Published online Jul 18, 2017. doi: 10.5312/wjo.v8.i7.588
Peer-review started: January 29, 2017
First decision: May 11, 2017
Revised: May 28, 2017
Accepted: June 12, 2017
Article in press: June 13, 2017
Published online: July 18, 2017
Processing time: 170 Days and 12.7 Hours
To systematically review the results of studies looking at autologous matrix-induced chondrogenesis (AMIC) in humans.
A literature search was performed, adhering to the PRISMA guidelines, to review any studies using such techniques in humans. Our initial search retrieved 297 articles listed on MEDLINE, Google Scholar, CINHal and EMBASE. From these studies, 15 studies meeting the eligibility criteria were selected and formed the basis of our systematic review.
The study designs, surgical techniques and outcome measures varied between the studies. Although all studies reported improvements in patient outcome measures, this was not necessarily correlated with magnetic resonance imaging findings. Although there were many additional procedures performed, when AMIC was performed in isolation, the results tended to peak at 24 mo before declining.
Although short-term studies suggest improved patient reported outcomes with a variety of scaffolds, surgical techniques and rehabilitation regimes, the literature remains equivocal on whether the defect size and location, and patient factors affect the outcome. Patient benefit appears to be maintained in the short-to-medium term but more high level studies with extensive and robust validated outcome measures should be conducted to evaluate the medium- and long-term effect of the AMIC procedure.
Core tip: Studies looking at autologous matrix-induced chondrogenesis (AMIC) in humans suggest improved patient reported outcomes in the short-to-medium term but there is significant variation in the scaffolds, surgical techniques and rehabilitation regimes used. The literature remains equivocal on whether the defect size and location, and patient factors affect the outcome. More high level studies with extensive and robust validated outcome measures should be conducted to evaluate the medium- and long-term effect of the AMIC procedure.
- Citation: Shaikh N, Seah MKT, Khan WS. Systematic review on the use of autologous matrix-induced chondrogenesis for the repair of articular cartilage defects in patients. World J Orthop 2017; 8(7): 588-601
- URL: https://www.wjgnet.com/2218-5836/full/v8/i7/588.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i7.588
Cartilage defects have a limited capacity for repair[1,2]. Untreated focal defects have the potential to progress to more generalised lesions and can cause significant morbidity. The frequent outcome for arthritis in large joints such as the knee is surgical intervention for joint replacement. This procedure is generally successful in older sedentary patients, but the limited lifetimes of prostheses make it much less desirable for younger and develop new strategies for the treatment of focal cartilage defects to prevent secondary osteoarthritis.
Various surgical procedures have been implemented to reduce pain, and postpone or prevent the need for joint replacement, while simultaneously withstanding the daily activities of the patient[3]. These include the use of bone marrow stimulation techniques pioneered by Pridie by introducing the concept of subchondral drillingPridie[4,5]. This was further developed by Steadman who introduced the notion of microfracture[6]. A range of chondrocyte implantation techniques have also developed including autologous chondrocyte implantation (ACI), matrix-induced autologous chondrocyte implantation (MACI), mosaicplasty and osteochondral autologous transplantation (OATS)[7-10].
In 2003 after funding issues were raised for two-step procedures such as ACI and MACI partly in view of associated costs, a new one-step procedure was introduced for the repair of cartilage defects called autologous matrix-induced chondrogenesis (AMIC) that brings together microfracture with a collagen matrix scaffold[11]. There is increasing interest in AMIC as it provides a cost-effective alternative to cell-based therapies for articular cartilage repair, and it is highly autologous in nature. Benthien and Behrens[1] first described the AMIC procedure using an awl to perform perforations in the subchondral bone, and “partial autologous fibrin glue” (PAF) using commercially available fibrin glue to adhere Chondro-Gide® (Geistlich Biomaterials, Wolhausen, Switzerland) collagen membrane to the lesion. The TGFβ component of fibrin may contribute to the chondrogenic differentiation of mesenchymal stem cells (MSCs)[10]. Since then the procedure has been described with variations in the drilling technique, scaffold and fixation.
The results with AMIC in the literature have been variable. As there are limited studies on AMIC, variability in the type of scaffold used[12-15], the surgical procedure[1,13,15-17], defect size and location, and patient variability may all contribute to variable results. In addition, we are not aware of the longevity of these results. We performed a systematic review of the literature identifying studies looking at AMIC to determine their clinical outcome, and address these three questions: (1) does the type of scaffold, surgical technique or rehabilitation regime affect outcome? (2) does the defect size and location, and patient factors affect outcome? and (3) does the outcome change with time?
A systematic review of the published literature was conducted following Preferred Reporting Items for Systematic Reviews and Meta-Analysis Guidelines[18]. This search was completed on November 30, 2016 using search databases MEDLINE, Google Scholar, Cumulative Index to Nursing and Allied Health Literature, AMED and EMBASE. No restrictions regarding publication date were applied during the literature search, due to the relatively new nature of AMIC and the limited number of related articles that have been published. Keywords used in the search include “autologous matrix-induced chondrogenesis” and “AMIC”. The Cochrane library was also searched using the terms “autologous matrix-induced chondrogenesis” and “AMIC”. Abstracts of the selected articles were reviewed to ensure they met the selection criteria, after which the full article was obtained. The bibliographies and in-text references of the retrieved articles were searched for any articles that may have been missed during the initial search. Unpublished or grey literature was identified using databases including System for Information on Grey Literature in Europe, the National Technical Information Service, the National Research Register (United Kingdom), UKCRN Portfolio Database, the National Technical Information Service, the British Library’s Integrated Catalogue, and Current Controlled Trials database. Published and unpublished material including university theses and dissertations, and conference proceedings in the English literature were also reviewed.
The inclusion criteria were clinical studies in English language looking at outcomes after AMIC in partial- and full-thickness focal chondral or osteochondral defects (ICRS grade III or IV) of any joint. Studies with a level of evidence I-IV as described by the Oxford Centre for Evidence-based Medicine[19] were included. Studies not meeting these criteria, single-patient case studies, techniques, comments, letters, editorials, protocols and guidelines were excluded. Animal and cadaveric studies were also excluded.
The titles and abstracts of all citations were reviewed by the three authors (Shaikh N, Seah MKT and Khan WS). Full manuscripts of citations adhering to the inclusion criteria and those that were uncertain were downloaded. Reference lists of all full manuscripts and applicable review articles were reviewed to identify any further articles omitted from the initial search. The same investigators then reviewed all full manuscripts against the inclusion criteria and any disagreement on eligibility was resolved by discussion. The corresponding author of the paper was contacted if any queries arose. They were also consulted as to any additional citations that may address the research question.
Data was extracted from papers that satisfied the eligibility criteria. The variables that were determined for each study were study type, treatment period, study size, gender, mean age, patients lost to follow-up, mean and range of follow-up, joint involved, size, grade and location of lesion, inclusion and exclusion criteria, source of funding, surgical technique, previous and associated surgeries, rehabilitation and outcome scores. The extracted data was entered onto Microsoft Excel (Microsoft Corporation, Washington, DC) by one investigator (Shaikh N), and re-evaluated and verified by the other authors (Seah MKT and Khan WS). The investigators were blinded to the source or authors of the identified papers. Although the systematic review protocol was approved by the host institution, the systematic review protocol was not formally registered in a registry. A systematic review was performed rather than a meta-analysis in view of the lack of randomised controlled trials and consistent outcome measures, where the results could be combined to allow statistical analyses.
The Coleman Methodology Score (CMS)[20] was used to evaluate the quality of the studies and to determine if the outcomes and claims made in particular studies should be given more weighting than others. The ratings were also used as a guide to assess the level of confidence from which conclusions could be drawn from a particular study. CMS consists of two parts; Part A that focuses on the design of the study and Part B that relates to the study outcomes. This instrument uses a scaling system, in which the studies are assessed using 10 criteria. Part A has a maximum total score of 65, while Part B has a maximum total score of 35, giving a total score of 100. The total score can be graded as being excellent (85-100 points), good (70-84 points), fair (55-69 points) and poor (< 55 points). A higher total score suggests that the study has an efficient design and is better at avoiding the effects of chance, various biases and confounding factors. The categories used in the CMS were formed on the basis of the Consolidated Standards of Reporting Trials statement for randomized controlled trials[21].
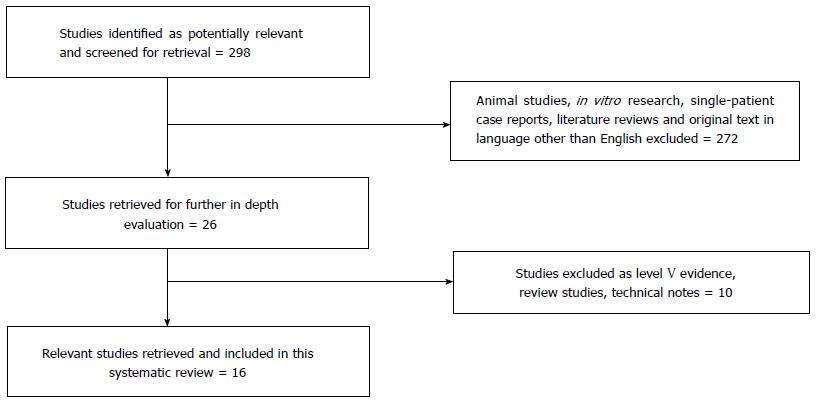
The results of the search using the databases retrieved 297 articles. Twenty-six articles were reviewed after excluding animal and pre-clinical studies, single-patient case reports, literature reviews and articles where the original text was in a language other than English. Of the 26 articles obtained, 10 were excluded as they represented level V evidence, review studies or technical notes, resulting in a total of 16 articles that were included in this systematic review (Figure 1)[3,13,15-17,22-33]. Of the 16 included articles, 13 studies were prospectively conducted, 2 were retrospective, and only 1 was a randomized control trial.
There were more males than females included in the studies, with a ratio of approximately 2:1. The mean age was 36.2 years (range 15-50 years) and the mean follow-up period was 30 mo (range 6-62 mo). Ten of the 16 studies focussed on the knee, 3 on the ankle, and 3 on the hip (Table 1). Some of the studies mentioned sources of funding, but none that would trigger any concerns about conflict of interests or bias. A variety of treatment algorithms were used including different drilling techniques, scaffold used, method of fixation, associated surgery and the rehabilitation protocol (Table 2).
| Ref. | Treatment period | Patient numbers | Mean age (yr) | Mean follow-up in months (range) | Joint | Defect location and type | Grade of lesion | Lesion dimensions (cm2) | Inclusions | Exclusions | Source of funding |
| Shetty et al[34] | 4 yr | 30 | MFC, LFC, trochlea, patella | Grade III/IV | 2-8 | Malalignment of the knee exceeding 5° of valgus or varus. Generalized osteoarthritic changes in the knee | |||||
| Buda et al[15] | Apr 2006-May 2007 | 20 (12M, 8F) | 15-50 | 29 | Knees | Grade III/IV | Not specified | Diffuse arthritis, general medical conditions (e.g., diabetes, rheumatoid arthritis etc.), haematological disorders and infections | None | ||
| Gille et al[26] | 2003-2005 | 27 (16M, 11F) | 39 | 37 (24-62) | Knees | Medial femoral condyle 7, lateral femoral condyle 3, patella 9, trochlea 2, femoral condyle and patella 6 | Grade IV | > 1 | Clinical symptomatic chondral lesions at femoral condyle, patella or trochlea | Advanced osteoarthritis, rheumatic disease, total menisectomy, BMI > 35, deviation of mechanical axis to the affected compartment | Not specified |
| Dhollander et al[16] | Jan 2008-Apr 2008 | 5 (3M, 2F) | 18-50 | 24 (12-24) | Knees | Patella | Grade III/IV | 2 (range 1-3) | Symptomatic focal patella cartilage defects | Untreatable tibiofemoral or patellofemoral malalignment, diffuse osteoarthritis, major meniscal deficiency or other general medical conditions | Not specified |
| Dhollander et al[13] | 2008-2009 | 5 (4M, 1F) | 29.8 | 24 | Knees | Right 2 (40%), left 3 (60%) medial femoral condyle (2), lateral femoral condyle (2), trochlea (1) | Grade III/IV | Median 2.3, range 1.5-5 | 16-40 yr, single symptomatic focal cartilage defect on femoral condyles or patellofemoral joint | Untreated tibiofemoral or patellofemoral malalsignment or instability, diffuse osteoarthritis, bipolar “kissing” lesions, major meniscal deficiency and other general medical conditions | Not specified |
| Kusano et al[22] | Aug 2003-Jul 2006 | 40 (23M, 17F) | 35.6 | 28.8 (13-51) | Knees | Full thickness chondral defect in patella (20), femoral condyle (9), osteochondral defect in femoral condyle (11) | Grade III/IV | 3.87 | Defects in other locations, age > 50 yr, skeletally immature | Not specified | |
| Leunig et al[23] | Mar 2009-Dec 2010 | 6 (5M, 1F) | 22.7 | Not specified (12-30) | Hips | Femoral head 5, acetabular 1 chondral 1, osteochondral 5 | Grade III/IV | > 2 | Full thickness chondral lesions > 2 cm2 or osteochondral lesions > 1 cm2 with defects in weight-bearing areas of acetabulum or femoral head, irreparable by osteotomy in age < 35 yr | Patients unwilling or unable to comply with post-operative rehabilitation protocols. Systematic inflammatory arthritis, advanced arthritis involving both femur and acetabulum, or age > 35 yr | Not specified |
| Pascarella et al[24] | 2006-2008 | 19 (12M, 7F) | 12-36 | Knees | Right knee: Femoral condyle (medial 34%, lateral 14%), patella (9%) Left knee: Femoral condyle (medial 29%, lateral 14%) | Grade III/IV | 3.6 | Age 18-50 yr with single lesion | Osteoarthritis, axial deviations, ligamentous injuries, complete meniscal resection, allergy to collagen membrane components | Not specified | |
| Anders et al[3] | Jan 2004-Mar 2010 | 38 (Not specified) | 37 | 19 (6-24) | Knees | Grade III/IV | 3.4 | Age 18-50 yr, 1-2 lesions | > 2 defects, corresponding defects, bilateral defects, signs of osetoarthritis, other general diseases, history of complete menisectomy, mosaicplasty, treatment with cartilage specific medication, chondropathia patallae or patellar dysplasia | None | |
| Gille et al[28] | Not specified | 57 (38M, 19F) | 37.3 | 24 | Knees | Medial condyle (32), lateral condyle (6), trochlea (4), patella (15) Grouping based on lesion size: Group A 0-3 cm2, Group B 3-6 cm2, Group C 6-9 cm2 | Grade III (35), Grade IV (37) | 3.4 (1-12) | Age 17-61 yr | Rheumatic disease, total meniscectomy, and revision surgery | Not specified |
| Valderrabano et al[17] | 26 (18M, 8F) | 33 | 31 (25-54) | Ankles | Osteochondral lesions of talus | 1.68 | First time osteochondral lesion or failure of previous lesion | Age > 55 yr, open ankle physis | Not specified | ||
| Wiewiorski et al[25] | 2008-2010 | 23 (16M, 7F) | 34 | 23 (11-49) | Ankles (talus) | Osteochondral lesions of talus | Osteochondral | 1.49 | Single lesion with history of ankle trauma | Not specified | |
| Dhollander et al[29] | April 2009-May 2011 | 10 (8M, 2F) | 37.2 ± 7.1 | 24 | Knee | Patella (8), trochlea (2) | Grade III/IV | 4.2 ± 1.9 | Patients aged 18-50 yr with a focal patellofemoral defect and clinical symptoms (pain, swelling, locking, giving way) | Untreatable tibio-femoral or patellofemoral mal - alignment or instability, diffuse osteoarthritis or bipolar “kissing” lesions, major meniscal deficiency and other general medical conditions (diabetes, rheumatoid arthritis) | Not specified |
| Mancini et al[30] | November 2004-June 2007 | 31 | 36.4 ± 10.3 | 60 | Hip | Acetabular chondral defects | Grade III/IV | 2-4 | Patients 18-50 yr of age with acetabular chondral lesions with radiological Tönnis degree < 2 followed up to 5 yr | Concomitant chondral femoral head kissing lesion, systemic rheumatoid diseases, dysplasia, femoral neck axial deviations, coxa profunda, protrusio acetabuli | Not specified |
| Fontana et al[31] | November 2004-March 2011 | 55 | 39.1 (18 to 55) | 36-60 | Hip | Acetabular ± femoral head chondral defects | Grade III/IV | 2-8 | Patients 18-55 years of age with acetabular ± femoral head chondral lesions with radiological Tönnis degree < 2 followed up for 3-5 yr | Rheumatoid arthritis, dysplasia, axial deviation of the femoral neck, coxa profunda, protrusio acetabuli | Not specified but Girolamo is a paid consultant for Geistlich |
| Kubosch et al[32] | Not specified | 17 | 38.8 ± 15.7 | 39.5 ± 18.4 | Ankle | Osteochondral lesions of talus | Grade III/IV | 2.4 ± 1.6 | First-time diagnosis or failure of a previous operative treatment | Arthritis of the ankle joint, kissing lesions and rheumatoid arthritis | Not specified |
| Ref. | Drilling technique | Scaffold/fixation | Associated surgery | Joint | Rehab |
| Buda et al[15] | No drilling | Hyalofast + PRP | 3 osteotomy | Knees | NWB 4 wk, run 6 mo, RTS 12 mo |
| Gille et al[26] | Awl/sharp cannula | ChondroGide Fibrin glue | 2 realignments, 1 capsular shift | Knees | Immobilization 1 wk, passive motion 6 wk, NWB 6 wk |
| Dhollander et al[16] | Microdrill | ChondroGide + PRP Sutures | 3 osteotomy + 1 medial patello-femoral ligament reconstruction | Knees | NWB 2 wk, brace 0-90 for 4 wk, full ROM at 8 wk, Low impact sports 12 mo |
| Dhollander et al[13] | Microdrill | Chondrotissue Pin | 1 osteotomy | Knees | NWB 2 wk, 0-90o 4 wk, full range 8 wk, RTS 12 mo |
| Kusano et al[22] | Awl | ChondroGide Suture/fibrin glue | 28 osteotomy | Knees | PWB 6 wk, 0-60 4wk |
| Leunig et al[23] | Kirchner wire | ChondroGide, fibrin glue | 3 osteoplasty, 2 femoral neck lengthening, drilling of acetabular defects | Hips | PWB 6-8 wk, passive motion 6-8 h for 6-8 wk |
| Pascarella et al[24] | Kirchner wire | ChondroGide Fibrin glue | Knees | ||
| Anders et al[3] | Awl | ChondroGide Suture/fibrin glue | Knees | PWB and lymphatic draining massage 3-6 wk, FWB at 4-6 mo, RTS 3-18 mo | |
| Gille et al[28] | Awl | ChondroGide Fibrin glue | 2 patella realignments, 3 corrective osteotomies, 6 partial menisectomies, 1 ACL reconstruction | Knees | |
| Valderrabano et al[17] | Microdrill | ChondroGide Fibrin glue | 16 osteotomy | Ankles | PWB, ROM of < 200 passive motion machine, lymphatic drainage massage 6wks, FWB 6-12 wk, Light sports 12 wk, RTS 5-6 mo |
| Wiewiorski et al[25] | Microdrill | ChondroGide Fibrin glue | Ankles (talus) | PWB and lymphatic draining massage 6 wk, FWB 12 wk | |
| Dhollander et al[29] | Slow speed 1.2 mm diameter | ChondroGide Vicryl 6/0 | No | Knees (Patellofemoral joint) | NWB for 2 wk, FWB at 10 wk, full range of motion at 8 wk, low impact sports 12 mo |
| Mancini et al[30] | Awl/sharp cannula | ChondroGide Fibrin glue | All patients had cam-type and/or pincer-type impingement, and underwent arthroscopic femoral head-neck resection arthroplasty and/or arthroscopic acetabular rim trimming and labral reattachment to the acetabular rim with suture anchors | Hips | PWB (30% of body weight) for 4 wk, impact sports 3 mo, complete RTS 6 mo |
| Fontana et al[31] | Awl/sharp cannula | ChondroGide Fibrin glue | All patients had cam-type and/or pincer-type impingement, and underwent arthroscopic femoral head-neck resection arthroplasty and/or arthroscopic acetabular rim trimming and labral reattachment to the acetabular rim with suture anchors | Hips | PWB for 7 wk, light sporting activities 4 wk, low impact sports 6 mo, complete RTS 12 mo |
| Kubosch et al[32] | Not specified | ChondroGide Fibrin glue | All patients also underwent autologous cancellous bone grafting to the site | Ankles (talus) | Ankle immobilisation for 2 wk, PWB for 6 wk |
| Shetty et al[34] | Microdrill | Tiseel Coltrix (atelocollagen) | - | Knees | PWB for 6 wk, gradual increase to FWB by next 6 wk |
All of the studies adopted at least one form of established patient-reported outcome measure and 9 of the 16 studies obtained patient Magnetic resonance Observation of CArtilage Repair Tissue (MOCART) scores (Tables 3 and 4). For the 10 studies looking at the knee, all reported more than one clinical outcome measure. Five used the Visual Analogue Scale (VAS), 4 used the Lysholm score and the Knee injury and Osteoarthritis Outcome Score (KOOS), 3 used the International Knee Documentation Committee (IKDC) score, 2 used the International Cartilage Repair Society (ICRS) and the Cincinnati score, and 1 used the Tegner score and Kujala patellofemoral score. The three studies looking at the ankle joint used the American Orthopaedic Foot and Ankle Society (AOFAS) score and the VAS. One study also reported the Foot Function Index (FFI). Two of the hip studies reported the modified Harris Hip Score (mHHS). Four knee, four ankle and one hip studies also reported on MOCART scores. Although positive patient-reported outcomes were observed in all studies, MOCART scores did not always correlate with the patient-reported outcomes.
| Ref. | Sub-groupings (Where Applicable) | Follow-up (mo) | Outcomes | |||||||||||||
| KOOS | IKDC | VAS | ICRS | Cincinnati | Lysholm | Other | ||||||||||
| Pre-surgery | At follow-up | Pre-surgery | At mean follow-up | Pre-surgery | At mean follow-up | Pre-surgery | At mean follow-up | Pre-surgery | At mean follow-up | Pre-surgery | At mean follow-up | Pre-surgery | At mean follow-up | |||
| Buda et al[15] | 29 ± 4.1 | 47.1 ± 14.9 | 93.3 ± 6.8 | 32.9 ± 14.2 | 90.4 ± 9.2 | |||||||||||
| Gille et al[26] | 48 | 31 ± 15 | 37 ± 4 | 46 ± 18 | 37 ± 9 | 36 ± 21 | 47 ± 22 | |||||||||
| Dhollander et al[16] | 24 | 41.6 | 71.4 | 5.2 | 1.4 | |||||||||||
| Dhollander et al[13] | 24 | 37.6 ± 16.7 | 73.1 ± 25 | 6.1 ± 2.4 | 1.9 ± 3.4 | |||||||||||
| Kusano et al[22] | ocF | 28.8 ± 1.5 | 44 ± 25 | 88 ± 9 | 6 ± 3 | 1 ± 1 | 50 ± 25 | 94 ± 8 | ||||||||
| cP | 28.8 ± 1.5 | 51 ± 25 | 74 ± 17 | 6 ± 2 | 2 ± 2 | 58 ± 17 | 85 ± 13 | |||||||||
| cF | 28.8 ± 1.5 | 45 ± 26 | 68 ± 14 | 6 ± 3 | 3 ± 3 | 56 ± 25 | 76 ± 18 | |||||||||
| Leunig et al[23] | Not specified | |||||||||||||||
| Pascarella et al[24] | 24 | 30 | 83 | 54 | 98 | |||||||||||
| Anders et al[3] | MFx | 24 | 54 ± 21 | 19 ± 17 | 40 ± 9 | 83 ± 8 | ||||||||||
| Sutured AMIC | 24 | 46 ± 19 | 14 ± 13 | 43 ± 16 | 88 ± 9 | |||||||||||
| Glued AMIC | 24 | 48 ± 20 | 16 ± 13 | 48 ± 15 | 85 ± 18 | |||||||||||
| Gille et al[28] | 24 | 7 ± 1.8 | 2 ± 2.1 | 50.1 ± 19.6 | 85.2 ± 18.4 | |||||||||||
| Valderrabano et al[17] | 31 | 5 ± 2 | 2 ± 2 | 62.2 ± 15.8 (AOFAS) | 89.2 ± 12.3 (AOFAS) | |||||||||||
| Wiewiorski et al[25] | 23 | 4.8 ± 1.6 | 1.3 ± 2 | 60.6 ± 15.5 (AOFAS) | 90.9 ± 11.4 (AOFAS) | |||||||||||
| Dhollander et al[29] | 24 | 44.5 ± 17.5 | 65.0 ± 23.3 | 73.9 ± 20.8 | 39.4 ± 28.8 | 1.5 ± 1.4 (Tegner) | 2.5 ± 1.5 (Tegner) | |||||||||
| 41.9 ± 15.1 (Kujala) | 59.8 ± 21.2 (Kujala) | |||||||||||||||
| Mancini et al[30] | 60 | 44.9 ± 5.9 (mHHS) | 84 ± 5.9 (mHHS) | |||||||||||||
| Fontana et al[31] | Defect < 4 cm2 | 60 | 44.7 (34-60) (mHHS) | Improvements demonstrated on graoh but not quantified | ||||||||||||
| Defect > 4 cm2 | 60 | 44.7 (34-60) (mHHS) | ||||||||||||||
| Kubosch et al[32] | 39.5 ± 18.4 | 7.8 ± 2.1 | 3.2 ± 2.4 | 82.6 ± 3.4 (AOFAS) 33.7% ± 23.8 (FFI) 52.7 ± 15.9 (MOCART) | ||||||||||||
| Shetty et al[34] | 48 | 64.7 | 88.2 | 39 | 78.6 | 50.8 | 80.4 | |||||||||
| Number and percentage of patients that achieved a particular result for each category of the MOCART scoring system | |||||||||||||||||
| Scoring measure | Outcome | Buda et al[15] | Dhollander et al[16] | Dhollander et al[13] | Kusano et al[22] | Leunig et al[23] | Valderrabano et al[17] | Wiewiorski et al[25] | Dhollander et al[29] | ||||||||
| No. of Pts. | % of Pts. | No. of Pts. | % of Pts. | No. of Pts. | % of Pts. | No. of Pts. | No. of Pts. | No. of Pts. | % of Pts. | No. of Pts. | % of Pts. | No. of Pts. | % of Pts. | No. of Pts. | % of Pts. | ||
| Degree of defect repair | Complete | 14 | 70% | 0 | 0% | 1 | 20% | 3 | 19% | 4 | 100% | 9 | 35% | 8 | 35% | 2 | 20% |
| Hypertrophy | 4 | 20% | 2 | 40% | 2 | 40% | 3 | 19% | 0 | 0% | 13 | 50% | 12 | 52% | 2 | 20% | |
| Incomplete | 2 | 10% | 3 | 60% | 2 | 40% | 10 | 63% | 0 | 0% | 4 | 15% | 3 | 13% | 6 | 60% | |
| Integration to the Surrounding Cartilage | Complete | 16 | 80% | 4 | 80% | 1 | 20% | 8 | 50% | 4 | 100% | 9 | 35% | 8 | 35% | 4 | 40% |
| Incomplete | 2 | 10% | 0 | 0% | 4 | 80% | 4 | 25% | 0 | 0% | 9 | 35% | 0 | 0% | 2 | 20% | |
| Defect visible | 2 | 10% | 1 | 20% | 0 | 0% | 4 | 25% | 0 | 0% | 8 | 31% | 15 | 65% | 4 | 40% | |
| Surface of the Repaired tissue | Intact | 14 | 70% | 0 | 0% | 1 | 20% | 2 | 13% | 3 | 75% | 17 | 65% | 15 | 65% | 3 | 30% |
| Damaged | 6 | 30% | 5 | 100% | 4 | 80% | 14 | 88% | 1 | 25% | 9 | 35% | 8 | 35% | 7 | 70% | |
| Structure of the Repaired tissue | Homogeneous | 6 | 30% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 25% | 7 | 27% | 6 | 26% | 4 | 40% |
| Inhomogeneous | 14 | 70% | 5 | 100% | 5 | 100% | 16 | 100% | 3 | 75% | 19 | 73% | 17 | 74% | 6 | 60% | |
| Signal Intensity DPFSE | Isointense | 13 | 65% | 0 | 0% | 2 | 40% | 1 | 6% | 2 | 50% | 4 | 15% | 3 | 13% | 1 | 10% |
| Hyperintense | 7 | 35% | 5 | 100% | 2 | 40% | 15 | 94% | 1 | 25% | 18 | 69% | 17 | 74% | 6 | 60% | |
| Hypointense | 0 | 0% | 0 | 0% | 1 | 20% | 0 | 0% | 1 | 25% | 4 | 15% | 3 | 13% | 3 | 30% | |
| Subchondral lamina | Intact | 6 | 30% | 0 | 0% | 0 | 0% | 3 | 19% | 1 | 25% | 9 | 35% | 8 | 35% | 0 | 0% |
| Not intact | 14 | 70% | 5 | 100% | 5 | 100% | 13 | 81% | 3 | 75% | 17 | 65% | 15 | 65% | 10 | 100% | |
| Subchondral bone | Intact | 6 | 30% | 0 | 0% | 1 | 20% | 4 | 25% | 2 | 50% | 3 | 12% | 3 | 13% | 6 | 60% |
| Not intact | 14 | 70% | 5 | 100% | 4 | 80% | 12 | 75% | 2 | 50% | 23 | 88% | 20 | 87% | 4 | 40% | |
| Adhesions | No | 20 | 100% | 5 | 100% | 5 | 100% | 15 | 94% | 3 | 75% | 26 | 100% | 23 | 100% | 10 | 100% |
| Yes | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 6% | 1 | 25% | 0 | 0% | 0 | 0% | 0 | 0% | |
| Effusion | No | 17 | 85% | 5 | 100% | 3 | 60% | 6 | 38% | 4 | 100% | 25 | 96% | 22 | 96% | 7 | 70% |
| Yes | 3 | 15% | 0 | 0% | 2 | 40% | 10 | 63% | 0 | 0% | 1 | 4% | 1 | 4% | 3 | 30% | |
Kusano et al[22] found significant improvements in the IKDC and Lysholm scores, but the MOCART scores did not correlate with the positive clinical outcomes. The majority of patients displayed incomplete defect repair, damaged repair tissue, and inhomogeneous repair tissue structure, as well as subchondral lamina and subchondral bone that were not intact. The randomized control trial by Anders et al[3] assessed differences between a microfracture technique, a sutured AMIC technique, and a glued AMIC technique. In all three groups, positive patient outcomes and pain levels were observed at follow-up, with no significant differences between the groups. In assessing the magnetic resonance imaging (MRI) outcomes of patients in this study, results showed good defect filling in most patients, however homogenous repair tissue was only seen in 50% of the patients treated using the AMIC techniques, compared to 100% of the patients treated using traditional microfracture. Additionally, surface regeneration and integration of the lesion with the cartilage proved to be marginally inferior in patients that were treated using AMIC. The finding that MRI scores do not always correspond with patient-assessed outcomes is consistent with those observed in other studies. Dhollander et al[29] found favourable clinical outcome scores in patients undergoing AMIC at the patellofemoral joint but the radiological findings did not support these outcomes. All 10 patients had subchondral lamina changes on MRI and 3 had osteophytes within 24 mo.
There are three commercially available biodegradable membrane scaffolds that fill in the lesions until they are absorbed and replaced by repair tissue (Table 2). The three scaffolds are Chondro-Gide®, Chondrotissue® (BioTissue, Zurich, Switzerland) and Hyalofast™ (Fidia Advanced Biopolymers, Padua, Italy). Chondro-Gide® is a porcine-based membrane that is the original and most popular scaffold used in AMIC. This protein-based matrix has a bi-layer structure composed primarily of type I/III collagen. In cases where the AMIC Plus technique[16] was implemented, a Platelet-rich plasma (PRP) gel (GPS® III System Advantages, Biomet) was applied to the surface of the lesion prior to the application of the membrane. Chondrotissue® is “sponge-like” matrix composed of polyglycolic acid treated with hyaluronan[12,13]. In cases where Chondrotissue® was used, PAF was substituted with biodegradable pins[13]. The HyalofastTM membrane is a partially-synthetic by-product of hyaluronic acid composed of an unstructured amalgamation of fibres. On degradation it releases hyaluronic acid into the defect site that may encourage chondrogenic differentiation of bone marrow-derived MSCs[14]. Prior to commencing the AMIC procedure, bone marrow is aspirated from the iliac crest, and processed to obtain bone-marrow derived MSCs. This is used with autologous PRP obtained from the blood sample, and together the HyalofastTM membrane is immersed in this solution prior to being applied onto defect[15]. Buda et al[15] performed the AMIC procedure on 20 patients using HyalofastTM membrane, and the improvements in the IKDC scores were greater than those seen with Chondro-Gide® membrane. The mean KOOS score at follow-up in this study were significantly greater than those reported by Dhollander et al[16,29] using Chondro-Gide® and in Dhollander et al[13] using Chondrotissue. The clinical outcomes achieved in Buda et al[15]’s study were partly supported by the MOCART scores, with a majority of patients displaying complete defect repair, complete integration to surrounding cartilage, intact repair tissue surface, and isointense signal intensity, while other MRI measures showed poor results despite positive patient-assessed outcomes. The remainder of the studies in this review used Chondro-Gide® and resulted in patient outcomes that were positive and comparable.
Several drilling techniques were adopted in the studies. In 6 of the 16 studies, an awl was used to perforate the subchondral surface of the bone as originally described[1]. Seven studies substituted an awl with a microdrill, with or without Kirchner wires[23,24]. Pascarella[24] carried out a slightly modified AMIC procedure with the intention of increasing the number of MSCs to produce healthy regenerative cartilage. Perforations were performed rather than microfractures, and the covering of the focus of the lesion with a biological collagen patch enriched with bone marrow blood drawn through the knee itself. The aim of the study was simply to show that the modified AMIC procedure was a viable alternative to current surgical practices. The IKDC and Lysholm scores showed a similar trend to that observed by Kusano et al[22], with the mean IKDC score increasing from 30 to 83 in 24 mo, and the mean Lysholm score increasing from 54 to 98. MRI scores showed a significant reduction of the defect area, although detailed MRI evaluations were not available. Similarly Valderrabano[17] introduced a modified AMIC procedure that involved the addition of spongiosa bone harvested from the iliac crest to increase the number of MSCs being recruited. This graft is inserted into the lesion and the membrane placed on top. They reported significant improvement in the mean AOFAS scores from 62 to 89 for 26 patients. MRI findings however showed that only 35% of participants displayed complete filling of the defect, and less than half of the participants returned to their previous level of activity. There were also slight variations depending on the region that needed to be operated upon. The study by Anders et al[3] assessed differences in efficacy and safety between a microfracture technique, a sutured AMIC technique, and a glued AMIC technique. Although the sutured AMIC group showed the greatest improvement in mean Cincinnati scores, there were no significant differences between the groups.
In more than half of the studies, additional surgery was required on at least one subject in the study. The most common additional procedure required was osteotomy and bony realignment. All patients who underwent AMIC at the hip joint underwent additional surgery, mostly for impingement. In the study carried out by Kusano et al[22] looking at the knee joint, patients treated with AMIC alone were compared with patients who had an associated procedure such as an osteotomy. No significant differences in outcomes were noted.
Post-operative rehabilitation regimes varied for the various studies, and were influenced by the location and extent of the lesion. Three studies[3,17,25] included lymphatic drainage massage as part of their rehabilitation process. The post-operative regime generally involved a period of reduced weight-bearing that may include immobilisation of the joint, followed by a periodic increase in weight-bearing and range of motion. Full-weight bearing commenced from 6 wk to 6 mo. Return to sports periods also lacked consistency, with subjects being able to return to sports after as little as 12 wk[17], and as much as 18 mo[3].
For all of the studies investigated, the AMIC procedure was carried out on subjects that had either grade III or grade IV type lesions, although the three ankle-based studies[17,25] did not specify the grade of lesions. The studies focussed on both osteochondral and chondral defects of the joints. Although the lesions varied from 1-8 cm2, the mean lesion size for all studies ranged from 1.5-3.6 cm2. In the ankle based studies all AMIC procedures were conducted on the talus, and a majority of the knee based studies involved the AMIC procedure being carried out on the femoral condyle.
Kusano et al[22] compared 40 defects; 11 were Osteochondral Femoral Condyle lesions (ocF), 20 were Chondral Patella lesions (cP), and nine were Chondral Femoral Condyle lesions (cF). The ocF group had the lowest mean age at 25.9, while the mean age for the other groups was just below 40. Only 36% of patients in the ocF group had an osteotomy compared with 90% in the cP group and 67% in the cF group. The cF group had a significantly smaller mean lesion size (2.3 cm2), compared with 4.2 and 4.4 cm2 in the other groups. The patient outcome scores were consistent across the groups. Although the cP group reported the highest mean pre-operative scores, the ocF group showed the greatest improvement at follow-up, and the cF group showed the least improvement. As there were inconsistencies between the three groups relating to age and size of lesion, it is difficult to draw a definitive conclusion from these results. Gille et al[26] followed up patients for 48 mo and failed to identify any significant effect of lesion size on Patient outcome scores. They did however find that outcomes were better for femoral condyle defects than patella defects, and the two patients who had cartilage defects greater than 8 cm2 did not benefit from the procedure. Fontana et al[31] compared AMIC with microfracture at the hip joint in patients undergoing impingement surgery, and only found a better five-year clinical outcome for the AMIC group for lesions greater than 4 cm2.
Interestingly Fontana et al[31] only found the five-year results to be better for the AMIC group in males, and not females. Looking at the remaining studies, males generally reported higher outcome scores but showed similar levels of improvement to females after treatment. In the study carried out by Kusano et al[22], the results suggested that younger patients generally experience greater improvements than older patients. Gille et al[26] reported on patient outcome scores at 48 months, and failed to identify any significant effect of age, weight, gender, and previous surgery on patient outcome, but younger patients did generally display better recovery rates than older patients.
Mancini et al[30] and Fontana et al[31] reported five-year follow-up in patients undergoing AMIC at the hip joint but all patients underwent additional impingement surgery. The authors report improved outcome scores that were achieved at six months and generally maintained till final follow-up at five-years. Gille et al[26] reported on ICRS, Cincinnati, and Lysholm patient-assessed scores at 24, 36, and 48 mo for patients undergoing AMIC at the knee joint with less than 10% of patients undergoing additional procedures. Patient recovery tended to peak at 24 mo before declining. The mean Cincinnati score peaked at 74 at 24 mo, and steadily declined to 62 (36 mo) and 37 (48 mo). For all scoring systems, the patient outcomes deteriorated more rapidly once they passed the 36 mo follow-up. The randomized control trial by Anders et al[3] compared a microfracture technique, a sutured AMIC technique, and a glued AMIC technique. None of the patients underwent any additional procedures. In all three groups, improvements in pain scores and patient outcomes, including Cincinnati scores, were observed at both 12 and 24 mo follow-up. Between 12 and 24 mo follow-up, 12 patients showed further improvement in Cincinnati scores, 12 showed little or no change, and 3 showed a decline.
CMS was used to assess the methodological quality of the studies carried out using the AMIC procedure (Tables 5 and 6). The mean CMS and standard deviation (SD) achieved was 60.7 ± 7.9 (range 49-75) out of 100. The mean CMS and standard deviation (SD) achieved in Part A was 31.8 ± 5.9, and in Part B was 28.9 ± 4.1.
| Ref. | Coleman methodology score | ||||||||||||||||
| Part A, maximum = 65 | Part B, maximum = 35 | Total, max = 100 | |||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 1 | 2 | 3 | |||||||||
| Buda et al[15] | 0 | 4 | 0 | 10 | 10 | 5 | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 64 |
| Gille et al[26] | 4 | 4 | 7 | 10 | 10 | 5 | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 75 |
| Dhollander et al[16] | 0 | 4 | 10 | 10 | 10 | 5 | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 0 | 5 | 5 | 67 |
| Dhollander et al[13] | 0 | 4 | 10 | 10 | 10 | 5 | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 74 |
| Kusano et al[22] | 4 | 4 | 10 | 0 | 10 | 5 | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 3 | 5 | 5 | 64 |
| Leunig et al[23] | 0 | 4 | 10 | 0 | 10 | 5 | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 0 | 5 | 0 | 56 |
| Pascarella et al[24] | 0 | 4 | 10 | 10 | 0 | 5 | 0 | 2 | 3 | 0 | 5 | 0 | 3 | 0 | 5 | 5 | 52 |
| Anders et al[3] | 4 | 0 | 0 | 10 | 10 | 5 | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 0 | 5 | 0 | 52 |
| Gille et al[28] | 7 | 4 | 10 | 0 | 0 | 0 | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 0 | 5 | 5 | 49 |
| Valderrabano et al[17] | 0 | 4 | 10 | 10 | 10 | 5 | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 0 | 5 | 5 | 67 |
| Wiewiorski et al[25] | 0 | 4 | 10 | 10 | 10 | 0 | 2 | 2 | 3 | 0 | 0 | 0 | 3 | 3 | 5 | 5 | 57 |
| Dhollander et al[29] | 0 | 4 | 10 | 0 | 10 | 5 | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 3 | 5 | 5 | 60 |
| Mancini et al[30] | 4 | 7 | 0 | 10 | 5 | 5 | 2 | 2 | 3 | 0 | 5 | 0 | 3 | 3 | 5 | 5 | 59 |
| Fontana et al[31] | 7 | 7 | 0 | 10 | 5 | 5 | 2 | 2 | 3 | 0 | 5 | 0 | 3 | 3 | 5 | 5 | 62 |
| Kubosch et al[32] | 0 | 7 | 10 | 0 | 0 | 5 | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 3 | 5 | 5 | 53 |
| Shetty et al[34] | 4 | 7 | 10 | 0 | 0 | 5 | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 3 | 5 | 0 | 52 |
| Section score (maximum) | Mean | Range | SD |
| Part A (65) | |||
| Study size | 2.1 | 0-7 | 2.6 |
| Minimum follow-up | 4.5 | 0-7 | 1.7 |
| Number of different surgical treatment included | 7.3 | 0-10 | 4.3 |
| Study design | 6.3 | 0-10 | 4.8 |
| Description of surgical technique | 6.9 | 0-10 | 4.3 |
| Post-Op management described | 4.4 | 0-5 | 1.7 |
| Total part A | 31.4 | 21-40 | 5.7 |
| Part B (35) | |||
| Outcome measures clearly defined | 1.9 | 0-2 | 0.5 |
| Timing of outcome clearly stated | 2 | 2 | 0 |
| Use of reliable outcome criteria | 3 | 3 | 0 |
| General health measure inc. | 2.2 | 0-3 | 1.3 |
| Subjects recruited | 4.7 | 0-5 | 1.2 |
| Inv. independent of surgeon | 1 | 0-4 | 1.7 |
| Written assessment | 3 | 3 | 0 |
| Completion of assessment by patients with minimal investigator assistance | 1.9 | 0-3 | 1.5 |
| Selection criteria reported and unbiased | 5 | 5 | 0 |
| Recruitment rate reported | 4.1 | 0-5 | 2 |
| Total part B | 28.9 | 23-35 | 3.9 |
| Total, maximum = 100 | 60.2 | 49-75 | 7.7 |
AMIC enables the transplantation of a scaffold with MSCs in one step, avoiding the need for laboratory cell number expansion and a second procedure[26]. In our review, 15 studies between 2003 and 2015 that used AMIC for the repair of articular cartilage defects in patients were systematically reviewed. AMIC is still a relatively new procedure and more mid-term and long-term outcomes are awaited. The mean CMS suggesting that the overall quality of the studies was fair. Studies scored poorly for number of patients, length of follow-up, study design and independence of the investigator and the surgeon. For Part A, the overall mean CMS was 31.8 out of 65 points (49%), whereas for Part B the overall mean CMS was 28.9 out of 35 (72%). This indicates that overall, the studies were more competent in defining their outcome criteria and procedures, and that greater improvements need to be made regarding study design and procedures. Although blinding of participants has ethical implications, blinding of clinicians recording the outcome measures was not practised commonly. In scoring systems that require completion by an investigator, it is recommended that the investigation be carried out by an independent investigator to ensure accurate responses from the patient avoiding risk of bias through patient-investigator relationships. Several authors contributed to multiple studies included in this review introducing a risk of bias in both study design and reporting of outcomes across the studies.
The studies included in this review were not directly comparable due to differences in study design, lesions, surgical technique, follow-up and outcome measures. Although the AOFAS score was used in all three ankle studies and the mHHS in two of the three hip studies, there were no consistent scoring systems used for the knee studies. Nevertheless, a pattern of positive patient outcomes can be seen across all of the studies. Future studies should incorporate a universal method of rating patient outcomes for each joint location, allowing direct comparison of results. There also is a need to determine whether MRI assessment is a reliable tool as the studies in our review suggest that it does not necessarily correspond with patient outcome measures. Nevertheless, we recommend that all studies should continue to carry out an MRI assessment while further evidence on its relevance is sought.
Many of the studies included patients that required additional surgical procedures including osteotomies. For a patient undergoing more than one surgical procedure it would be difficult to determine the effect of each procedure in relieving pain and improving joint function. There is a distinct lack of consensus regarding post-operative management and the structure of rehabilitation programmes. Rehabilitation programs can have a significant influence on patient outcomes and recovery rates. Although it is difficult to develop a universal rehabilitation program due to the large number of variables such as patient demographics, and lesion size and location, this needs to be considered when comparing outcomes between different studies. Due to the variation in studies it is not possible to determine if the type of scaffold, surgical technique or rehabilitation regime affect the outcome.
Limited studies suggest that femoral condyle lesions do better than patellar lesions, and osteochondral defects do better than chondral lesions. Defect sizes did not generally have an effect on the patient’s outcome unless the defect was > 8 cm2, in which case it had a detrimental effect on outcomes. There is limited evidence that younger patients experience greater improvements than older patients and display better recovery rates. It has been shown in vitro that bone marrow stem cells from older patients have reduced chondrogenic potential compared with younger patients, potentially decreasing the effectiveness of AMIC in older patient groups.
Follow-up period is an important factor in assessing the real effectiveness and reliability of the AMIC procedure. Since the treatment method is relatively new, there is a lack of long-term patient outcome data available. A longer follow-up period allows the proper assessment of long term outcomes for a procedure. Although five-year follow-up was available for two studies[30,31], the patients had all undergone additional procedures making any improvements difficult to attribute to the AMIC procedure alone. It was demonstrated in the study conducted by Gille et al[26] and Gudas, Gudas et al[27] that declines in clinical outcomes can be observed as early as 18 to 24 mo after undergoing surgical treatment without additional procedures. Patient assessed outcomes by Gille et al[26] declined significantly between the 24 mo and 48 mo post-operative period, indicating that there may be concerns regarding durability of the repaired cartilage after undergoing the AMIC procedure. In the randomized control trial by Anders et al[3] improvements in pain scores and patient outcomes, including Cincinnati scores, were observed at 12 mo follow-up. Between 12 and 24 mo follow-up, although 12 patients showed further improvement in Cincinnati scores, 12 showed little or no change, and 3 showed a decline. This supports the observation by other studies, and their 5-year follow-up results are awaited.
The published literature reviewed suggests that AMIC in cartilage repair is a safe and effective treatment option that improves patient outcome measures and reduces pain. MRI findings however do not necessarily correspond with patient outcome measures. Most studies reported promising results, with no mention of further surgical corrections being needed in the follow-up period. Medium- and long-term results for AMIC procedures without additional surgeries are awaited. Earlier studies suggest that AMIC results may peak at around 24 mo.
The CMS results suggest that the clinical trials evaluated in this systematic review were of fair to reasonable quality; with 8 of the 15 studies achieving total CMS scores ranging from 60 to 80. The main weaknesses across the studies were the total number of participants and the patient follow-up periods. Improvements in these areas will significantly increase the reliability of the patient outcome measures, while allowing investigators to draw more definitive conclusions. More high level studies with larger sample sizes, and extensive and robust validated outcome measures should be conducted to evaluate the medium- and long-term effect of the AMIC procedure.
The results with autologous matrix-induced chondrogenesis (AMIC) in the literature have been variable. As there are limited studies on AMIC, variability in the type of scaffold used, the surgical procedure, defect size and location, and patient variability may all contribute to variable results. In addition, we are not aware of the longevity of these results.
AMIC is a one-step procedure that brings together microfracture with a collagen matrix scaffold. There is increasing interest in AMIC as it provides a cost-effective alternative to cell-based therapies for articular cartilage repair, and it is highly autologous in nature.
The published literature reviewed suggests that AMIC in cartilage repair is a safe and effective treatment option that improves patient outcome measures and reduces pain. MRI findings however do not necessarily correspond with patient outcome measures. Most studies reported promising results, with no mention of further surgical corrections being needed in the follow-up period. Medium- and long-term results for AMIC procedures without additional surgeries are awaited.
More high level studies with larger sample sizes, and extensive and robust validated outcome measures should be conducted to evaluate the medium- and long-term effect of the AMIC procedure.
Mesenchymal stem cells (MSCs): These cells reside in bone marrow and many adult tissues. MSCs are multipotent stromal cells capable of self-renewal and differentiation in vitro into a variety of cell lineages, including chondrocytes, osteoblasts, and adipocytes. They are therefore seen as an optimal regenerative cellular therapeutic for musculoskeletal regeneration.
This is a well-designed and written systematic review.
Manuscript source: Invited manuscript
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gheita TA, Zhou S S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Benthien JP, Behrens P. The treatment of chondral and osteochondral defects of the knee with autologous matrix-induced chondrogenesis (AMIC): method description and recent developments. Knee Surg Sports Traumatol Arthrosc. 2011;19:1316-1319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 117] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 2. | Buckwalter JA, Mankin HJ. Articular cartilage: degeneration and osteoarthritis, repair, regeneration, and transplantation. Instr Course Lect. 1998;47:487-504. [PubMed] |
| 3. | Anders S, Volz M, Frick H, Gellissen J. A Randomized, Controlled Trial Comparing Autologous Matrix-Induced Chondrogenesis (AMIC®) to Microfracture: Analysis of 1- and 2-Year Follow-Up Data of 2 Centers. Open Orthop J. 2013;7:133-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 4. | Pridie K. A method of resurfacing osteoarthritic knee joints. J Bone Joint Surg Br. 1959;3:618-619. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Müller B, Kohn D. Indication for and performance of articular cartilage drilling using the Pridie method. Orthopade. 1999;28:4-10. [PubMed] |
| 6. | Steadman JR, Rodkey WG, Briggs KK. Microfracture to treat full-thickness chondral defects: surgical technique, rehabilitation, and outcomes. J Knee Surg. 2002;15:170-176. [PubMed] |
| 7. | Brittberg M. Autologous chondrocyte implantation--technique and long-term follow-up. Injury. 2008;39 Suppl 1:S40-S49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 179] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 8. | Behrens P, Bitter T, Kurz B, Russlies M. Matrix-associated autologous chondrocyte transplantation/implantation (MACT/MACI)--5-year follow-up. Knee. 2006;13:194-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 363] [Cited by in RCA: 330] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 9. | Lahav A, Burks RT, Greis PE, Chapman AW, Ford GM, Fink BP. Clinical outcomes following osteochondral autologous transplantation (OATS). J Knee Surg. 2006;19:169-173. [PubMed] |
| 10. | Gille J, Meisner U, Ehlers EM, Müller A, Russlies M, Behrens P. Migration pattern, morphology and viability of cells suspended in or sealed with fibrin glue: a histomorphologic study. Tissue Cell. 2005;37:339-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Benthien JP, Behrens P. Autologous matrix-induced chondrogenesis (AMIC). A one-step procedure for retropatellar articular resurfacing. Acta Orthop Belg. 2010;76:260-263. [PubMed] |
| 12. | Patrascu JM, Freymann U, Kaps C, Poenaru DV. Repair of a post-traumatic cartilage defect with a cell-free polymer-based cartilage implant: a follow-up at two years by MRI and histological review. J Bone Joint Surg Br. 2010;92:1160-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Dhollander AA, Verdonk PC, Lambrecht S, Almqvist KF, Elewaut D, Verbruggen G, Verdonk R. The combination of microfracture and a cell-free polymer-based implant immersed with autologous serum for cartilage defect coverage. Knee Surg Sports Traumatol Arthrosc. 2012;20:1773-1780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Hegewald AA, Ringe J, Bartel J, Krüger I, Notter M, Barnewitz D, Kaps C, Sittinger M. Hyaluronic acid and autologous synovial fluid induce chondrogenic differentiation of equine mesenchymal stem cells: a preliminary study. Tissue Cell. 2004;36:431-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 129] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 15. | Buda R, Vannini F, Cavallo M, Grigolo B, Cenacchi A, Giannini S. Osteochondral lesions of the knee: a new one-step repair technique with bone-marrow-derived cells. J Bone Joint Surg Am. 2010;92 Suppl 2:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 132] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 16. | Dhollander AA, De Neve F, Almqvist KF, Verdonk R, Lambrecht S, Elewaut D, Verbruggen G, Verdonk PC. Autologous matrix-induced chondrogenesis combined with platelet-rich plasma gel: technical description and a five pilot patients report. Knee Surg Sports Traumatol Arthrosc. 2011;19:536-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 112] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 17. | Valderrabano V, Miska M, Leumann A, Wiewiorski M. Reconstruction of osteochondral lesions of the talus with autologous spongiosa grafts and autologous matrix-induced chondrogenesis. Am J Sports Med. 2013;41:519-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 135] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 18. | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264-29, W64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21613] [Cited by in RCA: 18151] [Article Influence: 1134.4] [Reference Citation Analysis (0)] |
| 19. | Obremskey WT, Pappas N, Attallah-Wasif E, Tornetta P, Bhandari M. Level of evidence in orthopaedic journals. J Bone Joint Surg Am. 2005;87:2632-2638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 201] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 20. | Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2-11. [PubMed] |
| 21. | Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, Gøtzsche PC, Lang T. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med. 2001;134:663-694. [PubMed] |
| 22. | Kusano T, Jakob RP, Gautier E, Magnussen RA, Hoogewoud H, Jacobi M. Treatment of isolated chondral and osteochondral defects in the knee by autologous matrix-induced chondrogenesis (AMIC). Knee Surg Sports Traumatol Arthrosc. 2012;20:2109-2115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 23. | Leunig M, Tibor LM, Naal FD, Ganz R, Steinwachs MR. Surgical technique: Second-generation bone marrow stimulation via surgical dislocation to treat hip cartilage lesions. Clin Orthop Relat Res. 2012;470:3421-3431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Pascarella A, Ciatti R, Pascarella F, Latte C, Di Salvatore MG, Liguori L, Iannella G. Treatment of articular cartilage lesions of the knee joint using a modified AMIC technique. Knee Surg Sports Traumatol Arthrosc. 2010;18:509-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 25. | Wiewiorski M, Miska M, Kretzschmar M, Studler U, Bieri O, Valderrabano V. Delayed gadolinium-enhanced MRI of cartilage of the ankle joint: results after autologous matrix-induced chondrogenesis (AMIC)-aided reconstruction of osteochondral lesions of the talus. Clin Radiol. 2013;68:1031-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 26. | Gille J, Schuseil E, Wimmer J, Gellissen J, Schulz AP, Behrens P. Mid-term results of Autologous Matrix-Induced Chondrogenesis for treatment of focal cartilage defects in the knee. Knee Surg Sports Traumatol Arthrosc. 2010;18:1456-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 224] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 27. | Gudas R, Stankevicius E, Monastyreckiene E, Pranys D, Kalesinskas RJ. Osteochondral autologous transplantation versus microfracture for the treatment of articular cartilage defects in the knee joint in athletes. Knee Surg Sports Traumatol Arthrosc. 2006;14:834-842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 153] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 28. | Gille J, Behrens P, Volpi P, de Girolamo L, Reiss E, Zoch W, Anders S. Outcome of Autologous Matrix Induced Chondrogenesis (AMIC) in cartilage knee surgery: data of the AMIC Registry. Arch Orthop Trauma Surg. 2013;133:87-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 146] [Cited by in RCA: 140] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 29. | Dhollander A, Moens K, Van der Maas J, Verdonk P, Almqvist KF, Victor J. Treatment of patellofemoral cartilage defects in the knee by autologous matrix-induced chondrogenesis (AMIC). Acta Orthop Belg. 2014;80:251-259. [PubMed] |
| 30. | Mancini D, Fontana A. Five-year results of arthroscopic techniques for the treatment of acetabular chondral lesions in femoroacetabular impingement. Int Orthop. 2014;38:2057-2064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 31. | Fontana A, de Girolamo L. Sustained five-year benefit of autologous matrix-induced chondrogenesis for femoral acetabular impingement-induced chondral lesions compared with microfracture treatment. Bone Joint J. 2015;97-B:628-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 32. | Kubosch EJ, Erdle B, Izadpanah K, Kubosch D, Uhl M, Südkamp NP, Niemeyer P. Clinical outcome and T2 assessment following autologous matrix-induced chondrogenesis in osteochondral lesions of the talus. Int Orthop. 2016;40:65-71. [PubMed] |
| 33. | Taichman RS. Blood and bone: two tissues whose fates are intertwined to create the hematopoietic stem-cell niche. Blood. 2005;105:2631-2639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 423] [Cited by in RCA: 385] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 34. | Shetty AA, Kim SJ, Bilagi P, Stelzeneder D. Autologous collagen-induced chondrogenesis: single-stage arthroscopic cartilage repair technique. Orthopedics. 2013;36:e648-e652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |