Published online Aug 18, 2017. doi: 10.5312/wjo.v8.i8.644
Peer-review started: January 20, 2017
First decision: February 15, 2017
Revised: March 9, 2017
Accepted: March 23, 2017
Article in press: March 25, 2017
Published online: August 18, 2017
Processing time: 202 Days and 22.5 Hours
To systematically review the incidence of ipsilateral graft re-rupture and contralateral anterior cruciate ligament (ACL) rupture following its reconstruction, with special attention to the femoral drilling technique.
Systematic review and meta-analysis of high-level prospective studies searched in MEDLINE database following PRISMA statement. The rate of ipsilateral graft re-rupture and contralateral rupture in patients submitted to either transtibial (TT) technique (isometric) or anteromedial (AM) technique (anatomic) was compared.
Eleven studies met the criteria and were included in final analysis. Reconstructions using the AM technique had a similar chance of contralateral ACL rupture when compared to the chance of ipsilateral graft failure (OR = 1.08, P = 0.746). In reconstructions using TT technique, the chance of contralateral ACL rupture was approximately 1.5 times higher than ipsilateral graft failure (OR = 1.49, P = 0.048). Incidence of contralateral lesions were similar among the techniques TT (7.4%) and AM (7.0%) (P = 0.963), but a trend could be noticed with a lower incidence of lesion in the ipsilateral limb when using the TT technique (4.9%) compared to the AM technique (6.5%) (P = 0.081).
ACL reconstruction by TT technique leads to lower incidence of graft re-injury than contralateral ACL lesion. There is no difference between the chance of re-injury after AM technique and the chance of contralateral ACL lesion (native ligament) with either technique.
Core tip: There is no convincing evidence that anatomic reconstruction leads to better clinical outcomes than transtibial (TT) reconstruction. Moreover, data suggests that it could lead to an increased risk of graft re-rupture. We found that anterior cruciate ligament (ACL) reconstruction by TT technique led to lower incidence of graft re-rupture than contralateral ACL lesion. The chance of graft re-rupture after anteromedial (AM) technique was the same of contralateral ACL lesion. There was no difference between contralateral lesion after both techniques and re-rupture after AM technique, what could mean that re-rupture chance after AM technique is indeed closer to normal knee, and, in fact, it is the TT technique’s re-tear incidence that is lower than it should be.
- Citation: de Campos GC, Teixeira PEP, Castro A, Alves Junior WM. Femoral positioning influences ipsi-and contralateral anterior cruciate ligament rupture following its reconstruction: Systematic review and meta-analysis. World J Orthop 2017; 8(8): 644-650
- URL: https://www.wjgnet.com/2218-5836/full/v8/i8/644.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i8.644
Optimal reconstruction technique for an anterior cruciate ligament (ACL) tear still on debate. In the last fifteen years literature has shown a significant shift in trends regarding graft positioning[1]. The “isometric” femoral graft positioning, made through the tibial tunnel (transtibial technique) and very popular during the last two decades of the twentieth century, is gradually being loathed[2]. Since the introduction of the anterior cruciate anatomic reconstruction concept[3], the pursuit of the ideal graft positioning has led to the so-called “anatomic” single-bundle reconstruction techniques, which can be accomplished by either by an anteromedial approach[4,5] as well as an outside-in femoral drilling[6].
Despite the plethora of anatomical and biomechanical studies suggesting incorrect graft positioning and inadequate knee rotational stability with transtibial (TT) femoral drilling technique, there is no convincing evidence that anatomic reconstruction leads to better clinical outcomes[7]. Moreover, recent data suggests that the anteromedial (AM) technique for femoral drilling could lead to an increased risk of graft re-rupture[8].
We hypothesized that the increased risk of graft re-rupture observed in anatomical reconstructions could in fact represent an approximation to the “normal knee” ACL rupture risk, that could be represented by the risk of contralateral knee lesion. This also would explain the odd finding that there is a higher incidence of contralateral knee ACL lesion when compared to graft re-lesion following ACL reconstruction by isometric technique[9].
Therefore, the aim of this study is to systematically review the incidence of ipsilateral graft re-rupture and contralateral ACL rupture following ACL reconstruction, with special attention to the femoral drilling technique.
Systematic review and meta-analysis of studies including patients submitted to ACL reconstruction, registered at PROSPERO under the number CRD 42015019336. PRISMA statement guidelines were followed for conducting and reporting meta-analysis data.
On September 13, 2015, a systematic literature search of the MEDLINE database was performed independently by two of the authors (Gustavo Constantino de Campos and Paulo Eduardo Portes Teixeira) using the following terms: “Anterior cruciate ligament” AND “contralateral” AND “reconstruction” AND “follow-up”. The initial search yielded 189 results. Eligibility criteria were original studies that included adult patients submitted to ACL reconstruction, in English language. Title and abstract evaluation suggested 156 articles for full text revision. Studies were excluded if did not specifically described drilling technique for ACL femoral tunnel confection, did not report the incidence of ipsilateral graft failure and incidence of contralateral ACL lesion during follow-up, if they were experimental studies (biomechanics or animal), if patients were submitted to revision surgery, double bundle or multiple ligaments reconstruction, or graft selection comprising allograft, artificial devices or harvested from contralateral knee. Risk of bias was minimized including only grade I to III prospective studies with a minimum of 75% of patients at final follow-up.
From the 156 articles reviewed, 145 articles were excluded, resulting in 11 articles for final analysis[10-20]. The references of the remaining eleven articles were reviewed with no additional studies for inclusion identified. These 11 studies provided the data for the present analysis. Literature review is summarized in Figure 1.
Extracted data included type of study, evidence level, patient demographics, follow-up duration, loss of follow-up, surgical technique, graft choice, ACL graft re-lesion incidence and contralateral ACL rupture incidence. Data were extracted by two authors independently (GCC and PEPT). Discrepancies were resolved by consensus.
A meta-analysis of the incidence of contralateral vs ipsilateral lesions to each of surgical techniques (AM and TT) was performed by “Comprehensive Meta-Analysis software version 3.3.070”. The heterogeneity of variances between studies was examined by χ2 test for heterogeneity and I2 statistics (proportion of the total variance due to heterogeneity) and χ2 (effect size variance between studies)[21,22]. When a significant heterogeneity was observed between studies, the combined effects across studies were analyzed by random effects model. When there was no significant heterogeneity between studies, these effects were analyzed using fixed effects model[22].
The estimate of the pooled effect (pooled odds ratio) between studies was calculated using the Mantel-Haenszel method (MH OR). Publication biases were analyzed by the asymmetry in the Begg and Mazumdar’s funnel plot[23]. Additionally, an association analysis between the surgical technique used (AM or TT) and the incidence of total ipsilateral and contralateral lesions of all publications was performed using χ2 2 × 2 test statistic in SPSS 18.0 software (SPSS Inc., Chicago, United States).
The chance of injury occurrence was calculated by OR using simple logistic regression in which was considered the sum of the number of events (contralateral or ipsilateral lesions) and the sum of the number of cases of all publications that have used the technique AM or TT separately. The significance level (α) used for all analyzes was 5% (P < 0.05).
All studies had a minimum of 2 years of follow-up after ACL reconstruction. The duration of follow-up’s ranged from 2 to 15 years. Data concerning the incidence of lesions were based on the total amount of individuals who have completed 100% of follow-up for each study. The percentage of individuals who completed the follow-up in each study ranged from 75% to 98% (Table 1).
| Author | Year | Evidence level | No. of initial patients | No. of patients included in follow-up | Follow-up (yr) | No. of contralateral injuries | No. of Ipsilaterais injuries |
| Anteromedial drilling technique | |||||||
| Webb | 2013 | 3 | 200 | 181 (91) | 15 | 19 (10.5) | 35 (19.3) |
| Shelbourne | 2009 | 2 | 1820 | 1415 (78) | 14 | 75 (5.3) | 61 (4.3) |
| Pinczewsky | 2007 | 2 | 180 | 178 (99) | 10 | 29 (16.3) | 19 (10.7) |
| Sajovic | 2006 | 1 | 64 | 61 (95) | 5 | 5 (8.2) | 4 (6.6) |
| Shaieb | 2002 | 1 | 82 | 70 (85) | 2 | 6 (8.6) | 4 (5.7) |
| Total | - | - | 2346 | 1905 (81) | - | 134 (7.0) | 123 (6.5) |
| Transtibial drilling technique | |||||||
| Barenius | 2014 | 1 | 164 | 134 (82) | 14.1 | 6 (4.5) | 6 (4.5) |
| Webster | 2014 | 3 | 750 | 561 (75) | 4.8 | 42 (7.5) | 25 (4.5) |
| Holm | 2010 | 1 | 72 | 57 (79) | 10 | 7 (12.3) | 6 (10.5) |
| Keays | 2007 | 2 | 62 | 62 (100) | 6 | 5 (8.1) | 1 (1.6) |
| Drogset | 2005 | 1 | 41 | 38 (93) | 2 | 1 (2.6) | 3 (7.9) |
| Aune | 2001 | 1 | 72 | 64 (89) | 2 | 3 (4.7) | 3 (4.7) |
| Total | - | - | 1161 | 916 (79) | - | 64 (7.4) | 44 (4.9) |
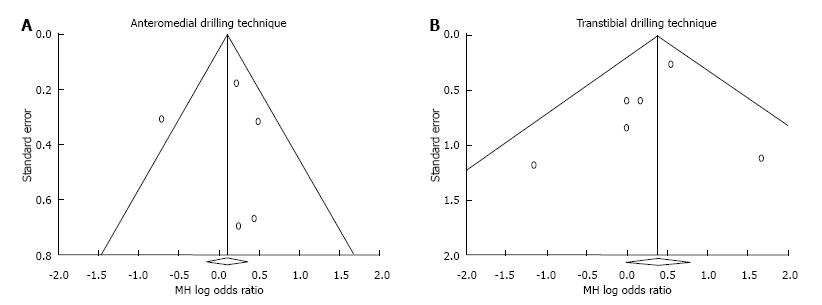
Study quality was assessed as recommended by previous studies[23,24]. Of the eleven studies included in this meta-analysis, 6 (55%) were classified as level of evidence 1, 3 (27%) with level of evidence 2 and 2 (18%) with evidence of Level 3 (Table 1). The potential bias across studies were evaluated by Begg and Mazumdar’s funnel plot for the incidence of contralateral and ipsilateral lesions in each of the AM and TT techniques, which were predominantly symmetrical, suggesting lack of significant biases in the publications included in the meta-analysis (Figure 2).
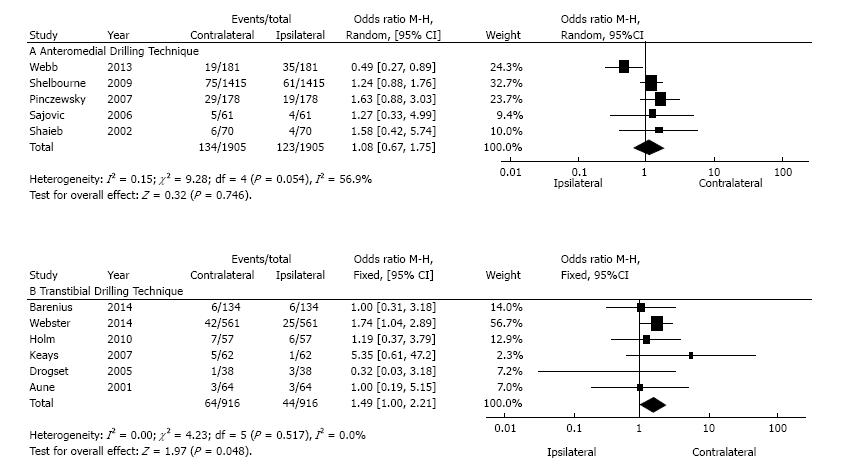
After the meta-analysis and combining the data, it was observed that ACL reconstructions using the AM technique had a similar chance of contralateral ACL rupture when compared to the chance of ipsilateral graft failure (MH OR = 1.08, 95%CI: 0.67 to 1.75, P = 0.746; Figure 3). However, after reconstructions using the TT technique, the chance of contralateral ACL rupture was approximately 1.5 times higher than the chance of ipsilateral graft failure (MH OR = 1.49, 95%CI: 1.00 to 2.21, P = 0.048, Figure 3). There was no heterogeneity of variances between studies using the TT technique (I2 = 0.0%, χ2 = 0.0, P = 0.517, Figure 3).
Nevertheless, those who used AM technique showed significant heterogeneity of variances (I2 = 56.9%, χ2 = 0.151, P = 0.054, Figure 3). Finally, from the publications included in the present meta-analysis (Table 1), no differences in the incidence of contralateral lesions were identified among the techniques TT (7.4%) and AM (7.0%) (OR = 0 99, 95%CI: 0.73 to 1.35, P = 0.963). But a trend could be noticed with a lower incidence of lesion in the ipsilateral limb when using the TT technique (4.9%) compared to the AM technique (6.5%) (OR = 0.73, 95%CI: 0.51 to 1.04, P = 0.081).
The present study found no difference between the risk of an ipsilateral graft re-rupture and a contralateral ACL rupture in individuals operated with the AM technique. There was also no difference in the risk of a contralateral ACL rupture when comparing both techniques (7%). However, the present analysis found a lower rate of ipsilateral graft re-rupture in patients operated with TT technique (4.9%; P = 0.048). This is the first analysis focusing the influence of femoral drilling technique over the graft failure and contralateral ACL lesion after ACL reconstruction.
Ipsilateral graft re-lesion is, for obvious reasons, an undesirable event, occurring in 1.8%[14] to 10.4%[25] of ACL reconstructed patients during the follow-up. Literature shows higher rates of contralateral ACL lesions than ipsilateral graft failure after ACL reconstruction[9]. An explanation to this finding could be inadequate rehabilitation[16] or even the assumption that the neoligament would be stronger than the original ACL[16]. Some authors attribute such finding to the protective role of the uninjured limb that renders it more suitable to lesion[26].
However, recent studies found a decrease in graft in situ forces when positioned in more vertical locations (isometric position), indicating that the femoral tunnel drilled through transtibial approach will result in a more vertical graft with in situ force lower than the in situ force found in the native ACL[27-29]. Therefore, the lower graft failure rates found in TT reconstruction could be because the neoligament simply is not submitted to the physiological forces that occur in the “normal” knee. With that in mind, one could speculate that it is not the AM technique that presents a higher failure rate, but the TT graft failure rate that is lower than it should be.
Anatomic ACL reconstruction results in graft inclination angle closer to the native ACL inclination angle and graft force and knee anterior laxity closer to those of the native knee[29]. It is our understanding that this could be the explanation to the findings of the present analysis, since we found same risk of contralateral ACL rupture (“normal” knee) for both techniques, with no difference for graft failure in the AM group (7%), and lower incidence of ipsilateral graft failure in TT group (4.9%, P = 0.048).
It is fundamental, thus, to provide information regarding femoral drilling technique when discussing ipsi or contralateral lesions rates during follow-up. Most of studies just focus on the graft choice and patient demographics. The vast majority of studies initially included in our analysis did not adequately describe the ACL reconstruction technique used. This is in accordance to van Eck et al[30], who examined 74 studies that claimed to use “anatomic technique” for ACL reconstruction and found a gross under-reporting of specific operative technique data.
Rahr-Wagner et al[8] found increased risk of revision in patients undergone to ACL reconstruction with femoral drilling through AM portal when compared to TT technique in the Danish Knee Ligament Reconstruction Register. They explained this finding as a result of a learning curve due to the introduction of a new and more complex technique. The higher force over the more anatomically placed grafts could be a more accurate explanation.
Our results indicate that the increased risk is in fact an approximation to the expected failure rate of the normal knee, that could be represented by the rate of contralateral ACL lesion. van Eck et al[31] found that the majority of graft failures following anatomic ACL reconstruction occurred between six and nine months postoperatively, precisely the commonly recommended period for return to sports. Although there has been a transition toward the “anatomic” reconstruction over the last decades, rehabilitation protocols still the same. Maybe the higher forces over the graft could alter the time frame for complete graft healing and maturation. More studies are needed on that matter.
In another point of view, one can argue that, since there is no convincing data on the superiority of anatomic technique regarding clinical outcomes, it would be better to chose a technique with a lower rate of graft failure (TT technique). This question will only be answered as longer follow-up of anatomic reconstruction series successfully demonstrates better clinical outcomes and lower evolution to osteoarthritis.
We acknowledge that this meta-analysis has strengths and limitations. One limitation is the lack of demographic data, such as age, gender, body mass index and level of activity. Post-operative rehabilitation protocols were not analyzed or even considered. We acknowledge the importance of rehabilitation data. However, meta-analysis was performed comparing two groups operated by the same authors, therefore subjected to same rehabilitation protocols. Also, we did not include anatomic reconstruction by out-in femoral drilling technique. We chose to use only AM technique to standardize our analysis.
In addition, we were not able to show the data on direct comparison between AM and TT techniques on graft failure and contralateral ACL rupture. To perform this comparison and present it in a meta-analysis format, the comparison effect between techniques would have to be presented individually in each study selected for this meta-analysis. All selected studies for this review were independent and presented only intra-technical comparisons. Although we performed an exploratory analysis to test the differences between the incidences of graft failure and contralateral ACL rupture among AM and TT techniques, it could be biased. This issue is still a gap in the literature and more clinical studies are needed to conduct future meta-analyzes to clarify the subject. The major strength is the rigorous criteria used. We only included studies that reported both ipsi-and contralateral failure information, thus ensuring proper comparison when performing the meta-analysis. Moreover, we only included high quality prospective studies with high level of evidence and loss of follow-up lower than 25%.
The ACL reconstruction by transtibial technique leads to lower incidence of graft re-injury than contralateral ACL lesion. There is no difference between the chance of re-injury after anteromedial technique and the chance of contralateral ACL lesion (native ligament).
Optimal reconstruction technique for an anterior cruciate ligament (ACL) tear still on debate. Evidence regarding the influence of graft femoral positioning over ipsilateral graft re-lesion and contralateral rupture following ACL reconstruction is conflicting.
Since the introduction of the anterior cruciate anatomic reconstruction concept, the pursuit of the ideal graft positioning has led to the so-called “anatomic” single-bundle reconstruction techniques. However, despite the plethora of anatomical and biomechanical studies suggesting incorrect graft positioning and inadequate knee rotational stability with transtibial (TT) femoral drilling technique, there is no convincing evidence that anatomic reconstruction leads to better clinical outcomes. Moreover, recent data suggests that the anteromedial (AM) technique for femoral drilling could lead to an increased risk of graft re-rupture.
This is the first analysis focusing the influence of femoral drilling technique over the graft failure and contralateral ACL lesion after ACL reconstruction. The authors found that ACL reconstruction by TT technique led to lower incidence of graft re-injury than contralateral ACL lesion. There was no difference between the chance of re-injury after AM technique and the chance of contralateral ACL lesion (native ligament) with any technique.
The increased risk of graft re-rupture observed in anatomical reconstructions could in fact represent an approximation to the “normal knee” ACL rupture risk, that could be represented by the risk of contralateral knee lesion. The lower graft failure rates found in TT reconstruction could be because the neoligament simply is not submitted to the physiological forces that occur in the “normal” knee. With that in mind, one could speculate that it is not the AM technique that presents a higher failure rate, but it is the TT graft failure rate that is lower than it should be, probably due to incorrect femoral positioning.
Transtibial technique refers to an anterior cruciate ligament reconstruction technique in which the femoral tunnel is created with a drill inserted through a tibial tunnel previously drilled. It leads to a non-anatomic positioning of the femoral tunnel, searching for an isometric position of the femoral tunnel. In the anteromedial portal technique, the femoral tunnel is created with a drill inserted through the arthroscopic anteromedial portal, which makes it possible to create the femoral tunnel in its anatomic position.
This is a very nice paper, it is well written with very interesting results and conclusions.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Brazil
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Fenichel I, Ohishi T S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Rayan F, Nanjayan SK, Quah C, Ramoutar D, Konan S, Haddad FS. Review of evolution of tunnel position in anterior cruciate ligament reconstruction. World J Orthop. 2015;6:252-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 75] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (1)] |
| 2. | Robin BN, Jani SS, Marvil SC, Reid JB, Schillhammer CK, Lubowitz JH. Advantages and Disadvantages of Transtibial, Anteromedial Portal, and Outside-In Femoral Tunnel Drilling in Single-Bundle Anterior Cruciate Ligament Reconstruction: A Systematic Review. Arthroscopy. 2015;31:1412-1417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 131] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 3. | Ferretti M, Ekdahl M, Shen W, Fu FH. Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy. 2007;23:1218-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 378] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 4. | Steiner M. Anatomic single-bundle ACL reconstruction. Sports Med Arthrosc. 2009;17:247-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Chalmers PN, Mall NA, Cole BJ, Verma NN, Bush-Joseph CA, Bach BR Jr. Anteromedial versus transtibial tunnel drilling in anterior cruciate ligament reconstructions: a systematic review. Arthroscopy. 2013;29:1235-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Arnold MP, Duthon V, Neyret P, Hirschmann MT. Double incision iso-anatomical ACL reconstruction: the freedom to place the femoral tunnel within the anatomical attachment site without exception. Int Orthop. 2013;37:247-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Riboh JC, Hasselblad V, Godin JA, Mather RC 3rd. Transtibial versus independent drilling techniques for anterior cruciate ligament reconstruction: a systematic review, meta-analysis, and meta-regression. Am J Sports Med. 2013;41:2693-2702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 96] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 8. | Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy. 2013;29:98-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 170] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 9. | Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93:1159-1165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 308] [Cited by in RCA: 271] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 10. | Aune AK, Holm I, Risberg MA, Jensen HK, Steen H. Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction. A randomized study with two-year follow-up. Am J Sports Med. 2001;29:722-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 293] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 11. | Shaieb MD, Kan DM, Chang SK, Marumoto JM, Richardson AB. A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:214-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 207] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 12. | Drogset JO, Grøntvedt T, Tegnander A. Endoscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone grafts fixed with bioabsorbable or metal interference screws: a prospective randomized study of the clinical outcome. Am J Sports Med. 2005;33:1160-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med. 2006;34:1933-1940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 163] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 14. | Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI. A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and Gracilis tendon graft. Am J Sports Med. 2007;35:729-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 149] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 15. | Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35:564-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 456] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 16. | Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 325] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 17. | Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38:448-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 160] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 18. | Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. 2013;41:2800-2804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 276] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 19. | Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42:1049-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 327] [Article Influence: 29.7] [Reference Citation Analysis (0)] |
| 20. | Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 373] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 21. | Petitti DB. Meta-analysis, decision analysis, and cost-effectiveness analysis: methods for quantitative synthesis in medicine. New York: Oxford University Press 2000; . |
| 22. | Higgins JPT, Green S, editors . Cochrane handbook for systematic reviews of interventions. West Sussex: John Wiley & Sons Ltd 2008; . |
| 23. | Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, Carpenter J, Rücker G, Harbord RM, Schmid CH. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. [PubMed] |
| 24. | Jackson D, White IR, Riley RD. Quantifying the impact of between-study heterogeneity in multivariate meta-analyses. Stat Med. 2012;31:3805-3820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 393] [Cited by in RCA: 448] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 25. | Drogset JO, Grøntvedt T. Anterior cruciate ligament reconstruction with and without a ligament augmentation device : results at 8-Year follow-up. Am J Sports Med. 2002;30:851-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 65] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 26. | Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40:1985-1992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 158] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 27. | Kato Y, Ingham SJ, Kramer S, Smolinski P, Saito A, Fu FH. Effect of tunnel position for anatomic single-bundle ACL reconstruction on knee biomechanics in a porcine model. Knee Surg Sports Traumatol Arthrosc. 2010;18:2-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 102] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 28. | Kato Y, Maeyama A, Lertwanich P, Wang JH, Ingham SJ, Kramer S, Martins CQ, Smolinski P, Fu FH. Biomechanical comparison of different graft positions for single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:816-823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 92] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 29. | Araujo PH, Asai S, Pinto M, Protta T, Middleton K, Linde-Rosen M, Irrgang J, Smolinski P, Fu FH. ACL Graft Position Affects in Situ Graft Force Following ACL Reconstruction. J Bone Joint Surg Am. 2015;97:1767-1773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 30. | van Eck CF, Schreiber VM, Mejia HA, Samuelsson K, van Dijk CN, Karlsson J, Fu FH. “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy. 2010;26:S2-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 127] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 31. | van Eck CF, Schkrohowsky JG, Working ZM, Irrgang JJ, Fu FH. Prospective analysis of failure rate and predictors of failure after anatomic anterior cruciate ligament reconstruction with allograft. Am J Sports Med. 2012;40:800-807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 158] [Article Influence: 12.2] [Reference Citation Analysis (0)] |