Published online Jul 18, 2017. doi: 10.5312/wjo.v8.i7.574
Peer-review started: February 12, 2017
First decision: March 28, 2017
Revised: April 3, 2017
Accepted: April 23, 2017
Article in press: April 24, 2017
Published online: July 18, 2017
Processing time: 165 Days and 19.3 Hours
To systemically review all studies reporting return to sport following tibial plateau fracture, in order to provide information on return rates and times to sport, and to assess variations in sporting outcome for different treatment methods.
A systematic search of CINAHAL, Cochrane, EMBASE, Google Scholar, MEDLINE, PEDro, Scopus, SPORTDiscus and Web of Science was performed in January 2017 using the keywords “tibial”, “plateau”, “fractures”, “knee”, “athletes”, “sports”, “non-operative”, “conservative”, “operative”, “return to sport”. All studies which recorded return rates and times to sport following tibial plateau fractures were included.
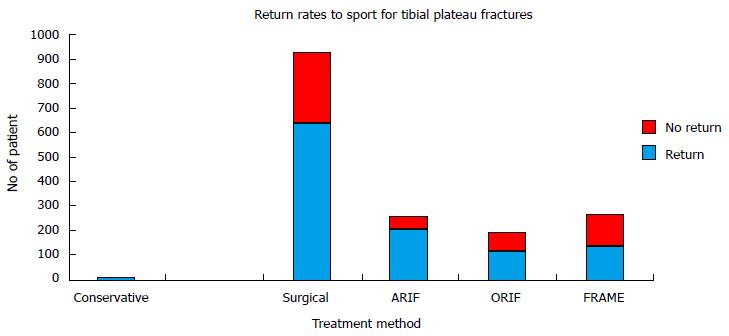
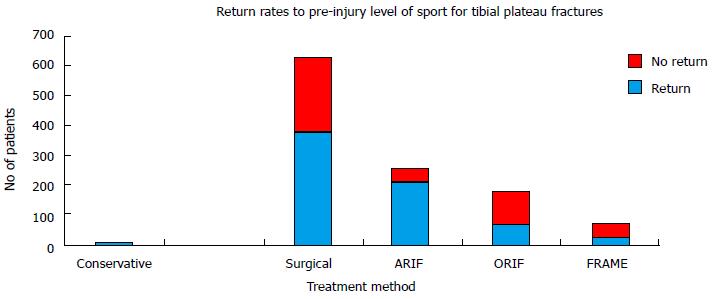
Twenty-seven studies were included: 1 was a randomised controlled trial, 7 were prospective cohort studies, 16 were retrospective cohort studies, 3 were case series. One study reported on the outcome of conservative management (n = 3); 27 reported on the outcome of surgical management (n = 917). Nine studies reported on Open Reduction Internal Fixation (ORIF) (n = 193), 11 on Arthroscopic-Assisted Reduction Internal Fixation (ARIF) (n = 253) and 7 on Frame-Assisted Fixation (FRAME) (n = 262). All studies recorded “return to sport” rates. Only one study recorded a “return to sport” time. The return rate to sport for the total cohort was 70%. For the conservatively-managed fractures, the return rate was 100%. For the surgically-managed fractures, the return rate was 70%. For fractures managed with ORIF, the return rate was 60%. For fractures managed with ARIF, the return rate was 83%. For fractures managed with FRAME was 52%. The return rate for ARIF was found to be significantly greater than that for ORIF (OR 3.22, 95%CI: 2.09-4.97, P < 0.001) and for FRAME (OR 4.33, 95%CI: 2.89-6.50, P < 0.001). No difference was found between the return rates for ORIF and FRAME (OR 1.35, 95%CI: 0.92-1.96, P = 0.122). The recorded return time was 6.9 mo (median), from a study reporting on ORIF.
Return rates to sport for tibial plateau fractures remain limited compared to other fractures. ARIF provides the best return rates. There is limited data regarding return times to sport. Further research is required to determine return times to sport, and to improve return rates to sport, through treatment and rehabilitation optimisation.
Core tip: We performed a systematic review assessing all studies which reported return rates and times to sport following tibial plateau fractures. Twenty-seven studies were included: All recorded return rates; only one study recorded return times. One study reported on conservative treatment; all 27 studies reported on surgical treatment. The surgical techniques comprised Open Reduction Internal Fixation (ORIF), Arthroscopic-Assisted Reduction Internal Fixation (ARIF) and Frame-Assisted Fixation (FRAME). The return rates were: Total Cohort-70%; conservatively-managed cohort-100%; surgically-managed cohort-70%; ORIF-60%, ARIF-83%, FRAME-52%. ARIF provided the best return rates to sport. Data however is limited, particularly for return times to sport. Further research in this area is required.
- Citation: Robertson GAJ, Wong SJ, Wood AM. Return to sport following tibial plateau fractures: A systematic review. World J Orthop 2017; 8(7): 574-587
- URL: https://www.wjgnet.com/2218-5836/full/v8/i7/574.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i7.574
Tibial plateau fractures comprise 1% of all fractures[1,2]; despite their limited frequency, due to their intra-articular nature, they commonly result in significant functional morbidity[2-5]. These fractures involve either the lateral tibial plateau, the medial tibial plateau, or both; injury patterns are commonly classified by the Schatzker or the AO/OTA classification[2-5]. Such injuries normally arise from high energy trauma: The common reported mechanisms include road traffic accidents, falls from a height, pedestrian struck by motor vehicle or high-impact sporting collision[1-5]. Despite sport being a well-documented cause for this injury, there is limited evidence on the predicted return rates and return times to sport following tibial plateau fractures[2,4,5]. This arises for the fact that most outcome studies on this injury type provide validated functional outcomes scores, failing to differentiate specific details on recovery of sporting function[2,4,5].
The treatment of tibial plateau fracture is based on the location and displacement of the fracture[2-5]. All undisplaced fractures are routinely managed non-operatively, with a period of knee immobilisation for 4 to 8 wk in a cast or a brace: This is combined with sequential range of motion exercises and a graduated weightbearing protocol[3]. For displaced fractures, the standard treatment is surgical reduction and fixation of the fracture[2-5]. A number of surgical techniques have been reported in the literature, and the choice of technique is directed by the fracture pattern[2-5]. Techniques can be classified into three categories: Those which involve open reduction and internal fixation of the fracture (ORIF), those which involve arthroscopic-assisted reduction and fixation of the fracture (ARIF), and those which involve frame (external fixation) assisted fixation of the fracture (FRAME)[2-5]. The choice of internal fixation can vary from cannulated screws to multiple locking plates, depending on the nature of the fracture[2-5]. Associated intra-articular injuries, when present, are also commonly treated in conjunction with fracture fixation[2-5]. While there is growing evidence on the clinical and radiological outcomes of such techniques, there remains limited evidence on return to sport following such injuries[2-5].
The aim of this systematic review was to assess all studies reporting return rates and times to sport following treatment for tibial plateau fractures, in order to provide clarification on the optimal treatment methods for this injury, as well as to provide prognostic information on return to sport following these fractures.
A systematic literature search was carried out in January 2017 from the following databases: MEDLINE (PubMed), Cochrane Collaboration Database, EMBASE, SPORTDiscus, CINAHAL, Google Scholar, Physiotherapy Evidence Database (PEDro), Scopus and Web of Science. This was to locate all articles, published in English language, in peer-reviewed journals, reporting on return rates and return times to sports following treatment for tibial plateau fractures. No distinction was made regarding the location or nature of fracture, nor level and type of sports activity performed. The keywords used for the search were “tibial”, “plateau”, “fractures”, “knee”, “athletes”, “sports”, “non-operative”, “conservative”, “operative”, “return to sport”. There was no limit regarding the year of publication.
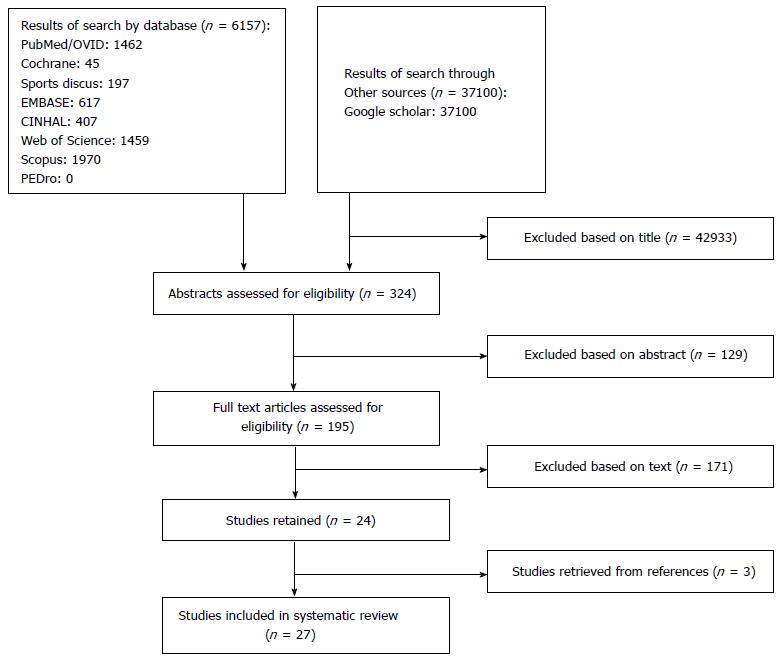
The authors followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines to design the review[6]. The abstract of each publication was independently reviewed by all three authors (Greg AJ Robertson, Seng J Wong and Alexander M Wood) to establish its suitability for inclusion within the review. As per the PRISMA guidelines, the inclusion and exclusion criteria for review are listed in Table 1[6]. The quality of reporting of meta-analyses flow diagram in Figure 1 presents the search results and selection process for the review[6]. Article categories excluded from the review included case reports, expert opinions, literature reviews, instructional courses, biomechanical reports, and technical notes. If exclusion could not be confirmed from the abstract alone, the full-text version of the study was accessed to confirm eligibility. Review of the reference lists of relevant articles were also performed to identify additional studies that could be suitable for inclusion. Discrepancies between the reviewers’ choice of articles for inclusion were resolved by consensus discussion.
| Inclusion criteria | Exclusion criteria |
| Acute tibial plateau fractures | Extra-articular proximal tibial fractures |
| Elite or recreational athletes | Stress fractures of the proximal tibial |
| Return rate to sporting activity reported | No sporting outcome data reported |
| Return time to sporting activity reported | Paediatric fractures (age under 15) |
| Two or more fractures reported | Reviews, case reports, abstracts or anecdotal articles |
| Peer-reviewed journals | Animal, cadaver or in vitro studies |
| English language |
The review database contained data on patient demographics, mode of injury, pre-operative radiological investigations, fracture location, fracture classification, operative and non-operative management techniques, rehabilitation protocols, return rates to sport, return times to sports, rate of fracture union, time to fracture union, complications, required re-interventions and predictive factors for return to sports.
The primary outcome measures were return rates to sport and return times to sport. The secondary outcome measures were return rates to pre-injury level of sport, rate of fracture union, time to fracture union and associated complications. Return to sport was defined as resumption of sporting activities following completion of treatment; return to pre-injury level of sport was defined as the return to specified pre-injury level of sporting activities following completion of treatment. Return time to sport was defined as: The time period from commencement of non-operative modalities to sporting return for conservatively-managed patients; and the time period from primary surgical treatment to sporting return for surgically-managed patients. Where return to sport or fracture union was not possible from the primary treatment method alone, with requirement for conversion to a secondary treatment, this was recorded as a failure for the primary treatment method.
The modified Coleman Methodology Score (CMS) was used to assess the quality of the included papers[7]. This is a 10-point-criteria validated scoring system, which has been previously used in multiple similar systematic reviews[7-10]. The scoring methodology utilised is that presented by Del Buono et al[7]. This provides a final score ranging from 0 to 100, indicating the quality of study included[7]. Two of the authors (Greg AJ Robertson and Alexander M Wood) performed scoring of each of the included studies. Using the intra-class correlation co-efficient statistic, the inter-observer reliability of the scores was noted as 0.91 (95%CI: 0.89-0.93).
Meta-analysis comparisons were performed for return rates to sport between cohorts of the synthesis data of sufficient size. There was insufficient data to perform meta-analysis comparisons on return times to sport. The meta-analysis was performed on RevMan Version 5.3 (The Cochrane Group). Odds ratios (ORs), with a random effects model, were used to assess comparisons between the dichotomous data. The heterogeneity of included studies was analysed with the I2 statistic and was judged to be significant if I2 was > 50%. The significance level was P < 0.05.
The details of the selection process for the included articles are listed in Figure 1. In total, 324 unique abstracts and 195 unique articles were assessed.
We identified 27 relevant publications[11-37], published from 1988[18] to 2016[14], focusing on clinical and functional outcomes of patients who returned to sports activity after tibial plateau fractures (Tables 2-6). One was a randomised controlled trial (RCT)[11], 7 were prospective cohort studies[14,16,25,26,28,30,32], 16 were retrospective cohort studies[12,13,15,17,18,20-24,27,29,34-37] and 3 were case series[19,31,33].
| Ref. | N | Study design | Mean follow-up | Treatment | Mode of injury | Fracture types | Report of IA injuries | IA injury repair | Coleman score | Return rate | Return rate by treatment modality | Return rate to same level of sport | Return time (range) | Rate of union | Time to union (range) |
| Waldrop et al[18] (1988) | 3 | RCS | 59 mo | Knee immobilisation | Falls RTA skiing | Postero-lateral (undisplaced) | Yes | Yes | 69 | 3/3 (100%) | Cons: 3/3 (100%) | 3/3 (100%) | N/A | N/A | N/A |
| Ref. | n | Study design | Mean follow-up | Treatment | Mode ofinjury | Fracture types | Report of IA injuries | IA injury repair | Coleman score | Return rate | Return rate bytreatment modality | Return rate tosame level of sport | Return time (range) | Rate of union | Time tounion (range) |
| Ahearn et al[12] (2014) | 21 | RCS | 40.5 mo | PF (21) | Falls RTA pedestrian | Schatzker VI Bicondylar | No | Not reported | 62 | 14/21 (67%) | PF: 14/21 (67%) | 4/21 (19%) | N/A | 21/21 (100%) | N/A |
| Brunner et al[19] (2009) | 5 | CS | 39 mo | PF (5) | Skiing (4) Falls (1) | Moore type II | Yes | Yes | 61 | 5/5 (100%) | PF: 5/5 (100%) | N/A | N/A | N/A | N/A |
| Canadian Orthopaedic Trauma Society[11] (2006) | 33 | RCT | 24 mo | PF (33) | Falls RTA Pedestrian Sports Work Cycling | Schatzker V and VI | Yes | Yes | 74 | 4/33 (12%) | PF: 4/33 (12%) | 4/33 (12%) | N/A | N/A | N/A |
| Chang et al[16] (2014) | 16 | PCS | 28.7 mo | PF (16) | N/A | Schatzker VI AO/OTA C2-3 | Yes | Yes | 66 | 14/16 (88%) | PF: 14/16 (88%) | 14/16 (88%) | N/A | 16/16 (100%) | 20.2 wk |
| Keogh et al[13] (1992) | 13 | RCS | 17 mo | PSF (13) | RTA (5) Falls (5) Work (2) Sport (1) | Schatzker I-VI | No | Not reported | 45 | 11/13 (85%) | PSF: 11/13 (85%) | N/A | N/A | N/A | N/A |
| Morin et al[14] (2016) | 15 | PCS | 18.2 mo | SF (15) | Skiing (15) | Postero-Medial Moore Type I | Yes | Yes | 73 | 13/15 (87%) | SF: 13/15 (87%) | 0/15 (0%) | N/A | N/A | N/A |
| Stevens et al[17] (2001) | 46 | RCS | 100 mo | PF (46) | RTA (13) Pedestrian (13) Falls (9) Sports (6) Work (2) | Schatzker I-VI | Yes | Yes | 70 | 21/46 (46%) | PF: 21/46 (46%) | 6/46 (13%) | N/A | 46/46 (100%) | N/A |
| van Dreumel et al[15] (2015) | 26 | RCS | 74 mo | SF PF | Falls (57%) RTA (25%) Other (14%) | Schatzker I-VI AO/OTA B1-C3 | No | Not reported | 79 | 15/26 (58%) | SF: N/A PF: N/A | 15/26 (58%) | 6.9 (2-18) mo (median) | N/A | N/A |
| Waldrop et al[18] (1988) | 3 | RCS | 59 mo | PF (6) ORBG (12) | Falls RTA Skiing | Postero-Lateral (displaced) | Yes | Yes | 69 | 18/18 (100%) | PF: 6/6 (100%) ORBG: 12/12 (100%) | 17/18 (100%) | N/A | N/A | N/A |
| Ref. | n | Study design | Mean follow-up | Treatment | Mode of injury | Fracture types | Report of IA injuries | IA injury repair | Coleman score | Return rate | Return rate by treatment modality | Return rate to same level of sport | Return time (range) | Rate of union | Time to union (range) |
| Chan et al[26] (2003) | 18 | PCS | 48 mo | APF (18) | RTA (17) Falls (1) | Schatzker V and VI | Yes | Yes | 68 | 13/18 (72%) | APF: 13/18 (72%) | 13/18 (72%) | N/A | N/A | N/A |
| Chan et al[25] (2008) | 54 | PCS | 87 mo | APF (54) | RTA (50) Falls (4) | Schatzker I-VI | Yes | Yes | 80 | 48/54 (89%) | APF: 48/54 (89%) | 48/54 (89%) | N/A | 54/54 (100%) | N/A |
| Chiu et al[34] (2013) | 25 | RCS | 86 mo | APF (25) | N/A | Schatzker IV-VI | Yes | Yes | 73 | 22/25 (88%) | APF: 22/25 (88%) | 22/25 (88%) | N/A | 25/25 (100%) | N/A |
| Duan et al[29] (2008) | 39 | RCS | 34 mo | APSF (37) | RTA (19) Falls (11) Sports (9) | Schatzker I-V | Yes | Yes | 57 | 30/39 (77%) | APSF: 30/39 (77%) | 30/39 (77%) | N/A | 39/39 (100%) | 12 (11-14) wk |
| Gill et al[28] (2001) | 25 | PCS | 24 mo | APSF (25) | Skiing (25) | Schatzker I-IV | Yes | Yes | 79 | 21/25 (84%) | APSF: 21/25 (84%) | 21/25 (84%) | N/A | N/A | N/A |
| Guanche et al[31] (1993) | 5 | CS | N/A | APSF (5) | N/A | Schatzker I-III | No | Not reported | 55 | 5/5 (100%) | APSF: 5/5 (100%) | 5/5 (100%) | N/A | 5/5 (100%) | N/A |
| Holzach et al[30] (1994) | 15 | PCS | 35.3 mo | APSF (10) | Skiing (15) | AO/OTA B2.2 and B3.1 | Yes | Yes | 76 | 13/15 (87%) | APSF: 13/15 (87%) | 13/15 (87%) | N/A | N/A | N/A |
| Hung et al[32] (2003) | 31 | PCS | 36 mo | APF (31) | RTA (30) Falls (1) | Schatzker I-VI | Yes | Yes | 76 | 26/31 (84%) | APF: 26/31 (84%) | 26/31 (84%) | N/A | 31/31 (100%) | 12 (11-14) wk |
| Itokazu et al[24] (1996) | 16 | RCS | 30 mo | APSF (5) ACF (7) APF (4) | N/A | Hohl II and III | Yes | Yes | 49 | 16/16 (100%) | APSF: 5/5 (100%) ACF: 7/7 (100%) APF: 4/4 (100%) | 16/16 (100%) | N/A | 16/16 (100%) | N/A |
| Kampa et al[27] (2016) | 20 | RCS | 30 mo | APSF (20) | Falls (52%) Sport (48%) | Schatzker I-III | Yes | Yes | 71 | 10/20 (50%) | APSF: 10/20 (50%) | 10/20 (50%) | N/A | 20/20 (100%) | N/A |
| Pizanis et al[33] (2012) | 5 | CS | 24 mo | APF (5) | N/A | AO/OTA B2 and B3 | No | Not reported | 61 | 5/5 (100%) | APF: 5/5 (100%) | 5/5 (100%) | N/A | N/A | N/A |
| Ref. | n | Study design | Mean follow-up | Treatment | Mode of injury | Fracture types | Report of IA injuries | IA injury repair | Coleman score | Return rate | Return rate by treatment modality | Return rate to same level of sport | Return time (range) | Rate of union | Time to union (range) |
| Ahearn et al[12] (2014) | 15 | RCS | 41 mo | Frame and IF (15) Non-Bridging Frames (15) | Falls RTA Pedestrian | Schatzker VI (Bicondylar) | No | Not reported | 62 | 11/15 (73%) | Frame and IF: 11/15 (73%) | 3/15 (20%) | N/A | 15/15 (100%) | N/A |
| Chin et al[20] (2005) | 18 | RCS | 28 mo | Frame and IF (16) Arthro Frame (2) Bridging Frames (3) Non-Bridging Frames (15) | RTA Pedestrian Falls Skiing Cycling | Schatzker V and VI | No | Not reported | 61 | 15/18 (83%) | Frame and IF: N/A Arthro Frame: N/A | 7/18 (39%) | N/A | 15/18 (83%) | 14 (11-22) wk |
| Canadian Orthopaedic Trauma Society[11] (2006) | 33 | RCT | 24 mo | Frame and IF (33) Bridging Frames (4) Non-Bridging Frames (29) | Falls RTA Pedestrian Sports Work Cycling | Schatzker V and VI | Yes | Yes | 74 | 10/33 (30%) | Frame and IF: 10/33 (30%) | 10/33 (30%) | N/A | N/A | N/A |
| Itokazu et al[24] (1996) | 1 | RCS | 30 mo | Arthro Frame (1) Non-Bridging Frame (1) | N/A | Hohl II and III | Yes | Yes | 49 | 1/1 (100%) | Arthro Frame: 1/1 (100%) | 1/1 (100%) | N/A | 1/1 (100%) | N/A |
| Katsenis et al[21] (2005) | 46 | RCS | 38 mo | Frame and IF (46) Bridging Frames (30) Non-Bridging Frames (16) | RTA Falls | Schatzker V and VI AO/OTA C1-3 | Yes | Not reported | 72 | 25/46 (54%) | Frame and IF: 25/46 (54%) | N/A | N/A | 45/46 (98%) | 13.5 (11-18) wk |
| Katsenis et al[22] (2009) | 127 | RCS | 60 mo (minimum) | Frame and IF (127) Bridging and Non-Bridging Frames (127) | RTA (96) Falls (29) Sports (2) | AO/OTA C1-3 | Yes | Not reported | 68 | 68/127 (54%) | Frame and IF: 68/127 (54%) | N/A | N/A | 126/127 (99%) | 13.7 (10-20) wk |
| Weigel et al[23] (2002) | 22 | RCS | 98 mo | Frame and IF (22) Non-Bridging Frames (22) | RTA (16) Fall (3) Pedestrian (2) Assault (1) Sport (1) Crush (1) | Schatzker II, IV, V and VI AO/OTA C1-3 | No | Not reported | 54 | 7/22 (32%) | Frame and IF: 7/22 (32%) | N/A | N/A | N/A | N/A |
| Ref. | n | Study design | Mean follow-up | Treatment | Mode of injury | Fracture types | Report of IA injuries | IA injury repair | Coleman score | Return rate | Return rate by treatment modality | Return rate to same level of sport | Return time (range) | Rate of union | Time to union (range) |
| Kraus et al[36] (2012) | 79 | RCS | 53 mo | PF PSF APSF | Sports (54%) RTA (20%) Falls (18%) | Schatzker I-VI AO/OTA A2-C3 | Yes | Yes | 47 | 65/79 (82%) | ORIF: N/A PSF: N/A APSF: N/A | N/A | N/A | N/A | N/A |
| Loibl et al[37] (2013) | 92 | RCS | 94 mo | PF PSF ARSF | Skiing (92) | AO/OTA B1-C3 | No | Not reported | 55 | 81/92 (88%) | ORIF: N/A PSF: N/A APSF: N/A | 57/92 (62%) | N/A | N/A | N/A |
| Scheerlinck et al[35] (1998) | 38 | RCS | 62 mo | APSF (30) Arthro Frame (2) Arthro Frame and IF (6) | N/A | AO/OTA B1-C3 | Yes | Yes | 68 | 32/38 (84%) | APSF: N/A Arthro Frame: N/A Arthro Frame and IF: N/A | 24/38 (63%) | N/A | N/A | N/A |
Of the 1134 fractures, 613 (54%) occurred in male patients, 428 (38%) in female patients, and 93 (8%) failed to specify gender. Ninety-nine of the fractures were open injuries[11,12,17,20-23]. Two patients had bilateral tibial plateau fractures[22]. Of the 1134 fractures recorded, sport-related follow-up data was available for 920 (81.1%). The mean age at the time of injury ranged from 34.8 years[31] to 52.2 years[37]. The commonly reported modes of injury were road traffic accidents, falls from height, pedestrian struck by motor vehicle and collisions during sports: The most commonly reported sport was skiing (Tables 2-6).
Twenty-six of the twenty-seven studies used formal fracture classifications to describe the fracture types[11-17,19-37]. Six studies used the Schzakter Classification alone to define fracture pattern[17,20,27-29,32]. Five studies used the AO/OTA classification alone[13,22,30,35,37]. Three studies used the Hohl and Moore Classification alone[14,19,24]. Twelve used both the AO/OTA and the Schzakter Classification[11,12,15,16,21,23,25,26,31,33,34,36]. One study reported on postero-lateral tibial plateau fractures with no classification used[18].
The reported fracture configurations from each study are recorded in Tables 2-6. Four studies in the ARIF cohort, restricted patient inclusion to low-energy fracture patterns (Schatzker I-III, AO/OTA A-B)[27,30,31,33]. There were no restriction of fracture types in the ORIF[11-19] and FRAME[11,12,20-24] cohorts. One study reported on undisplaced fractures[18]; all 27 studies reported on displaced fractures[11-37]. Seven studies included open fractures: All used the Gustillo-Anderson Classification to classify the soft tissue damage[11,12,17,20-23].
Twenty-one studies recorded associated injuries[11-14,16-22,24-30,32,34-36]. For twelve studies, the reported injuries comprised solely of intra-articular knee injuries[12,14,16,18,19,28-30,32,34-36]. For six studies, the reported injuries comprised both intra-articular knee injuries and non-knee-related trauma injuries[11,17,21,22,24,25]. For three studies, the reported injuries comprised solely of non-knee-related trauma injuries[13,20,27]. The commonest intra-articular knee injuries were meniscal tears, tibial spine avulsions fractures, anterior cruciate ligament (ACL) ruptures, posterior cruciate ligament ruptures and medial collateral ligament rutpures[11,12,14,16-19,21,22,24,25,28-30,32,34-36]. The non-knee-related trauma injuries comprised head, chest and abdominal traumatic injuries, as well as associated spinal, upper limb and lower limb fractures[11,13,17,20-22,24,25,27].
Of the 920 tibial plateau fractures with follow-up data, 917 were surgically managed[11-37] and 3 were conservatively managed[18]. Of the surgically managed fractures, 193 were treated with ORIF[11-19], 253 were treated ARIF[24-34] and 262 were treated with FRAME[11,12,20-24]. For 209 fractures, the outcome data was reported within combined surgical cohorts, with no differentiation for treatment method used[35-37].
All of the studies used plain radiographs as initial assessment of the fractures[11-37]. Eleven studies reported using a combination of plain radiographs and CT Scans for fracture imaging[14,16,19,20,22,24,25,29,30,32,34]. Four studies, reported using a combination of plain radiographs, CT and MRI Scans for fracture imaging[21,26-28].
The mean CMS for all the studies was 65.5 (range 45-80) (Tables 2-6)[11-37]. For the study reporting on conservative management, the CMS was 69 (Table 2)[18]. For the studies reporting on surgical management, the mean CMS was 65.5 (range 45-80) (Tables 3-6)[11-37]. For the ORIF cohort, the mean CMS was 66.6 (range 45-79) (Table 3)[11-19]. For the ARIF cohort, the mean CMS was 67.7 (range 49-80) (Table 4)[24-34]. For the FRAME cohort, the mean CMS was 62.9 (range 49-74) (Table 5)[11,12,20-24].
Conservative management: This comprised of knee immobilisation for 4 to 8 wk, during which the patient performed quadriceps strengthening exercises[18]. Following this, the patients commenced range of motion exercises, with progressive weightbearing and physiotherapy[18].
Surgical management: The surgical technique could be categorised into three main categories: ORIF, ARIF, FRAME.
For the ORIF cohort, surgical techniques comprised open reduction of the fracture followed by internal fixation[11-19]. Depending on the severity of the fracture, the internal fixation ranged from cannulated screws to locked plate fixation (Table 3). Concomitant management of intra-articular injuries was performed in six studies[11,14,16-19]. Bone graft was used in three studies to augment fixation[11,12,19]; synthetic bone graft substitute was used in one study to augment fixation[16].
For the ARIF cohort, surgical techniques comprised reduction of the fracture under arthroscopic guidance followed by internal fixation[24-34]. Depending on the severity of the fracture, the internal fixation ranged from cannulated screws to locked plate fixation (Table 4). Concomitant management of intra-articular injuries was performed in nine studies[24-30,32,34]. Bone graft was used in six studies to augment fixation[25-27,29,30,32]; synthetic bone graft substitute was used in four studies to augment fixation[27,28,33,34].
For the FRAME cohort, surgical techniques comprised fracture reduction by traction and open intervention, followed by Frame Application[11,12,20-24]. In six studies, limited internal fixation was performed as part of the procedure[11,12,20-23]. In two studies, reduction of the fracture was assisted by arthroscopic visualisation of the fracture[20,24]. Four studies used either bridging or non-bridging frames, with bridging frames reserved for cases with significant knee joint instability[11,20-22]; three studies used non-bridging frame exclusively[12,23,24] (Table 5). Concomitant management of intra-articular injuries was performed in two studies[11,24]. Bone graft was used in three studies to augment fixation[11,12,20]; synthetic bone graft substitute was used in two studies to augment fixation[21,22].
Post-operative rehabilitation regimes were reported by all but one study[11-22,24-37]. These comprised limited weightbearing for 6 to 12 wk[11-22,24-37]. There was a variety of range of motion (ROM) protocols based on the severity of fracture, the surgical technique used and associated injuries: Some studies advocated full ROM exercises immediately post-operative, while other advised knee immobilisation for 4 to 6 wk post-operative[11-22,24-37].
Seventeen of the studies reported concomitant management of intra-articular knee injuries at the time of surgical procedures[11,14,16-19,24-30,32,34-36]. These included meniscal repair, partial and total (medial or lateral) meniscectomy, tibial spine avulsions fixation and ACL re-attachment/repair[11,14,16-19,24-30,32,34-36].
Twenty-six of the studies used validated scoring systems to assess post-intervention functional status[11-30,32-37]. These included both the conservatively managed[18] and surgically-managed patients[11-30,32-37]. The only study not to use a validated scoring systems was in the ARIF cohort[31]. The most commonly used scores were the Rasmussen Score (7 studies)[13,25,26,28,29,33,34], the Lysholm Knee Score (6 studies)[14,19,27,33,36], the Short-Form 36 (SF-36) health status questionnaire (6 studies)[11,12,17,19,20,23] and the Hospital for Special Surgery Knee Score (4 studies)[11,16,32,35].
Conservative management: The return rates for the conservatively-managed tibial plateau fractures are provided in Table 7 and Figure 2.
| Mode of treatment | n (total) | Return rates to sport | Return times to sport | Return rate to pre-injury level | Rates of union | Mean times to union |
| All[11-37] | 920 | 642/920 (70%)[11-37] | 6.9 mo (median)[15] | 374/628 (60%)[11,12,14-18,20,24-35,37] | 475/480 (99%)[12,16,17,20-22,24-27,29,31,34] | 13.6 wk[16,20-22,29,32] |
| Non-surgical[18] | 3 | 3/3 (100%)[18] | N/A | 3/3 (100%)[18] | N/A | N/A |
| Surgical[11-37] | 917 | 639/917 (70%)[11-37] | 6.9 mo (median)[15] | 371/625 (59%)[11,12,14-18,20,24-35,37] | 475/480 (99%)[12,16,17,20-22,24-27,29,31,34] | 13.6 wk[16,20-22,29,32] |
| Surgical | ||||||
| ORIF[11-19] | 193 | 115/193 (60%)[11-19] | 6.9 mo (median)[15] | 60/175 (34%)[11,12,14-18] | 83/83 (100%)[12,16,17] | 20.2 wk[16] |
| ARIF[24-34] | 253 | 209/253 (83%)[24-34] | N/A | 209/253 (83%)[24-34] | 190/190 (100%)[24-27,29,31,34] | 12.0 wk[29,32] |
| FRAME[11,12,20-24] | 262 | 137/262 (52%)[11,12,20-24] | N/A | 21/67 (31%)[11,12,20,24] | 202/207 (98%)[12,20-22,24] | 13.7 wk[20-22] |
| Non-specific surgical cohort[35-37] | 209 | 178/209 (85%)[35-37] | N/A | 81/130 (62%)[35,37] | N/A | N/A |
The return rates to pre-injury level sport for the conservatively-managed tibial plateau fractures are provided in Table 7 and Figure 3.
Surgical management: The return rates for the various methods of surgical management are provided in Table 7 and Figure 2.
On meta-analysis of the synthesis data, the return rates for the ARIF cohort were found to be significant higher than both: The return rates for the ORIF cohort (OR = 3.22, 95%CI: 2.09-4.97, P < 0.001; I2 = N/A); and the return rates for the FRAME cohort (OR 4.33, 95%CI: 2.89-6.50, P < 0.001; I2 = N/A). There was no significant difference between the return rates of the ORIF cohort and the FRAME cohort (OR 1.35, 95%CI: 0.92-1.96, P = 0.122; I2 = 0%, P = 0.40). The return rates to pre-injury level sport for the various methods of surgical management are provided in Table 7 and Figure 3.
On meta-analysis of the synthesis data, the return rates to pre-injury level sport for the ARIF cohort were found to be significant higher than both: The return rates to pre-injury level sport for the ORIF cohort (OR 9.10, 95%CI: 5.80-14.29, P < 0.001; I2 = N/A); and the return rates to pre-injury level sport for the FRAME cohort (OR = 10.40, 95%CI: 5.65-19.15, P < 0.001; I2 = N/A). There was no significant difference between the return rates to pre-injury sport of the ORIF cohort and the FRAME cohort (OR 1.14, 95%CI: 0.63-2.09, P = 0.664; I2 = 3%, P = 0.31).
Conservative management: There were no reported return times for the conservatively-managed tibial plateau fractures (Table 7).
Surgical management: Only one study on the surgically managed fractures reported return times to sport. This was from the ORIF cohort. The reported return time was 6.9 mo (median) with a range of 2 to 18 mo[15]. This represented a return time to full level sport[15].
Conservative management: The study reporting on conservatively-managed fractures, did not record post-treatment fracture union[18].
Surgical management: Fracture union was recorded in 13 studies[12,16,17,20-22,24-27,29,31,34], with all 13 studies recording rates of union[12,16,17,20-22,24-27,29,31,34] and only 6 studies recording times to union[16,20-22,29,32] (Table 7). For those managed by ORIF, the union rate was 100%[12,16,17] and the mean time to union was 20.2 wk[16]. For those managed by ARIF, the union rate was 100%[24-27,29,31,34] and the mean time to union was 12.0 wk[29,32]. For those managed by FRAME, the union rate was 98%[12,20-22,24] and the mean time to union was 13.7 wk[20-22].
Conservative management: For the conservatively-managed tibial plateau fractures, there were no complications reported[18].
Surgical management: For the ORIF cohort, 8 of the studies reported complications[11-13,15-19]: One study reported no complications[14]. The reported complications included wound infection (0%-40%), prominent metalwork (0%-56%), post-operative knee stiffness requiring intervention (0%-8%), nerve-related symptoms (0%-6%), and loss of fixation requiring revision (0%-10%)[11-19]. Removal of metalwork ranged from 0%-56% (mean 27%); re-intervention rate ranged 0%-93% (mean 39%)[11-19].
For the ARIF cohort, nine of the studies reported complications[24-30,32,34]; two studies reported no complications[31,33]. The reported complications included wound infection (0%-7%), prominent metalwork (0%-20%), post-operative knee stiffness requiring intervention (0%-8%), DVT (0%-10%), nerve-related symptoms (0%-20%), loss of fixation requiring revision (0%-3%)[24-34]. Removal of metalwork ranged from 0%-20% (mean 2%) and re-intervention rate ranged 0%-20% (mean 4%)[24-34].
For the FRAME cohort, all studies reported complications[11,12,20-24]. These included pin site infection (0%-57%), nerve-related symptoms (0%-10%), DVT (0%-13%) delayed union (0%-14%) post-treatment knee stiffness requiring intervention (0-5%), and post-treatment mal-alignment requiring intervention (0%-18%)[11,12,20-24]. All cases required frame removal; beyond this, re-intervention rate ranged 0%-35% (mean 14%)[11,12,20-24].
A randomised controlled trial by the Canadian Orthopaedic Trauma Society[11], comparing ORIF to FRAME for Schatzker VI fractures, found that there was a trend towards earlier return to pre-injury sporting activity levels at 6 mo (P = 0.031) and 12 mo (P = 0.024) post-injury for FRAME compared to ORIF. This difference, however, disappeared at 24 mo post-injury (P = 0.128)[11].
These results are in keeping with those from Ahearn et al[12], who found there was no significant long-term difference between FRAME and ORIF, in terms of return to sporting activities, at a mean follow-up of 41 mo.
Loibl et al[37] noted poorer outcomes regarding return to sport for the more severe fracture types (AO/OTA B3 and C3) They also found that participation in downhill skiing post-injury decreased more for patients 61 years and older (56% decline) compared to patients younger than 60 years (45% decline): Post-injury frequency of sports (r = 0.22, P < 0.05) and duration of sports (r = 0.25, P < 0.05) was weakly correlated with the patient’s age at injury[37].
Kraus et al[36] found that, while patients with high-energy fracture patterns (AO/OTA Type C) could continue to participate in sports post-injury, at a frequency and duration similar to those of low-energy fracture patterns (AO/OTA Type A and B) (P = 0.357), the variety of sports they could return to was significantly reduced (P < 0.004). Conversely, however, they found that the presence of a concomitant ligamentous injuries was not associated with a poorer return to sporting activity (P = 0.365)[36].
The main findings of this review are that seventy percent of patients with a tibial plateau fracture returned to sport following injury, with only sixty percent able to return to their pre-injury level of sport. Conservative management offered very acceptable results for undisplaced fractures, with a return to sport rate of 100%. Regarding surgical techniques for displaced fractures, ARIF offered the best return rates at 83%; however, such results were likely influenced by less severe fracture patterns being more amendable to this technique. There was no difference seen in return rates between ORIF and FRAME. There was a significant limitation in the reporting of data with only one studies reporting return times to sport for this fracture type.
In comparison to previous similar systematic reviews, the methodological quality of the studies in this review was improved, with a mean modified CMS of 66[7-10]. In keeping with this, there was one recorded RCT[11]. However, all other included studies comprised Level 2 to 4 evidence[11-37], demonstrating a need for further high quality research in this field to better define the optimal treatment modalities for these injuries.
From our data we found that conservative management offered a good return rates to sport at 100%. Similarly, return rates to previous level of sport were very satisfactory at 100%. However, this was from a cohort of three fractures, on which there were no return times reported[18]: This reflects a significant limitation of data in this area. Despite this, the rate of persisting symptoms and complications following this treatment was 0%[18]. Thus, with the restricted evidence available, conservative management appears to be a very acceptable treatment for undisplaced fractures. Clinicians should, however, remain vigilant for fracture displacement during follow-up: If this is occurs, surgical management should be offered[3].
From our data we found that surgical management offered limited return rates to sport at 70%. Again, the evidence in this area was restricted, with only one study in this cohort reporting return times to sport[15]. Despite such limitations, with the reported median return time of 6.9 mo, it appears that sporting rehabilitation following such injuries is notably prolonged[15]. Despite the restricted reporting on return times to sport, there was sufficient data on return rates to sport to allow comparison between the three main treatment methods: ORIF, ARIF and FRAME. ARIF offered the best return rates at 83%, with a similar value for return to pre-injury level of sport. In comparison, the return rates for ORIF and FRAME were 60% and 52% respectively, and the return rate to pre-injury level of sport were 34% and 31%. The positive findings for ARIF are in keeping with the current literature: A recent systematic review found ARIF to provide encouraging clinical and radiological outcomes from an assessment of 12 studies[2]. It has been suggested that this technique provides the surgeon with a superior assessment of fracture reduction intra-operatively, as well as allowing direct intra-operative assessment and management of concomitant intra-articular knee injuries[2]. Indeed, within our review, 9 of the 11 studies using ARIF, reported associated arthroscopic procedures at time of surgery[24-30,32,34]. However, to note, six of the nine studies in the ORIF cohort also reported associated management of intra-articular injuries, with a number of these studies avoiding arthroscopic-assisted reduction due to the complexity of fractures encountered[11,14,16-19]. It has been noted that the use of arthroscopic-assisted reduction techniques for Schatzker V and VI fractures can significantly prolong operating time, and increase the risk of post-operative infection and compartment syndrome[38]. Certainly, on assessment of the fracture types recorded in the studies of the ARIF cohort, at least four studies restricted the technique to low-energy fracture patterns (Schatzker I-III, AO/OTA Type A and B)[27,30,31,33]. In comparison, there were no such restrictions of fracture types in the ORIF[11-19] and FRAME[11,12,20-24]. cohorts. Thus, it is likely that selection of fracture type had a confounding influence on the results from our review[36,37]. Nevertheless, it appears that, particularly for the lower-energy fracture patterns, ARIF offers athletes the best possibility to return to sport post-treatment.
Other notable findings were that FRAME offered a quicker return to pre-injury sporting levels than ORIF for Schatzker V and VI fractures[11]. This may reflect a lesser insult to the surrounding soft tissue with FRAME compared to ORIF, so enabling a quicker return of function[11]. However, return rates to sport for the two techniques, beyond 2 years follow-up, from two studies, showed no difference[11,12]: Thus it remains debatable if FRAME is truly better than ORIF in allowing return to sport following high energy bicondylar tibial plateau fractures. Further notable findings were that two other studies found that return to sport following tibial plateau fractures was adversely affected by increasing severity of fracture pattern and by advancing age of the patient[36,37]. It would appear that for increasing severity of fracture pattern, with the associated damage to cartilage and surrounding structures, recovery of sporting function in the knee becomes more challenging[36,37]. Such effects are then confounded by increasing age of the patient, through the reduced physiological reserve and reduced healing potential that is often associated with this[36,37].
In comparison to previous studies, there was an improvement in the reporting of both rehabilitation methods and functional outcome scores[7-10]. All but one of the studies reported comprehensive rehabilitation protocols, with the majority providing detailed descriptions of weight-bearing status, immobilisation method and range of motion protocols[11-22,24-37]. Similarly, twenty-six of the twenty-seven studies used formal validated scoring methods to allow assessment of post-treatment function[11-30,32-37].
Assessment of the rehabilitation methods revealed there was notable variation between the techniques. These were largely centred on range of motion protocols and methods of post-operative immobilisation[11-22,24-37]. With the numbers available, it was not possible to assess the effect of variation in rehabilitation methods on return to sport. Appreciably, such variations are guided by the severity of the injury and associated damage to the surrounding ligaments[11-22,24-37]. However, with the considerable variations observed, it appears there is definite ability, within future studies, to assess, refine and optimise rehabilitation techniques.
The most notable finding, in comparison to previous similar reviews[7-10], was the significant lack of reporting on return times to sport. This, in part, reflects the limited description of return to sport in the included studies, with this often being briefly reported a secondary outcome measure[11-37]. However, this also reflects the prolonged rehabilitation associated with such fractures, with return to sport often outdating the standard follow-up duration for these injuries[3,15]. Nevertheless, the restricted reporting on return to sport for these fractures was a significant shortcoming, limiting both inter-study comparisons and collection of certain relevant details such as return to pre-injury level of sport[7-10]. Future studies should aim to provide more comprehensive descriptions of return rates and times to sport, detailing the level of sport to which the athlete returned, as well as the time taken to return to both training and full-level sport.
Firstly, due to the limited reporting in most studies, it was not possible to develop synthesis data for return times to sport for this injury. Given the usefulness of such information for athletes and clinicians alike, future studies should be encouraged to record such information as able.
Similar to this, due to the paucity of reporting in the included studies, it was not possible to analyse the synthesis data for the effect of certain factors such as fracture severity, concomitant injuries, and required re-intervention on sporting return. Given the importance of such data on treatment decisions and final outcome, the generalised data provided can be of limited value for the individual athlete. However, the authors have tried to illustrate such information, where possible, including details on fracture severity, the presence of associated intra-articular injuries and rates of complications and further surgery accordingly.
Thirdly, the reporting of return rates to sport throughout the studies was limited. Few provided comprehensive descriptions, with the majority only providing a brief summary of sporting outcomes. This limits our ability to compare sporting outcome both between studies as well as between treatment modalities. In order to limit this effect, sporting outcome was divided in two distinct categories (return to sport, return to same level of sport), enabling a clear outcome from each study.
Lastly, due to the limited size of certain sub-cohorts within the synthesis data, it was only possible to perform six meta-analysis comparisons: further comparisons between sub-sets of the surgical techniques would have been preferable but unfortunately this was not possible due to sub-cohort size.
In conclusion, thirty percent of all athletes who suffer a tibial plateau fracture may not be able to return to sport post-injury. Conservative management forms the first-line treatment for all undisplaced fractures, and provides good results regarding return to sport. Surgical fixation is reserved for displaced fractures. The choice of surgical technique is guided by the severity and pattern of the fracture. With low-energy fracture patterns, ARIF appears to offers the best possibility of return to previous level of sport. With high-energy fracture patterns, there appears no clear difference between ORIF and FRAME for return rates to sport. There was a significant limitation on reporting of return times to sport following these injuries. Thus, despite the available data, further well-designed research is required to better define return rates and times to sport following tibial plateau fractures.
Tibial plateau fractures account for 1% of all fractures. The main causes for these injuries include road traffic accidents, falls from a height, pedestrian struck by motor vehicle and high-impact sporting collisions. Despite sport being a common cause for this injury, the literature on return rates and return times to sport for this fracture type remains limited. Such data is valuable to sporting medical personnel and sports teams alike, as this can allow optimisation of management and rehabilitations technique for this injury, ensuring optimisation of sporting outcome for the affected athletes.
Despite comprising only 1% of all fractures, tibial plateau fractures represent an injury with significant morbidity, due to the intra-articular nature of the fracture. This is particularly the case for athletes sustaining this injury, as return to sport can be significantly affected. Despite sport being a well-documented cause for this injury, data on return to sport following this fracture remains limited, as most studies present outcome data through combined scoring systems, failing to differentiate sporting outcomes. Given the significant difficulties experienced by athletes planning to return to sport following this injury, accurate information on the return rates and return times to sport for this fracture type, stratified by fracture classification and treatment modality, can allow sporting medical personnel and sports team to appropriately select the optimal treatment modality for each patient and adequately schedule rehabilitation programmes following these injuries. By optimising the treatment and rehabilitation of these injuries, this can ensure that affected athletes achieves the optimal sporting outcome possible.
In this systematic review, the authors identified 27 studies which reported either return rates or return times to sport following tibial plateau fractures: All studies recorded return rates; only one study recorded return times. One study reported on the outcome of conservative-managed fractures; all 27 studies reported on the outcome of surgically-managed fractures. The surgical techniques comprised Open Reduction Internal Fixation (ORIF), Arthroscopic-Assisted Reduction Internal Fixation (ARIF) and Frame-Assisted Fixation (FRAME). The return rates were: Total cohort 70%; Conservatively-Managed cohort 100%; Surgically-Managed cohort 70%. For the different surgical techniques, the return rates were: ORIF cohort 60%, ARIF cohort 83% and FRAME cohort 52%. The recorded return time was 6.9 mo (median), from a study reporting on ORIF. ARIF was more commonly used for lower energy fracture patterns (Schatzker I-III; AO/OTA Type A and B), while ORIF and FRAME were used for all fracture patterns. ARIF provided the best return rates to sport, particularly for the lower energy fracture patterns. Data however is limited, particularly for return times to sport. Further research in this area is required.
A comprehensive understanding of the expected return rates and return times to sport following tibial plateau fractures, stratified by fracture pattern and treatment modality, ensures the treating clinician can appropriately select the optimal method of management, to allow the best possibility of return to sport post-injury. Such information can also allow sports team to realistically plan rehabilitation schedules, with a better understanding of the required treatment duration before athletes will be able return to sport. This allows optimization of both the management and outcome of these injuries.
ARIF: Fixation of a Tibial Plateau Fracture with Internal Fixation and an Arthroscope to ensure accurate articular surface reduction; FRAME: Fixation of a Tibial Plateau Fracture with an External Fixation Device; Non-Bridging Frame: An External Fixation Device which does not bridge across the knee joint; Bridging Frame: An External Fixation Device which bridges across the knee joint; Arthroscopic-Assisted Frame Application: Fixation of a Tibial Plateau Fracture with an External Fixation Device and an Arthroscope to ensure accurate articular surface reduction; Frame Application with Internal Fixation: Fixation of a Tibial Plateau Fracture with an External Fixation Device along with Internal Fixation; AO/OTA Classification: The Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association Tibial Plateau Fracture Classification. This comprises three main categories: Type A: Extra-Articular; Type B: Partial Articular; Type C: Articular; Schatzker Classification: The Schatzker Tibial Plateau Fracture Classification. This comprises six groups: I - Lateral Plateau Split Fracture; II - Lateral Plateau Split-Depression Fracture; III - Lateral Plateau Depression Fracture; IV Medial Plateau Fracture; V - Bicondylar Fracture; VI - Bicondylar Fracture with Metaphyseal-Diaphyseal Disassociation.
The manuscript is nice and well written.
Manuscript source: Invited manuscript
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Emara KM, Ohishi T S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1916] [Cited by in RCA: 2181] [Article Influence: 114.8] [Reference Citation Analysis (0)] |
| 2. | Chen HW, Liu GD, Wu LJ. Clinical and radiological outcomes following arthroscopic-assisted management of tibial plateau fractures: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:3464-3472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Court Brown C, McQueen MM, Tornetta III P. Trauma. Philadelphia: Lippincott Williams & Wilkins 2006; . |
| 4. | McNamara IR, Smith TO, Shepherd KL, Clark AB, Nielsen DM, Donell S, Hing CB. Surgical fixation methods for tibial plateau fractures. Cochrane Database Syst Rev. 2015;CD009679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Jiwanlal A, Jeray KJ. Outcome of Posterior Tibial Plateau Fixation. J Knee Surg. 2016;29:34-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18665] [Cited by in RCA: 17508] [Article Influence: 1094.3] [Reference Citation Analysis (1)] |
| 7. | Del Buono A, Smith R, Coco M, Woolley L, Denaro V, Maffulli N. Return to sports after ankle fractures: a systematic review. Br Med Bull. 2013;106:179-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Robertson GA, Wood AM. Return to sports after stress fractures of the tibial diaphysis: a systematic review. Br Med Bull. 2015;114:95-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Robertson GA, Wood AM. Return to Sport After Tibial Shaft Fractures: A Systematic Review. Sports Health. 2016;8:324-330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Robertson GA, Wood AM. Return to sport following clavicle fractures: a systematic review. Br Med Bull. 2016;119:111-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Canadian Orthopaedic Trauma S. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. Results of a multicenter, prospective, randomized clinical trial. J Bone Joint Surg Am. 2006;88:2613-2623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Ahearn N, Oppy A, Halliday R, Rowett-Harris J, Morris SA, Chesser TJ, Livingstone JA. The outcome following fixation of bicondylar tibial plateau fractures. Bone Joint J. 2014;96-B:956-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Keogh P, Kelly C, Cashman WF, McGuinness AJ, O’Rourke SK. Percutaneous screw fixation of tibial plateau fractures. Injury. 1992;23:387-389. [PubMed] |
| 14. | Morin V, Pailhé R, Sharma A, Rouchy RC, Cognault J, Rubens-Duval B, Saragaglia D. Moore I postero-medial articular tibial fracture in alpine skiers: Surgical management and return to sports activity. Injury. 2016;47:1282-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | van Dreumel RL, van Wunnik BP, Janssen L, Simons PC, Janzing HM. Mid- to long-term functional outcome after open reduction and internal fixation of tibial plateau fractures. Injury. 2015;46:1608-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 89] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 16. | Chang SM, Hu SJ, Zhang YQ, Yao MW, Ma Z, Wang X, Dargel J, Eysel P. A surgical protocol for bicondylar four-quadrant tibial plateau fractures. Int Orthop. 2014;38:2559-2564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 17. | Stevens DG, Beharry R, McKee MD, Waddell JP, Schemitsch EH. The long-term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma. 2001;15:312-320. [PubMed] |
| 18. | Waldrop JI, Macey TI, Trettin JC, Bourgeois WR, Hughston JC. Fractures of the posterolateral tibial plateau. Am J Sports Med. 1988;16:492-498. [PubMed] |
| 19. | Brunner A, Honigmann P, Horisberger M, Babst R. Open reduction and fixation of medial Moore type II fractures of the tibial plateau by a direct dorsal approach. Arch Orthop Trauma Surg. 2009;129:1233-1238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Chin TY, Bardana D, Bailey M, Williamson OD, Miller R, Edwards ER, Esser MP. Functional outcome of tibial plateau fractures treated with the fine-wire fixator. Injury. 2005;36:1467-1475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Katsenis D, Athanasiou V, Megas P, Tyllianakis M, Lambiris E. Minimal internal fixation augmented by small wire transfixion frames for high-energy tibial plateau fractures. J Orthop Trauma. 2005;19:241-248. [PubMed] |
| 22. | Katsenis D, Dendrinos G, Kouris A, Savas N, Schoinochoritis N, Pogiatzis K. Combination of fine wire fixation and limited internal fixation for high-energy tibial plateau fractures: functional results at minimum 5-year follow-up. J Orthop Trauma. 2009;23:493-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Weigel DP, Marsh JL. High-energy fractures of the tibial plateau. Knee function after longer follow-up. J Bone Joint Surg Am. 2002;84-A:1541-1551. [PubMed] |
| 24. | Itokazu M, Matsunaga T, Ishii M, Kusakabe H, Wyni Y. Use of arthroscopy and interporous hydroxyapatite as a bone graft substitute in tibial plateau fractures. Arch Orthop Trauma Surg. 1996;115:45-48. [PubMed] |
| 25. | Chan YS, Chiu CH, Lo YP, Chen AC, Hsu KY, Wang CJ, Chen WJ. Arthroscopy-assisted surgery for tibial plateau fractures: 2- to 10-year follow-up results. Arthroscopy. 2008;24:760-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Chan YS, Yuan LJ, Hung SS, Wang CJ, Yu SW, Chen CY, Chao EK, Lee MS. Arthroscopic-assisted reduction with bilateral buttress plate fixation of complex tibial plateau fractures. Arthroscopy. 2003;19:974-984. [PubMed] |
| 27. | Kampa J, Dunlay R, Sikka R, Swiontkowski M. Arthroscopic-Assisted Fixation of Tibial Plateau Fractures: Patient-Reported Postoperative Activity Levels. Orthopedics. 2016;39:e486-e491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Gill TJ, Moezzi DM, Oates KM, Sterett WI. Arthroscopic reduction and internal fixation of tibial plateau fractures in skiing. Clin Orthop Relat Res. 2001;243-249. [PubMed] |
| 29. | Duan XJ, Yang L, Guo L, Chen GX, Dai G. Arthroscopically assisted treatment for Schatzker type I-V tibial plateau fractures. Chin J Traumatol. 2008;11:288-292. [PubMed] |
| 30. | Holzach P, Matter P, Minter J. Arthroscopically assisted treatment of lateral tibial plateau fractures in skiers: use of a cannulated reduction system. J Orthop Trauma. 1994;8:273-281. [PubMed] |
| 31. | Guanche CA, Markman AW. Arthroscopic management of tibial plateau fractures. Arthroscopy. 1993;9:467-471. [PubMed] |
| 32. | Hung SS, Chao EK, Chan YS, Yuan LJ, Chung PC, Chen CY, Lee MS, Wang CJ. Arthroscopically assisted osteosynthesis for tibial plateau fractures. J Trauma. 2003;54:356-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 46] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 33. | Pizanis A, Garcia P, Pohlemann T, Burkhardt M. Balloon tibioplasty: a useful tool for reduction of tibial plateau depression fractures. J Orthop Trauma. 2012;26:e88-e93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 34. | Chiu CH, Cheng CY, Tsai MC, Chang SS, Chen AC, Chen YJ, Chan YS. Arthroscopy-assisted reduction of posteromedial tibial plateau fractures with buttress plate and cannulated screw construct. Arthroscopy. 2013;29:1346-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 35. | Scheerlinck T, Ng CS, Handelberg F, Casteleyn PP. Medium-term results of percutaneous, arthroscopically-assisted osteosynthesis of fractures of the tibial plateau. J Bone Joint Surg Br. 1998;80:959-964. [PubMed] |
| 36. | Kraus TM, Martetschläger F, Müller D, Braun KF, Ahrens P, Siebenlist S, Stöckle U, Sandmann GH. Return to sports activity after tibial plateau fractures: 89 cases with minimum 24-month follow-up. Am J Sports Med. 2012;40:2845-2852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 37. | Loibl M, Bäumlein M, Massen F, Gueorguiev B, Glaab R, Perren T, Rillmann P, Ryf C, Naal FD. Sports activity after surgical treatment of intra-articular tibial plateau fractures in skiers. Am J Sports Med. 2013;41:1340-1347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 38. | Wang Z, Tang Z, Liu C, Liu J, Xu Y. Comparison of outcome of ARIF and ORIF in the treatment of tibial plateau fractures. Knee Surg Sports Traumatol Arthrosc. 2017;25:578-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |