Published online Jul 18, 2017. doi: 10.5312/wjo.v8.i7.602
Peer-review started: October 23, 2016
First decision: February 17, 2017
Revised: February 28, 2017
Accepted: April 18, 2017
Article in press: April 20, 2017
Published online: July 18, 2017
Processing time: 263 Days and 8.3 Hours
A 75-year-old man presented with knee pain due to medial osteoarthritis of the knee in the orthopedic outpatient clinic. Conservative treatment was started with steroid infiltration. Besides his knee complaint reported a bilateral painless swollen calf muscle without traumatic cause, and also without any pain at night, fever or medical illness. On physical examination the soleus muscle had a swollen aspect in both calfs. The skin appeared normal without deformities and the arterial pulsations were intact. An X-ray did not show abnormalities in the tibia. Magnetic resonance imaging of the legs revealed bilateral multiple saccular intramuscular venous malformations involving the soleus muscle. Intramuscular venous malformations in skeletal muscles are rare, especially when the occurrence is bilateral. Bilateral venous malformations have the potential to be missed because of the intramuscular localization. Symptoms of intramuscular venous malformation can be often mild and overlap with non-exercise related compartment syndrome, claudication, lymphedema and post thrombotic syndrome or muscle strains.
Core tip: Intramuscular venous malformations involving in the skeletal muscles are rare, especially when occurrence of these lesions is bilateral. These lesions are easily missed due to intramuscular localization. We report a rare presentation of these lesions arising from the soleus muscle on both sides in a 75-year-old man, diagnosed with magnetic resonance imaging of the legs. When the lesions are asymptomatic conservative treatment is preferred. When the appearance is symptomatic surgical resection or sclerotherapy can be an option.
- Citation: Piekaar RSM, Zwitser EW, Hedeman Joosten PPA, Jansen JA. Painless swollen calf muscles of a 75-year-old patient caused by bilateral venous malformations. World J Orthop 2017; 8(7): 602-605
- URL: https://www.wjgnet.com/2218-5836/full/v8/i7/602.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i7.602
A vascular malformation is an aberrant morphogenetic type of blood or lymphatic vessel. The origin of vascular malformations is an abnormal embryonic development of the vascular build-up after the endothelial stage. The malformation consists of an arteriovenous, capillary, venous or lymphatic type. Also combined structures are described[1]. This subdivision is based on the type of vessel involvement. When a lymphatic vessel is involved the anomaly is called a lymphangioma. Abnormal connections between arteries and veins will lead arteriovenous shunting with a cluster of vessels, the nidus. The most common shown type of vascular malformation is the venous malformation. These are mostly situated in the skin and subcutaneous tissues and are present at birth, although clinical manifestation will usually become apparent later in life[2,3]. Intramuscular venous malformations on the other hand are rare especially when the occurrence is bilateral, and these have the potential to be missed because of the intramuscular localization[1,2]. In this report we have described a patient with bilateral extensive intramuscular venous malformations involving the soleus muscles with an asymptomatic presentation.
A 75-year-old man was seen in our orthopedic outpatient clinic with osteoarthritis of the right knee. He experienced morning stiffness, pain on the medial side of his right knee after walking and he had difficulties with full flexion of his knee. Conservative treatment was started with steroid infiltration, 4 cc lidocaine mixed with 1 cc depomedrol. Besides these complaints the patient reported a bilateral painless swollen calf muscle. The patient had noticed these swellings of the calf muscle a few years ago without any traumatic history. He had no pain at night and no fever or medical illness. The past medical history of the patient was uneventful.
On physical examination the soleus muscle was swollen on both sides. The swelling was localized on the right leg over the whole soleus muscle, 10 by 3 cm. On the left lower leg the swelling was about 3 by 3 cm over the medial part of the soleus muscle. A dimpling in both legs (right more than left) at the medial calf area was seen while standing (Figure 1). There was full strength in all lower leg muscles and the reflexes were normal on examination. The rest of the examination was unremarkable, the overlying skin appeared normal without deformities, erythema or warmth and the arterial pulsations were intact. Laboratory test results did not show any abnormalities. An X-ray did not show any bony irregularities in the tibia.
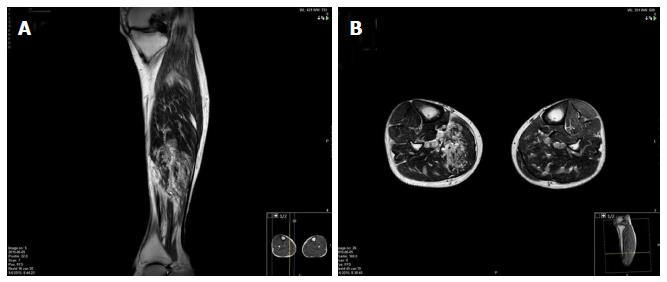
Magnetic resonance imaging (MRI) of the legs revealed bilateral multiple saccular intramuscular venous malformations involving the soleus muscle (Figure 2). There was no nidus seen on MRI so an arteriovenous form of the malformation was not plausible. Due to its asymptomatic presentation no angiogram or ultrasonography was performed to further specify the lesion. After consultation of the vascular surgeon we did not perform surgical resection or focal sclerotherapy because of the asymptomatic nature of the lesions. After explanation of the possible muscle damage from resection and because of the fact that our patient had no disabilities in daily living, we agreed upon conservative management. At three mo follow up the swollen calf muscles were still asymptomatic and examination did not show any change of the venous malformations. We continued the conservative treatment focused on the osteoarthritis of the knee with good result.
Vascular anomalies are common in the general population, and the major of vascular malformations occur in the upper and lower extremities. The origin of the development of vascular malformations lies in an abnormal embryonic root thus they are present at birth, although not always evident[1]. The precise pathogenesis is still though. These anomalies exist of an arteriovenous, capillary, venous and lymphatic type. Also combined structures are described[1]. Venous malformations are a type of vascular malformations that is seen more often by changes in skin color and focal edema[3]. These are mostly the malformations situated in the skin and subcutaneous tissues[2]. As an uncommon cause of tumor the venous malformation can also occur in skeletal muscles of the lower extremities. Asymptomatic intramuscular venous malformations are rare, especially when the occurrence is bilateral[1,2]. The venous malformations we presented in our patient had a bilateral appearance in both calf muscles, the soleus muscle, although the left lower extremity was less severe in comparison with the right side.
Intramuscular venous malformations can provoke contractures of the involved muscles[4,5]. A study by Hein et al[3] shows that most of the intramuscular venous malformations are noted in youth and remain manifest during lifetime. Symptoms of intramuscular venous malformation can be often mild and overlap with non-exercise related compartment syndrome, claudication, post thrombotic syndrome or muscle strain. Other possible diagnosis of swollen lower extremities can be lymphedema with or without hyperkeratosis and papillomatosis[6]. Besides this other vascular anomalies such as arteriovenous or lymphatic malformations can fit in the differential diagnosis of these swellings.
To determine the nature of the vascular malformation MRI is the most accurate tool and it is superior to the other modalities such as ultrasound. On MRI, venous malformations have a T1-hypointense or T1-isointense signal with a T2-hypernintese signal[3]. In this case there were no nidi or connections between arteries and veins visible on the MRI so arteriovenous malformations were not plausible. The lymphatic system was shown without any abnormalities.
Surgical treatment for venous malformations is mostly not necessary and conservative therapy is preferred. Pain, bleeding due to lesions of the skin or cosmetic issues can make treatment indicated though after failure of nonoperative management. When the appearance is intramuscular, venous malformations can result in painful contractures of the involved muscles. In these cases operative treatment can be necessary. The main operative treatment is surgical resection or sclerotherapy (percutaneous embolization). Percutaneous approach is the recommended treatment due to the minor connections to the normal venous system[7]. This kind of treatment often required for larger extensive intramuscular lesions was not indicated in this instance. If sclerotherapy is impossible due to the extent or location more invasive therapy by performing excision of the lesion is possible. If surgical resection is planned it is important to visualize hidden deep truncular anomalies previously to the operation. Otherwise surgery can result in large defects with venous insufficiency and cosmetic deformities as undesirable results. The patient in our case had neither symptoms nor disabilities in daily living as a result of the intramuscular venous malformations whereby conservative treatment, focused on the osteoarthritis of the knee was chosen.
Previously some case indicated focal lesions in the muscle were presented by toe walking and a case reported the presence of extensive intramuscular venous malformation in the lower extremity as well[4,5,8]. But, to our knowledge, a bilateral form of these intramuscular venous malformations in the soleus muscles was never reported before.
Venous malformations are the most common type of vascular anomalies. Although an asymptomatic tumor of the lower extremity can have many causes, a painless swollen calf muscle can be caused by the presence of intramuscular venous malformations. Bilateral asymptomatic appearances of these intramuscular venous malformations are rare and have the potential to be missed because of the intramuscular localization. The intramuscular localization is easily found by using MRI. Treatment is only necessary when the swelling is symptomatic.
Learning points: (1) intramuscular venous malformations in the skeletal muscles are rare, especially when the occurrence is bilateral; (2) bilateral venous malformations have the potential to be missed because of the intramuscular localization; (3) symptoms of intramuscular venous malformation can be often mild and overlap with non-exercise related compartment syndrome, claudication, post thrombotic syndrome or muscle strain; and (4) in this case we have reported a bilateral venous malformation manifestation in calf muscles.
A 75-year-old man with osteoarthritis of the knee presented with asymptomatic bilateral painless swollen calf muscles, which were firstly noticed a few years ago without any previous traumatic cause.
Bilateral painless swollen soleus muscles, with a dimpling (right more than left) while standing.
Non-exercise related compartment syndrome, muscle strain, claudication, lymphangioma, lymphedema, post-thrombotic syndrome or other vascular anomalies such as arteriovenous or lymphatic malformations.
All laboratory test results were within the normal limits.
X-ray of the both legs did not show abnormalities in the bones. Magnetic resonance imaging of both legs revealed bilateral multiple saccular intramuscular venous malformations involving the musculus soleus, nidus of the arteries and the veins in an arteriovenous form of the malformation were not found.
Biopsy was not performed so pathological findings could not be given.
Because of asymptomatic appearances of the bilateral swollen calf muscles conservative treatment was started in our case. Main treatment for symptomatic venous malformations is surgical resection or sclerotherapy (percutaneous embolization).
The precise etiopathogenesis of vascular malformations is still unclear, but the origin of the development lies in an abnormal embryonic root. Venous malformations are frequently shown and are simply diagnosed when situated in the skin or in the subcutaneous tissues. Uncommon localizations of these entities are those in the skeletal muscles. Bilateral appearances of venous intramuscular malformations in the lower extremities are commonly confused with other causes of tumor in the legs.
Asymptomatic bilateral intramuscular venous malformation is a rare type of vascular anomalies of which the origin lies in an abnormal embryonic development.
Bilateral intramuscular venous malformations in the skeletal muscles are rare, with mild symptoms, and have the potential to be missed because of the intramuscular localization.
A straightforward, simple case report with a reasonable review of the literature. The interest is from the differential diagnosis and the concomitant other pathology of knee arthritis.
Manuscript source: Invited manuscript
Country of origin: The Netherlands
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Bruce M, Rothschild Anand A, Hammad Malik S- Editor: Kong JX L- Editor: A E- Editor: Wu HL
| 1. | Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69:412-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Villavicencio JL, Scultetus A, Lee BB. Congenital vascular malformations: when and how to treat them. Semin Vasc Surg. 2002;15:65-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Hein KD, Mulliken JB, Kozakewich HP, Upton J, Burrows PE. Venous malformations of skeletal muscle. Plast Reconstr Surg. 2002;110:1625-1635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 148] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Domb BG, Khanna AJ, Mitchell SE, Frassica FJ. Toe-walking attributable to venous malformation of the calf muscle. Clin Orthop Relat Res. 2004;420:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 5. | Babiker MO, Yeo TH, Goodwin S. A venous malformation presenting as toe walking. Pediatr Neurol. 2015;52:133-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Warren AG, Brorson H, Borud LJ, Slavin SA. Lymphedema: a comprehensive review. Ann Plast Surg. 2007;59:464-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 445] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 7. | Steiner F, FitzJohn T, Tan ST. Surgical treatment for venous malformation. J Plast Reconstr Aesthet Surg. 2013;66:1741-1749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Jung HC, Kim DH, Park BK, Park MK. Extensive intramuscular venous malformation in the lower extremity. Ann Rehabil Med. 2012;36:893-896. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |