Published online Sep 18, 2017. doi: 10.5312/wjo.v8.i9.735
Peer-review started: February 12, 2017
First decision: June 12, 2017
Revised: June 16, 2017
Accepted: July 21, 2017
Article in press: July 22, 2017
Published online: September 18, 2017
Processing time: 228 Days and 15 Hours
Osteogenesis imperfecta (OI) is a rare inherited connective tissue disorder caused by mutation of collagen which results in a wide spectrum of clinical manifestations including long bone fragility fractures and deformities. While the treatment for these fractures was recommended as using intramedullary fixation for minimizing stress concentration, the selection of the best implant in the adolescent OI patients for the surgical reconstruction of femur was still problematic, due to anatomy distortion and implant availability. We are reporting the surgical modification by using a humeral nail for femoral fixation in three adolescent OI patients with favorable outcomes.
Core tip: This case report presented the satisfactory clinical outcome of the adolescent osteogenesis imperfecta patients suffering from femoral fracture or bowing deformity which had been treated with the modification of humeral nail as intramedullary implant.
- Citation: Sa-ngasoongsong P, Saisongcroh T, Angsanuntsukh C, Woratanarat P, Mulpruek P. Using humeral nail for surgical reconstruction of femur in adolescents with osteogenesis imperfecta. World J Orthop 2017; 8(9): 735-740
- URL: https://www.wjgnet.com/2218-5836/full/v8/i9/735.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i9.735
Osteogenesis imperfecta (OI) is a rare hereditary connective tissue disorders with the common clinical presentation of excessive bone fragility caused by mutations in collagen[1]. Clinical manifestations of OI are wide spectrum and could be vary from lethal forms in the perinatal period to the subtle forms, which could be hardly identified and comparable to a normal person. However, the common orthopaedic problems in the OI patients, that is related to the excessive fragility, are frequent fractures, progressive deformity of long bones and impaired ambulation. The treatment of OI requires a multidisciplinary approach including both medical treatment, such as using bisphosphonates therapy to increase bone mineral density and reduce long bone fractures rate[2-4], and surgical treatment for fracture fixation or deformity correction[4].
Regarding surgical management of OI, the treatment goals are to minimize the incidence of fracture, restore bone axis and avoid bone bowing[4]. The recommended surgical implant in OI was a load-sharing intramedullary (IM) device, with the largest diameter as possible, due to the better biomechanical property in fragile bone over plate construct[1] and avoid plate-related complications, such as bony resorption from stress shielding, implant failure, and subsequent fracture at the plate ending[5,6]. However, the surgical fixation in OI, especially in adolescent OI patients with femoral fracture or nonunion, are still problematic due to particular abnormal femoral anatomy (such as short limb, non-anatomical alignment secondary to previous injury, and narrow and non-linear medullary canal with superphysiologic bowing)[1] resulting in implant selection difficulty which was suitable for medullary canal size and bone length. Although there is an advanced surgical system, like a telescopic rod, which is specifically designed for OI patients with many different sizes that allow fixation in all age groups, this implant is not available everywhere, including our country. Moreover, the traditional implant standard pediatric IM devices such as single Rush pin might not be appropriate in these adolescent OI patients due to its small size and inability to provide rotational stability[6-8]. Recently, there has been a few studies which reported that the small IM interlocking nail, such as humeral nail, could be used in femoral fixation in normal adolescent patients due to the advantages of the entry point lateral to tip of greater trochanter resulting in avoiding iatrogenic vascular injury and being the IM locking device with smaller diameter and shorter length than conventional femoral nail which was appropriate for small-sized adolescent femoral anatomy[9,10]. Therefore, this humeral nail should be also suitable for femoral fixation in adolescent OI patients. This study aimed to demonstrate the outcome of adolescent OI patients with femoral fracture or deformity and treated with humeral nail fixation.
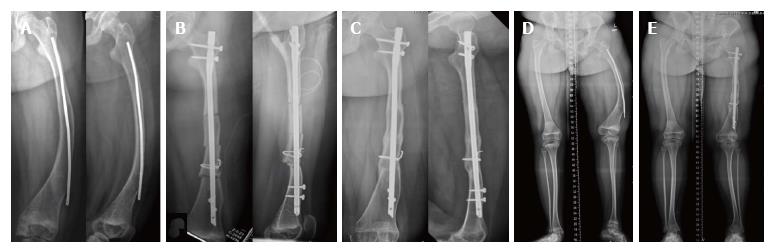
A 12-year-old girl with type I OI presented with progressive left femur deformity (August, 2013). Her height and weight were 138 cm and 51 kg. Initially, she had been diagnosed as type Ib (Silence classification)/Tarda B (Shapiro classification) and received treatment since age of 7 years. Three years ago (2010), she had been treated with corrective osteotomy and Ender nail fixation for left femur bowing deformity and the fracture was united uneventfully. However, she had experienced the progressive deformity on her left thigh without pain on weight bearing. The radiographs showed anterolateral femoral bowing due to femoral varus and flexion deformity with 8.5-mm medullary canal diameter (Figure 1A).
Preoperative planning for progressive left femoral deformity was discussed. The goal of treatment was rigid fixation with load-sharing intramedullary (IM) device[1]. The IM instrument options were K-wire, Rush pin, and telescoping IM device. K-wire and Rush was suitable only for small children with small IM canal due to the size of implant. Telescoping IM device was suitable for older children with larger IM canal, although this device was not available in our country. Therefore, we decided to use humeral IM nail for femoral osteotomy stabilization in this case due to two reasons. Firstly, the humeral nail was the interlocking nail that was available in smaller size and shorter length than conventional femoral nail. Thus, the humeral nail would be better in biomechanical property than single Rush pin. Secondly, the humeral nail geometry was rather straight than femoral nail resulting in the more lateral entry point for humeral nail insertion at the lateral to the tip of greater trochanter, and so avoiding the iatrogenic vascular injury on piriformis fossa.
Surgical technique: The patient was placed in lateral decubitus position under general anesthesia (GA). Multi-level corrective osteotomy was performed with drill and osteotome. Then the femur was reduced to acceptable alignment. The entry point was made at the tip of greater trochanter (GT), and the medullary canal was gently prepared by hand reaming using 6-mm and 7-mm T-reamer. Then a 7-mm diameter Expert humeral nail (Synthes®, Inc.) with 290-mm length was inserted following by proximal blade and distal locking screw insertion under fluoroscopic guidance. One additional wiring was performed due to iatrogenic cortical crack on the osteotomized fragment (Figure 1B). The operative time was 4 h, and the total length of hospital stay was 6 d. Estimated blood loss was 350 mL.
Postoperative care and rehabilitation: The postoperative protocol was initially 6-wk toe touch weight bearing with gait aids following by progressive weight bearing as tolerated. The patient reported clinical union (pain-free full weight bearing without tenderness on osteotomy site) at 6 mo postoperatively, and the radiographic union was completed at 9 mo postoperatively (Figure 1C). On 3-year postoperative follow-up period, the patient had normal hip range of motion and function. The radiographs showed no evidence of avascular necrosis of femoral head (Figure 1D and E).
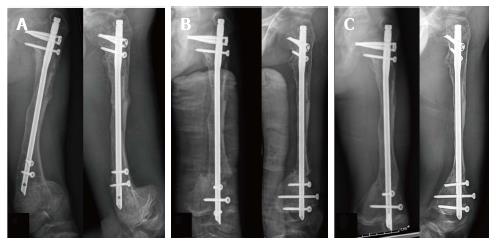
A 12-year-old girl with type III OI presented with left femoral shaft oligotrophic nonunion with failed Rush pin fixation (2014). Her height and weight were 122 cm and 25 kg. She had been diagnosed as type III (Silence classification)/Tarda A (Shapiro classification) after birth and treated with intravenous bisphosphate therapy since the age of 3 mo. On 2010, at the age of 7 years, she sustained left femoral shaft fracture and had been treated with single Rush pin fixation (Figure 2A and B). After surgery, she was lost to follow-up for 3 years (2011-2014) and then came back to our clinic 4-year postoperatively with limping and mild pain on full weight bearing. The radiographs showed that the fracture was still non-united with progressive bending of Rush pin (Figure 2C), and the medullary canal diameter was 9.2 mm. Therefore, the revision operation was planned as Rush pin removal with nonunion resection and humeral nail insertion with local bone graft.
Surgical technique: The patient was placed on lateral decubitus position under general anesthesia. The Rush pain was removed from old surgical scar. The nonunion site was opened directly with subvastus approach. Nonunion fibrous tissue was resected and previous bony callus was harvested for local bone graft. The humeral nail insertion was performed, with the same technique as above, using previous Rush pin entry point at the tip of GT. A 8-mm diameter M/DN Humeral Intramedullary nail (Zimmer, Warsaw, IN) with 255-mm length was applied and locked proximally and distally. Then local bone graft was inserted around the fracture site (Figure 2D). The operative time was 3.5 h, and the total length of hospital stay was 5 d. Estimated blood loss was 300 mL.
Postoperative care and rehabilitation: The patient was allowed 6-wk toe touch weight bearing followed by progressive weight bearing as tolerated. The clinical union was achieved within 6 mo and the radiographic union was completed within 9 mo postoperatively (Figure 2E). On 2-year postoperative follow-up period, the patient had normal function without pain on FWB. The radiographs showed no evidence of avascular necrosis of femoral head (Figure 2F).
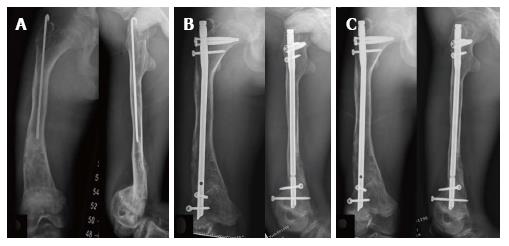
A 16-year-old male with type III OI presented with left subtrochanteric peri-implant fracture after falling on the ground (September, 2014). His height and weight were 130 cm and 27 kg. He was diagnosed as type III (Silence classification)/Congenita A (Shapiro classification) during antenatal care period, and treated with intravenous bisphosphate therapy since the age of 19 mo. He had previous bilateral leg deformity and had been treated with bilateral femoral and tibial corrective osteotomy. The radiographs showed displaced left subtrochanteric fracture below osteotomy plate with varus angulation, and bilateral distal femur extension deformity (Figures 3A, 4A, and 5A). The left and right medullary canal diameters were 8.6 and 9.0 mm respectively.
Surgical technique: After preoperative planning was discussed, bilateral staged femoral reconstructions were planned as: (1) osteotomy plate removal and humeral nail insertion (August, 2014) (Figure 3B); (2) corrective hinged osteotomy left distal femur with humeral nail (June 2015) (Figure 4B); and (3) corrective osteotomy right distal femur with humeral nail (March, 2016) (Figure 5B). All operations were performed using the same technique as mentioned above with Expert humeral nail (Synthes®, Inc.). The operative times were 2.5, 3.5, and 3 h respectively. The lengths of hospital stay were 4, 4, and 3 d. Estimated blood loss were 200, 500, and 350 mL, respectively.
Postoperative care and rehabilitation: After the first and second operation on left femur, due to bilateral deformity, the patient was allowed for 8-wk wheel chair mobilization, and followed by weight bearing as tolerated with full weight bearing after 3 mo postoperatively. The subtrochanteric fracture and osteotomy site both showed clinical union and radiographic union at 3-mo and 8-mo postoperatively (Figures 3C and 4C). After the third operation on his right femur, the postoperative protocol was the same as case no.1 and no.2 due to complete fracture healing with good alignment on left femur. The clinical and radiographic union were shown at 3-mo and 5-mo postoperatively, respectively (Figure 5C). At the most recent follow-up (postoperative 10 mo after the third operation), the patient showed normal hip range of motion with pain-free weight bearing. No avascular necrosis of femoral head was found.
OI is a heritable disorder of collagen synthesis that commonly presents as bone fragility with multiple long bone fractures and deformities. These boney problems usually require surgical management for fracture fixation or reconstruction by the load-sharing IM device. However, the surgical fixation in OI patients, especially in the older children with femoral fracture or deformity, is very difficult due to the abnormal femoral anatomy resulting in implant selection problems such as a mismatch with conventional femoral IM nail, the poor fixation stability of standard pediatric IM device (Rush pin), and the high cost of advanced telescopic rod. This study aimed to present the usefulness of humeral nail fixation as a surgical tool for femoral reconstruction in adolescent OI patients.
The humeral nail application for femoral fixation in adolescent OI patients has many advantages. Firstly, humeral nail implant, which is available in smaller diameter and shorter length than conventional femoral IM nail, is more suitable with these patients’ femoral anatomy with narrow medullary canal and short limb. Secondly, humeral nail geometry has narrow width and is easier to insert into the lateral transtrochanter area[9] which can avoid the risk of iatrogenic injury to greater trochanter physis[11] or medial femoral circumflex artery[12]. Thirdly, due to the interlocking nail property, the humeral nail would offer superior biomechanical benefits than the standard Rush pin fixation as better in rotational stability and leg length control, especially for the patients with multilevel corrective osteotomy.
However, there were also some limitations for using humeral nail for femoral reconstruction in adolescent OI patients. First, most of the humeral nail designs had only 90-100 degree of the cephalomedullary angle for proximal locking blade/screw, which was more varus than the neck-shaft angle of the femur and resulting in suboptimal fixation for proximal femur. Therefore, we recommended carefully adjustment of the proximal blade/screw position to achieve the best position and longest length as possible for the stable femoral head and neck fixation (Figures 2-5). Second, the required length for distal locking screw was usually longer than normal due to the wider width of distal femur than distal humerus, thus it was necessary to prepare the extra-length distal locking screw or using the other types of screw, such as 3.5 mm or 4.5 mm cortical screw, instead. Lastly, due to the abnormal femoral anatomy and using humeral nail design, we recommended performing the rotational alignment examination by intraoperative checking hip rotation in every cases.
The results of this study showed that using humeral nail implant in femoral fixation was possible and could be used in proximal, middle or distal location. Moreover, this option could be indicated for fixation of fracture and nonunion, or corrective osteotomy. Our study also demonstrated the favorable outcome with 100% fracture healing [the mean clinical union time of 4.2 mo (range 3-6 mo) and the mean radiographic union time of 7.8 mo (range 5-9 mo)] and without the implant-related complications such as infection, nonunion, or AVN. Therefore, we concluded that the humeral nail application for femoral fixation in adolescent OI patients would be one of the possible options with satisfactory outcomes.
Three adolescent patients with underlying osteogenesis imperfecta presented with progressive femoral deformity (case 1) or nonunion (case 2) or peri-implant fracture and bilateral distal femur deformity (case 3).
Case 1: Varus and flexion deformity on left femur without local tenderness. Case 2: Antalgic gait with pain on weight bearing, and local tenderness on the fracture site. Case 3: Moderate swelling, local tenderness on left thigh, and limited movement by pain with bilateral distal thigh deformity.
Progressive deformity associated with osteogenesis imperfecta (OI), fracture or osteotomy nonunion, infection, implant irritation.
All labs were within normal limits.
Case 1: Radiographs showed anterolateral femoral bowing deformity. Case 2: Radiographs showed persistent radiolucent line on fracture site and progressive Rush pin bending. Case 3: Radiographs showed displaced subtrochanteric fracture below osteotomy plate with bilateral distal femur deformity.
Case 1: Ender nails removal and multi-level corrective osteotomy with humeral nail. Case 2: Rush pin removal, and open reduction and internal fixation with humeral nail and local bone graft. Case 3: Bilateral staged femoral reconstructions; (1) osteotomy plate removal and humeral nail insertion; (2) corrective hinged osteotomy left distal femur with humeral nail; and (3) corrective osteotomy right distal femur with humeral nail.
The recommended surgical treatment of long bone fracture in OI patients is load-sharing intramedullary fixation to avoid plate-related complications (implant failure, peri-implant fracture, etc.). However, the femoral reconstruction in these adolescent OI patients was difficult due to the abnormal femoral anatomy (short limb, abnormal alignment from previous fracture or bowing, and narrow medullary canal), and the unavailability of the specific IM implant.
OI is a rare genetic disorder of the synthesis of collagen that mainly affects the bone, and commonly presents as recurrent fracture and deformity.
The humeral nail application for femoral fixation in adolescent OI patients should be performed with careful preoperative planning, gentle fracture manipulation, and strict postoperative rehabilitation protocol.
The authors demonstrated excellent results for treatment of femur deformity in OI adolescents with humeral nail. The paper is well written and instructive.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Thailand
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cui Q, Ohishi T S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Roberts TT, Cepela DJ, Uhl RL, Lozman J. Orthopaedic Considerations for the Adult With Osteogenesis Imperfecta. J Am Acad Orthop Surg. 2016;24:298-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Seikaly MG, Kopanati S, Salhab N, Waber P, Patterson D, Browne R, Herring JA. Impact of alendronate on quality of life in children with osteogenesis imperfecta. J Pediatr Orthop. 2005;25:786-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Shapiro JR, Thompson CB, Wu Y, Nunes M, Gillen C. Bone mineral density and fracture rate in response to intravenous and oral bisphosphonates in adult osteogenesis imperfecta. Calcif Tissue Int. 2010;87:120-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Burnei G, Vlad C, Georgescu I, Gavriliu TS, Dan D. Osteogenesis imperfecta: diagnosis and treatment. J Am Acad Orthop Surg. 2008;16:356-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Enright WJ, Noonan KJ. Bone plating in patients with type III osteogenesis imperfecta: results and complications. Iowa Orthop J. 2006;26:37-40. [PubMed] |
| 6. | Esposito P, Plotkin H. Surgical treatment of osteogenesis imperfecta: current concepts. Curr Opin Pediatr. 2008;20:52-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Gil JA, DeFroda SF, Sindhu K, Cruz AI Jr, Daniels AH. Challenges of Fracture Management for Adults With Osteogenesis Imperfecta. Orthopedics. 2017;40:e17-e22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Joseph B, Rebello G, B CK. The choice of intramedullary devices for the femur and the tibia in osteogenesis imperfecta. J Pediatr Orthop B. 2005;14:311-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Gordon JE, Khanna N, Luhmann SJ, Dobbs MB, Ortman MR, Schoenecker PL. Intramedullary nailing of femoral fractures in children through the lateral aspect of the greater trochanter using a modified rigid humeral intramedullary nail: preliminary results of a new technique in 15 children. J Orthop Trauma. 2004;18:416-422; discussion 423-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Park H, Kim HW. Treatment of femoral shaft fracture with an interlocking humeral nail in older children and adolescents. Yonsei Med J. 2012;53:408-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Raney EM, Ogden JA, Grogan DP. Premature greater trochanteric epiphysiodesis secondary to intramedullary femoral rodding. J Pediatr Orthop. 1993;13:516-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 64] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | O'Malley DE, Mazur JM, Cummings RJ. Femoral head avascular necrosis associated with intramedullary nailing in an adolescent. J Pediatr Orthop. 1995;15:21-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 91] [Article Influence: 3.0] [Reference Citation Analysis (0)] |