterior spinal fusion surgery when a fusion to the pelvis is indicated. The benefits of this instrumentation choice are well known; and now with 3D technology surgeons can safely place S2AI screws reproducibly even in aberrant pediatric anatomy.
- Citation: Anari JB, Cahill PJ, Flynn JM, Spiegel DA, Baldwin KD. Intra-operative computed tomography guided navigation for pediatric pelvic instrumentation: A technique guide. World J Orthop 2018; 9(10): 185-189
- URL: https://www.wjgnet.com/2218-5836/full/v9/i10/185.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i10.185
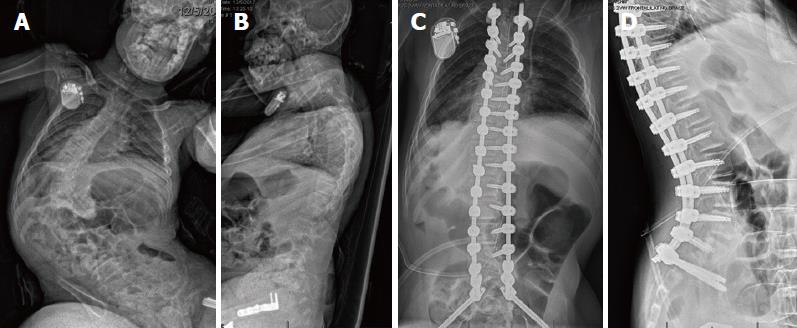
Neuromuscular scoliosis is a common cause of spinal deformity, and nonambulatory patients commonly have a thoracolumbar or lumbar curve associated with pelvic obliquity (Figure 1). While corrective strategies have varied, the initial approach using the Luque-Galveston technique involved extension of the spinal rod into the posterior ilium/pelvis. The corrective strategy in the unit rod occurred by first placing the pelvic limbs of the fixation in the pelvis, and then gradually bringing the rod to the spine by applying cantilever forces and sequentially tightening sublaminar wires to bring the spine to the rod[1]. Problems include prominence of the implants, loosening of the pelvic limbs within the pelvis (“windshield wipering”), and rod fracture. The unit rod is a pre-contoured rod which was developed to avert the need for intraoperative rod contouring, and the technique for correction was the same. Subsequent variations in lumbo-pelvic fixation have included iliac screws, which are placed into the posterior iliac crest and attached to the spinal rod via connectors. Some authors have placed duel screws into the ilium, while others have advocated for screws in both the first sacral vertebra and the ilium. Challenges with this fixation include implant prominence and failure of the implant at the junction between either the screw and the connector or the connector and the rod.
In 2007, Sponseller introduced the S2-alar-iliac technique (S2AI) in which the pelvic screw is placed from the sacrum into the pelvis. The screw head is low profile and connects directly with the spinal rod[2]. While initial reports documented safety and placement in both pediatric and adult spinal deformity patients, much of the recent literature regarding safety of placement using the S2AI technique has been published in adults[3-6]. Shillingford et al[3] report a free hand technique without intra-operative imaging that has a cortical breech rate of 7% posteriorly and 1% anteriorly. Anterior perforation into the pelvis or inferior perforation into the sciatic notch can have catastrophic result given the neurovascular and visceral structures found in such locations[3]. There may also be variations in anatomy, for example the relationship between the iliac wings and the pelvis. In the setting of considerable pelvic obliquity, the patient may bear weight on the downside iliac wing, and one may observe asymmetry in the relationship between the iliac wings and the pelvis such as adduction of one iliac wing with abduction of the other.
We have utilized computed tomography (CT) image navigation for placement of pedicle screws at our institution for more than 10 years, and we have extended this practice to the placement of S2AI screws[7]. Here we describe our technique for CT guided pediatric pelvic fixation using the S2AI technique.
The patient is placed in the prone position on an open Jackson table and a subperiosteal exposure from the upper instrumented vertebrae to S2 is performed. Adequate exposure on the sacrum includes visualization of both the S1 and S2 neural foramina. An anchor point is picked proximally in the lumbar or thoracic spine that is sturdy enough to hold a reference array (4 tines at a minimum) and simultaneously remain out of the surgeon’s working space while placing instrumentation. Our preferred location is the lower thoracic spine (T11/12) as this is usually far enough away to be out of the working field but not too far from the insertion point to alter the information acquired by the CT scan. Patient lordosis must be taken into account as significant differences in trajectory may lead to interference of the guidance probe with the sensor array.
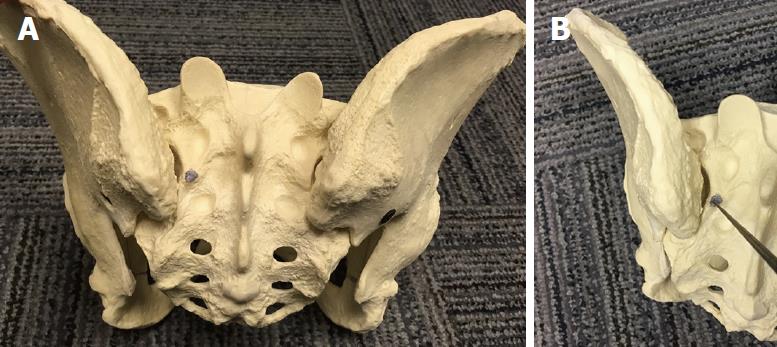
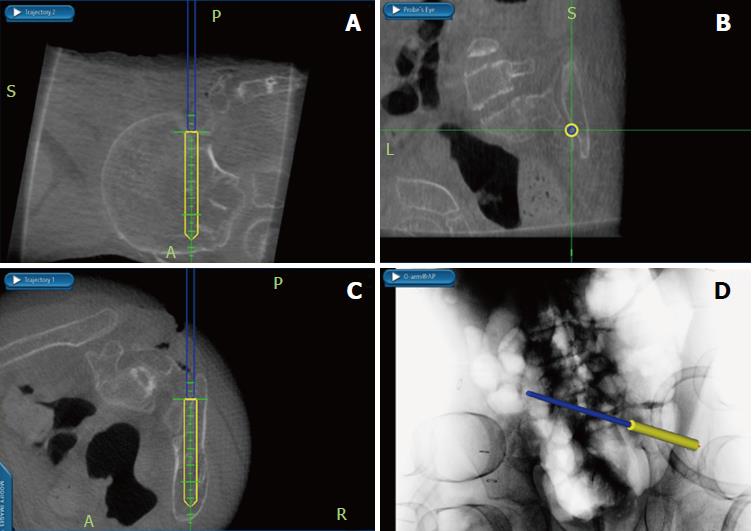
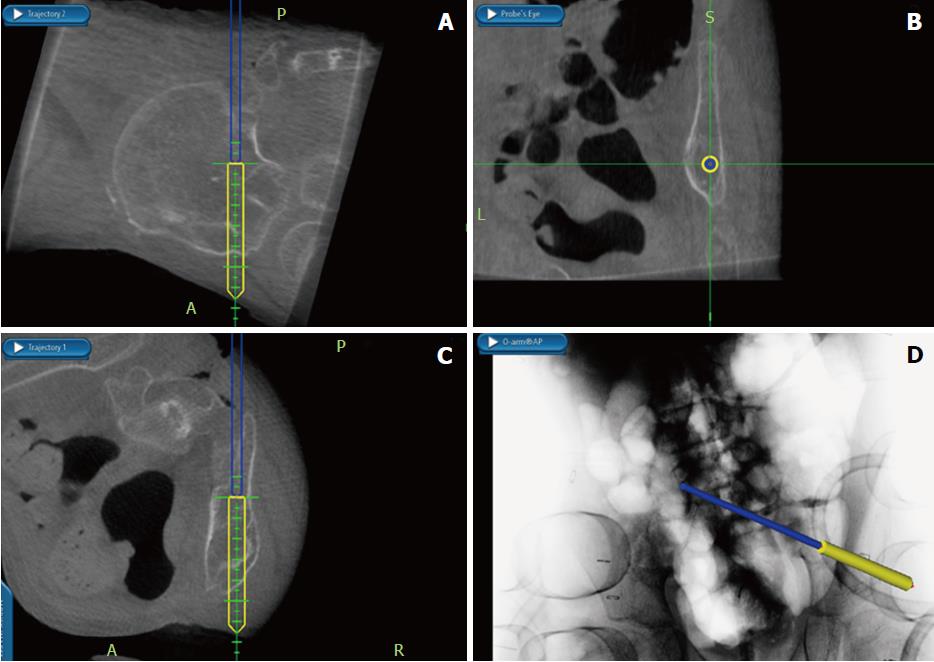
Once the exposure is complete and the array in a stable location a low dose CT scan (2.25 mSv) is performed from the top of the femoral heads to the lower lumbar spine region (O-Arm Medtronic Sofamor-Danek, Nashville, TN). Following completion of the CT scan the navigation probe (Figure 2) is connected to the array by docking the probe in the array’s recess. Once confirmation of coupling occurs 3D anatomy from the CT scan is confirmed by placing the probe over a lumbar spinous process correlating the imaging seen on the screen with the patient. The surgeon, who stands on the patient’s left places the right sided S2AI screw and switches sides for the left sided screw. The typical entry point insertion for the S2AI screws are just lateral to the lateral edge of the S1 and S2 foramina midway between the two (Figure 3), although minor variations may be required depending on the local anatomy. Once this point is identified using the probe a 4 mm acorn burr is used to create a pilot hole for the pedicle probe approximately 3 mm in depth. The navigation probe is replaced in the pilot hole to confirm trajectory in both the axial and sagittal planes. Normal anatomy puts the S2AI trajectory at approximately 40° lateral in the axial plane and 20°-40° caudal in the sagittal plane[2,8]. Once surgeon has trajectory memorized the straight gearshift is passed through the sacrum into the sacroiliac joint and into the ilium (Figure 4). In rare cases the proper trajectory may require that the screw be placed directly into the ilium and not through the sacrum.
On the navigation screen depth and trajectory can be checked anytime with gearshift removal and placement of navigation probe. The authors prefer to place gearshift to the desired screw depth, dilate the tract, and then place the navigation probe down the tract to ensure circumferential bone and a floor alongside a guide wire (Figure 5). A ball tip probe then palpates the walls of the tract, and the channel is tapped to a diameter 0.5 mm less than the desired screw diameter, over the guide wire. The walls of the tract are palpated one last time before the cannulated screw is placed over the guide wire. Lastly the navigation probe is placed down the cannulated screw to palpate a floor as well as ensure the trajectory taken by the screw (Figure 6). Final position of the S2AI screws align with the cephalad instrumentation facilitating rod insertion. Figure 7 depicts a patient with neuromuscular scoliosis and pelvic obliquity who had S2AI instrumentation placed during an instrumented posterior fusion.
The extension of spinal instrumentation and fusion across the lumbosacral junction and into the pelvis is required in a number of clinical scenarios in both children and adults. In the pediatric population this is most commonly to address pelvic obliquity in the neuromuscular population, while in adults a common indication is to achieve rigid distal anchors for correcting sagittal imbalance in the setting of osteoporotic bone and to enhance the chances of arthrodesis across the lumbosacral junction[9-12]. Each situation offers varying complexity with regard to the insertion of implants, for example in pediatric patients in which there may be variations in the relationship between the iliac wings and the sacrum. We have also observed that the isthmus may be quite narrow in some pediatric patients, and the navigation allows us to identify this and choose the optimal sized screw, which is important given the literature suggestion screw diameter < 8 mm are at an increased risk of implant complications[13].
We have utilized a CT guided approach for more than 10 years and have been satisfied with our ability to safely place the implants, and this approach also serves as a valuable training tool for our residents and fellows who are being exposed to the challenge of lumbo-pelvic fixation. Reports concerning both free hand instrumentation and navigation assisted instrumentation are available[14-16]. The discussions include a comparison of cost, radiation safety for patient/surgeon/staff, reliance on technology, and associated risks with the learning curve[17-19]. At our institution the intra-operative CT dose is extremely low and all faculty are prepared to place without image guidance if the technology fails intra-operatively[20].
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kung WM, Pavone V S- Editor: Ji FF L- Editor: A E- Editor: Song H
| 1. | Herkowitz HN, Garfin SR, Eismont FJ, Bell GR, Balderson RA. Rothman-Simeone the Spine. 6th edition. Philadelphia: Elsevier Saunders 2011; . |
| 2. | Chang TL, Sponseller PD, Kebaish KM, Fishman EK. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976). 2009;34:436-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 214] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 3. | Shillingford JN, Laratta JL, Tan LA, Sarpong NO, Lin JD, Fischer CR, Lehman RA Jr, Kim YJ, Lenke LG. The Free-Hand Technique for S2-Alar-Iliac Screw Placement: A Safe and Effective Method for Sacropelvic Fixation in Adult Spinal Deformity. J Bone Joint Surg Am. 2018;100:334-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 4. | Hu X, Lieberman IH. Robotic-guided sacro-pelvic fixation using S2 alar-iliac screws: feasibility and accuracy. Eur Spine J. 2017;26:720-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Shillingford JN, Laratta JL, Park PJ, Lombardi JM, Tuchman A, Saifi CS, Lehman RA, Lenke LG. Human versus Robot: A Propensity-Matched Analysis of the Accuracy of Free Hand versus Robotic Guidance for Placement of S2 Alar-Iliac (S2AI) Screws. Spine (Phila Pa 1976). 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Laratta JL, Shillingford JN, Lombardi JM, Alrabaa RG, Benkli B, Fischer C, Lenke LG, Lehman RA. Accuracy of S2 Alar-Iliac Screw Placement Under Robotic Guidance. Spine Deform. 2018;6:130-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 7. | Ughwanogho E, Patel NM, Baldwin KD, Sampson NR, Flynn JM. Computed tomography-guided navigation of thoracic pedicle screws for adolescent idiopathic scoliosis results in more accurate placement and less screw removal. Spine (Phila Pa 1976). 2012;37:E473-E478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 8. | Zhu F, Bao HD, Yuan S, Wang B, Qiao J, Zhu ZZ, Liu Z, Ding YT, Qiu Y. Posterior second sacral alar iliac screw insertion: anatomic study in a Chinese population. Eur Spine J. 2013;22:1683-1689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | O’Brien JP, Dwyer AP, Hodgson AR. Paralytic pelvic obliquity. Its prognosis and management and the development of a technique for full correction of the deformity. J Bone Joint Surg Am. 1975;57:626-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 28] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Hayer SD, Rabago DP, Amaza IP, Kille T, Coe CL, Zgierska A, Zakletskaia L, Mundt MP, Krahn D, Obasi CN. Effectiveness of nasal irrigation for chronic rhinosinusitis and fatigue in patients with Gulf War illness: protocol for a randomized controlled trial. Contemp Clin Trials. 2015;41:219-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Lee MC, Jarvis C, Solomito MJ, Thomson JD. Comparison of S2-Alar and traditional iliac screw pelvic fixation for pediatric neuromuscular deformity. Spine J. 2018;18:648-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Sponseller PD, Zimmerman RM, Ko PS, Pull Ter Gunne AF, Mohamed AS, Chang TL, Kebaish KM. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine (Phila Pa 1976). 2010;35:1887-1892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 150] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 13. | Jain A, Kebaish KM, Sponseller PD. Sacral-Alar-Iliac Fixation in Pediatric Deformity: Radiographic Outcomes and Complications. Spine Deform. 2016;4:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine (Phila Pa 1976). 2004;29:333-42; discussion 342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 515] [Cited by in RCA: 528] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 15. | Du JP, Fan Y, Wu QN, Wang DH, Zhang J, Hao DJ. Accuracy of Pedicle Screw Insertion Among 3 Image-Guided Navigation Systems: Systematic Review and Meta-Analysis. World Neurosurg. 2018;109:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 73] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 16. | Mason A, Paulsen R, Babuska JM, Rajpal S, Burneikiene S, Nelson EL, Villavicencio AT. The accuracy of pedicle screw placement using intraoperative image guidance systems. J Neurosurg Spine. 2014;20:196-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 264] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 17. | Hu X, Lieberman IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res. 2014;472:1839-1844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 124] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 18. | Yoshihara H, Paulino CB. Radiation Exposure to the Surgeons and Patients in Fluoroscopic-guided Segmental Pedicle Screw Placement for Pediatric Scoliosis. Spine (Phila Pa 1976). 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Ghasem A, Sharma A, Greif DN, Alam M, Maaieh MA. The Arrival of Robotics in Spine Surgery: A Review of the Literature. Spine (Phila Pa 1976). 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 139] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 20. | Sarwahi V, Payares M, Wendolowski S, Maguire K, Thornhill B, Lo Y, Amaral TD. Low-Dose Radiation 3D Intraoperative Imaging: How Low Can We Go? An O-Arm, CT Scan, Cadaveric Study. Spine (Phila Pa 1976). 2017;42:E1311-E1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |