Published online Jul 18, 2017. doi: 10.5312/wjo.v8.i7.567
Peer-review started: November 24, 2016
First decision: February 17, 2017
Revised: April 18, 2017
Accepted: May 3, 2017
Article in press: May 5, 2017
Published online: July 18, 2017
Processing time: 232 Days and 8.4 Hours
To determine technical considerations and radiographic outcomes of the Synthes volar rim distal radius plate to treat complex intra-articular fractures.
This review highlights technical considerations learnt using this implant since it was introduced in a major trauma unit in November 2011, including anatomical reduction and whether this was maintained radiographically.
Twenty-six of the 382 internally fixed distal radial fractures at our unit (6.8%) were deemed to require this plate in order to achieve optimal fracture fixation between November 2011 and May 2014. A further dorsal and/or radial plate was necessary in 35% and variable angle screws were used in 54% of cases. Post-operatively, mean radial height, inclination, volar tilt and ulnar variance restored were 11.7 mm, 21º, 4.3º and -1.2 mm respectively. There were no cases of non-union or flexor/extensor tendon rupture; one case of loss of fracture reduction. Overall incidence of plate removal was 15% with one plate removed for flexor and one for extensor tendon irritation
The use of a rim plate enables control of challenging far distal fracture patterns. However, additional plates were required to improve and maintain reduction. Variable angle screws were necessary in half the cases to avoid intra-articular screw penetration. If used judiciously, this implant can achieve stable fixation despite the complexity of the fracture pattern.
Core tip: Far distal intra-articular fractures of the distal radius are not easily treated with standard volar plates. The rim plate is designed to sit distal to the watershed line, allowing purchase of bone fragments and subchondral support of the articular surface, enabling early mobilization. In view of the implant’s design, variable angle screws are necessary to avoid intra-articular screw penetration. Intra-operatively, reduction and stable fixation should be assessed fluoroscopically during wrist movement, and if necessary, an additional dorsal plate applied to allow mobilization. Judicious use of this implant can restore anatomical reduction and stable fixation in this complex subset of fractures.
- Citation: Spiteri M, Roberts D, Ng W, Matthews J, Power D. Distal radius volar rim plate: Technical and radiographic considerations. World J Orthop 2017; 8(7): 567-573
- URL: https://www.wjgnet.com/2218-5836/full/v8/i7/567.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i7.567
The application of locking plate technology to distal radius fracture fixation enables dorsally unstable fracture configurations to be reliably reduced and internally fixed using a volar approach and volar implant placement. The volar approach has gained widespread popularity due to the perceived benefits of greater soft tissue cover over the implant and less tendon irritation than with the dorsal approach. This technique may be used for the majority of distal radius fractures, however an understanding of fracture anatomy and biomechanics as well as correct implant choice and placement are critical to a successful outcome. Indeed one implant cannot provide a stable fixation for all configurations through the volar approach[1]. The non-specialist trauma surgeon will be familiar with the volar approach but should recognize those fracture configurations that may need dorsal or combined volar and dorsal approaches. In these complex intra-articular cases the use of pre-operative computerised tomography (CT) aids planning the surgical approach and choice of implant.
The AO-23B3 fracture with a small distal and volar fragment and the AO-23C3 fracture with articular comminution are two fracture subtypes where a standard volar plate positioned proximal to the watershed line[2] will not provide a sufficient buttress for the distal fragments and there is a risk of secondary volar displacement of the fragment along with the carpus distal to the plate. An early plate design for these fracture subtypes was the Synthes juxta-articular plate but due to the distal plate positioning and angular design tendon irritation was problematic, often necessitating implant removal after fracture union. The distal screws were originally inserted in a fixed angle configuration that is proximally directed to avoid screw penetration of the radio-carpal joint, which was a significant risk if the distal fragment was small or the volar tilt incompletely corrected. In addition, there was no second row angled buttress for dorsal joint surface support.
The Synthes variable angle two column plate design was developed from the extra-articular and juxta-articular designs and offers an anatomically contoured plate, which is positioned close to the watershed line and can be used for fixation of the majority of distal radius fractures. However, reliable fixation of the far distal fracture subtype remains problematic. The variable angle distal radius rim plate was introduced in our unit in autumn 2011 and is designed for these complex fractures. It is inserted via a volar approach and is placed over the watershed line as it is pre-contoured to fit the volar rim of the distal radius. The edges of the plate are designed to provide a smooth surface against which the flexor digitorum profundus and flexor pollicis longus tendons may glide with minimal irritation. Due to the distal placement of the plate, there is a theoretical risk of intra-articular screw placement. To reduce this risk, the screw options include fixed or variable angle subtypes to allow proximal direction of screws away from the joint. These also allow purchase of small fracture fragments where a fixed angle screw would enter a fracture line. There are a number of important technical considerations for plate positioning, anatomical fracture reduction, avoiding screw penetration to the joint and minimising the risk of secondary displacement. This is especially pertinent with the AO-23C3 fracture configuration when successful volar buttress of small distal fragments may unmask distal and dorsal instability necessitating supplementary dorsal plating.
This paper reports on a series of twenty-six consecutive cases of Synthes variable angle 2.4 distal radius rim plates used for distal radius fracture fixation at a major trauma and tertiary referral hand centre between November 2011 and May 2014. All patients treated with this implant were identified from a database of distal radius fracture fixations compiled from theatre logbooks and cross-referenced with implant logbooks. The pre-operative radiographs and CT scans were used to assess fracture configuration. All post-operative radiographs were reviewed to measure volar tilt, inclination and radial height in order to assess restoration of anatomy. All radiographs were reviewed taken in the same radiology unit using the same machine calibration. Operative records and imaging, medical and therapy records were used to monitor progression of the fracture to union and retention of post-operative fracture reduction.
The primary outcome measures were initial and final radiographic alignment parameters to assess maintenance of fracture reduction, and implant removal. Secondary outcome measures were the use of variable angle screws, the need for accessory plate support and tendon irritation/rupture.
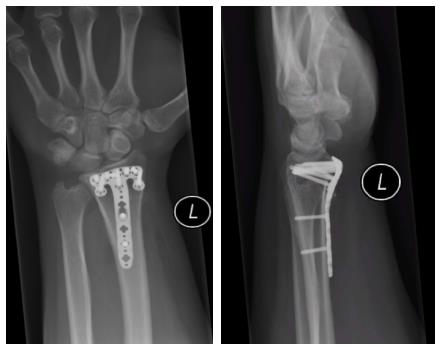
During the study period, 382 distal radius fractures were treated operatively with internal fixation, the majority using a volar approach (83.5%). Twenty-six distal radius fixations utilised rim plates accounting for 6.8% of all operations. The rim plate was used in isolation in seventeen cases (Figure 1), however an additional dorsal or dorso-radial approach to reduce and maintain reduction of fracture fragments was required in 35% of cases. This equates to half the total number of distal radial fractures requiring combination plating, highlighting the complexity of the fractures for which rim plates were used.
The use of variable angle screws was higher in this subset of patients, with 54% of cases requiring a median of four such screws. Variable angle screws were required to reduce the risk of joint penetration and to optimise screw configurations in comminuted fractures when a fixed angle screw would sit within a fracture line and not provide sufficient subchondral support.
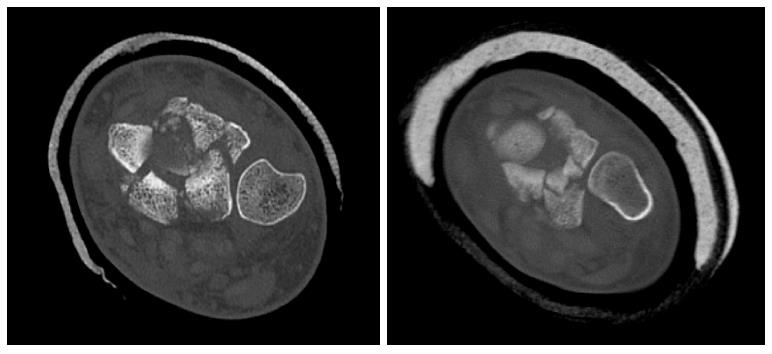
All fractures were classified as either AO-23B3 or AO-23C3 with a significant degree of articular and metaphyseal comminution. To evaluate the degree of fracture comminution, the size of the dorso-ulnar and radial styloid fracture fragments were assessed on pre-operative CT scans.
Analysis of the CT coronal and axial sections demonstrated no significant difference in the size of the dorsal fragments between the groups treated with a single volar rim plate and those treated with a combined approach using a second dorso-ulnar buttress plate.
In all twenty-six cases there was a significant level of comminution, which also involved the distal radio-ulnar joint in twenty-two cases (five of these cases having a simple coronal split through this joint and the others having multi-fragmentary fracture configurations) (Figure 2). The main sites of articular comminution were in the dorso-ulnar and volar-ulnar regions of the distal radius rather than the radial styloid, where most of the fragmentation was metaphyseal.
In six cases (23%) there was a volar instability pattern at presentation with volar translation of the carpus together with the distal volar ulnar fragments. Involvement of the lunate fossa had a die punch fracture configuration in all cases (Figure 3). The dorso-ulnar fragments sustained a higher degree of comminution when compared to their volar counterpart in sixteen of the twenty six cases (Figure 4).
Standard volar variable angle plates are sited too proximal to secure and buttress these volar lip marginal fragments (Figure 4), therefore allowing carpal translation to occur despite apparent adequate fixation intra-operatively. By stabilizing these volar marginal lip fragments, the rim plate avoids this potential for secondary displacement[1,2].
Fracture reduction was assessed by measuring volar tilt, radial inclination, radial height and ulnar variance on the post-operative radiographs. Alignment was restored to 4.3 ± 5.5 degrees volar tilt, mean radial inclination of 21.2 degrees (range: 15-30 degrees), 11.7 mm (range: 7-16 mm) radial height and -1.2 mm (range: -4.5-2.5) ulnar variance.
Six patients did not complete follow-up in our unit. Two patients were not from our region and attended follow-up at their local units, and four patients declined the offer of follow-up beyond six weeks. The patients who discontinued follow up have not been referred back to our unit with complications of tendon irritation or rupture.
The 20 patients completing follow-up all demonstrated radiographic fracture union by 12 wk from surgery. There are no cases of either flexor or extensor tendon rupture and two cases of tendon irritation. Post-operative loss of reduction occurred in one polytrauma case, with loss of volar tilt and height. No intervention was required and the patient was asymptomatic at eighteen months after surgery.
Four patients required removal of metalwork. One patient clinically had first extensor compartment tendon irritation due to a prominent screw following an isolated volar operative approach; one patient had pain on grip strength testing, which may have represented flexor tendon irritation. This resolved after removal of the volar plate and a dorsal lunate fossa fragment buttress plate. One case had radiographic signs of avascular necrosis of the lunate fossa fragment. This was asymptomatic until a second fall after which the patient developed new onset dorso-radial pain symptoms. A diagnostic arthroscopy identified screw penetrance into the joint; one case had the volar plate removed at the same time as a triangular fibrocartilagenous complex repair for symptoms of distal radio-ulnar joint instability.
The indications for a variable angle volar rim plate are for the infrequent AO-23B3 and AO-23C3 distal radius fractures where the distal and volar fragments cannot be adequately buttressed with standard extra-articular and variable angle two column volar plates.
Prior to the launch of the volar rim plate these distal fractures were managed in our unit with a volar juxta-articular plate or with an extra-articular plate and supplementary distal lag screws. However, this plate has a higher profile and angular design and therefore is more likely to cause flexor tendon irritation necessitating implant removal.
Alternatively they were treated by a dorsal only approach if the primary instability was thought to be dorsal, however an unmasked volar instability could result in volar displacement of the carpus with the volar distal fracture fragment at the lunate facet buttress.
Rarely they were treated with a external fixator or a temporary 3.3 mm 16 hole distraction bridge plate spanning the fracture site and carpus[3]. Both of these techniques offer reliable fracture union, but unlike the volar rim plate, it is not possible to restore most aspects of distal radius anatomy as well as radio-carpal and distal radio-ulnar congruity. They also have other specific complications, including stiffness, pin tract infection and metacarpal fracture at the site of distal pin or screw insertion[4].
Due to the complexity of these fractures, a preoperative CT scan is required for in depth assessment of the fracture configuration. Unfortunately, there were no predictors on the scans which can be used to identify fractures that are more likely to need additional plating via a dorsal or dorso-radial approach. We attempted to correlate the size of the fracture fragments with the need for additional plates, but no correlation was evident. This decision was made intra-operatively on assessment of fracture stability after volar plating.
In this series of rim plate fixations of distal radius fractures a combined dorsal and volar plating approach was required in 35% of procedures (Figure 5). If the distal fracture configuration with potential for volar and dorsal instability is identified from the pre-operative CT scan it is important that the treating surgeon is familiar with the dorsal approach in case an adjuvant dorsal plate is required. The alternative is to refer the case on to a specialist wrist surgeon who is familiar with both approaches. Whilst the rim plate increases the numbers of fractures and configurations that may be managed with internal fixation through the volar approach it does not obviate the need for the dorsal approach.
The rim plate has a low profile to allow its placement distal to the watershed line without increasing the risk of flexor tendon irritation. Despite its distal placement, in this series, there were no cases of flexor tendon rupture and only two of the four cases of implant removal were for flexor or extensor tendon irritation. This is consistent with the literature which suggests that attrition flexor tendon rupture is infrequent yet may occur with prominent higher profile plates placed at the watershed line, but is unlikely in cases were plates are designed to be placed more distal to this line, probably due to their contoured design and low profile[5].
Signs of tendon irritation were noted at clinic review between three and six months post-operatively when range of motion had been restored and the patients had regained grip strength and pre-injury activity levels. None of the other cases were symptomatic or had signs of tendon irritation up to one year after surgery. Hence we suggest a minimum follow up until six months post-operatively and removal of implants if there are clinical signs of tendon irritation, rather than awaiting patients to be symptomatic thus decreasing the risk of attrition tendon ruptures. The published recommendations for removal of previous volar plate designs include only symptomatic patients who had plate prominence more than 2 mm volarly at the watershed line or plate position within 3 mm of the volar rim[6].
The volar rim of the lunate fossa is anatomically designed to resist volar carpal translation and the short radiolunate ligament, which attaches to the volar lip fragment, stabilizes the carpus on the distal radius. The carpus can therefore translate volarly with the distal volar and ulnar fracture fragment of the distal radius. This fragment must be anatomically reduced and buttressed to prevent this volar instability. Standard volar variable angle plates are sited too proximal to secure and buttress these volar lip marginal fragments, therefore allowing carpal translation to occur despite apparent adequate fixation intra-operatively. The rim plate contour is designed to overhang and engage the distal volar lip fragments avoiding this potential for secondary displacement. Due to the variable angle screw option, this plate also allows purchase on these small fragments without joint penetration.
Even though the radial styloid had more metaphyseal than distal comminution in this series, variable angle screws were required, as fixed angle screws did not adequately engage the bone fragments due to their fixed trajectory, and in most cases the angle of these screws was changed as necessary to ensure stable fixation.
Unfortunately, this was not always enough to achieve adequate fracture stabilization. After volar plate fixation, all fractures were assessed for stability to ensure that the fracture and carpus are stable through a full range of motion. In 35% of cases this was not the case. Therefore an additional plate was placed either along the radial styloid to bridge and secure this styloid fracture; or over the lunate fossa fragment via a dorsal approach. In the latter cases, which all had a higher degree of dorso-ulnar than volar-ulnar comminution, rim plates were used to engage the distal volar lip fragments and act as a subchondral raft supporting the radio-carpal joint, aiding adequate restoration of radial height, tilt and angulation. The additional dorsal plates were then applied to buttress the dorso-ulnar fragments, preventing their displacement and translation whilst enhancing radio-carpal and distal radio-ulnar joint stability.
The distal radio-ulnar joint was involved in 85% of cases, with varying degrees of central comminution; a simple split in the coronal plane occurred in only 5 cases. Congruity was restored through the volar approach by using the variable angle screw option and changing the angle of screw insertion to capture the dorso-ulnar fragments. However this was not possible in all cases and an additional buttress plate was applied to the dorso-ulnar fragments in cases of significant comminution.
Besides allowing bone purchase of the distal radial fragments, which is important for fracture stability[7], variable angle screws decrease the risk of intra-articular screw penetration into the radio-carpal and distal radio-ulnar joints by allowing multidirectional angulation of screws, if necessary. This risk is heightened due to the degree of intra-articular comminution in these fractures and small size of the fragments that are often only large enough to allow fixation with a single screw, sometimes only by using this variable angle option. Some studies have highlighted increased incidence of removal of metalwork[8] due to intra-articular placement of fixed angle screws probably as a result of incomplete restoration of volar tilt, distal plate positioning or angulation of the plate.
In this series there was only one case of radio-carpal screw penetration which was noted arthroscopically in a patient who was asymptomatic until sustaining a fall six months following fracture fixation and subsequently developed dorso-radial wrist pain. The implant was removed at the same sitting. In this case, it is hard to determine whether the screw was placed in an intra-articular position at surgery, whether this occurred after the second fall, or whether it was due to avascular necrosis of the lunate fossa fragments secondary to the original injury and plate fixation.
This low incidence of intra-articular screw penetration was perhaps due to careful pre- and intra-operative planning of screw positioning, the liberal use of variable angle screws and the use of additional dorsal plates to aid stability if volar screw placement to capture the dorsal fragments was deemed to be at risk of breaching the articular surface.
Post-operative radiographs showed correction of radial height, inclination and ulnar variance similar to that quoted in the literature for standard volar locking plates used for AO-23A2, A3, C1-3[9], with only one case of loss of volar tilt correction after fracture fixation using a solitary volar approach, This required no further surgical intervention as the patient remained asymptomatic.
The main difference with this implant is the inability to restore volar tilt to the same extent as with standard volar plates, where a mean correction of 6 degrees (0-18 degrees) is described in the literature[10-13] and 4.3 degrees in our series. Our results using the rim plate are therefore within the lower limits of this range for standard volar locking plates. This is partly due to the complexity of the fracture pattern and metaphyseal comminution, but also due to the far distal plate position requiring wrist hyperextension for adequate plate and distal screw placement, hence placing limitations on the degree of correction of volar tilt that can be achieved. The joint comminution precludes distal first fixation and then reduction to the shaft of radius.
Ideally, the study should include a larger cohort of patients, and a longer duration of follow up in clinic can be considered. Unfortunately, as these fractures are not common this is not possible unless a multicentre approach is used.
In conclusion, this case series of variable angle distal radius rim plates highlights the fact that these implants are indicated for the far distal and complex intra-articular fractures of the distal radius, but cannot achieve enough stability in isolation for all fractures. Some fractures require additional plating techniques, therefore we recommend that all AO-23C3 fractures should be assessed with a pre-operative CT scan. If trauma surgeons are not confident with dorsal plating techniques, it would be appropriate to consider referral to a specialised wrist surgeon who can base decisions on a combination of factors including pre-operative imaging, intra-operative findings and their experience with the various techniques and implants available. When used appropriately, good results can be achieved using this plate with correction and maintenance of distal radial anatomy. There were few cases of tendon irritation and no cases of flexor or extensor tendon rupture but we recommend prompt removal of implants if there are signs of tendon irritation.
Pre-operative CT scan provides information of fracture configuration and consideration of referral to specialist wrist surgeon if necessary; Radial styloid fixation often requires variable angle screws as the fixed angle trajectory does not always provide adequate hold; Variable angle screws in the lunate facet buttress may prevent penetration of the radio-carpal or DRUJ but may not adequately capture dorsal fragments; Volar tilt restoration is less reliable than the other alignment parameters due to the technique of plate insertion; Intra-operative assessment of stability of fracture fixation necessary after volar plating for assessment of dorsal fracture stability; additional dorsal and/or radial plates are necessary to stabilize these fractures in 35% of cases; plate positioning distal to the watershed line can lead to tendon irritation and risk of attrition rupture requiring removal of implant.
Far distal intra-articular fractures of the distal radius involving the volar rim are a specific subset of fractures which are difficult to treat in view of the small size of the fracture fragments, location and instability. If stable fixation is not achieved, volar carpal subluxation can occur due to the attachment of the marginal bone fragments to the short radiolunate ligament. Standard volar plate placement proximal to the watershed line poses problems when treating these fractures.
In recent years, various plates have been designed with various contours and lower profiles to facilitate fracture fixation and decrease the risk of tendon irritation yet still achieve anatomical reduction, stable fixation and allow early mobilization.
The rim plate is a pre-contoured low profile implant, having standard locking and variable angle locking screw options, to allow plate placement distal to the watershed line whilst decreasing the risk of screw penetration into the joint. The aim of this design is to allow fixation of the intra-articular fractures of the distal radius which involve the marginal volar rim. Besides the risk of screw penetration into the radio-carpal and distal radio-ulnar joints when using such a distally sited plate, the other main risk is tendon irritation and rupture. Recent literature has shown that low profile plates can be safely applied at and beyond the watershed line if used appropriately.
This study shows that this implant allows subchondral support of the articular surface achieving anatomical reduction. Judicious use of a combination of distal standard locking and variable angle locking screws allows purchase of bone fragments, especially of the dorso-ulnar fragment and avoids intra-articular screw penetration. The manuscript also provides information about the need for additional fixation in certain cases and the risk of tendon irritation.
The manuscript aimed to retrospectively report the clinical outcomes of fixation of far distal intra-articular distal radial fractures using variable angle distal radius rim plate. This topic is interesting and the language is excellent.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Guerado E, Kamburoglu K, Peng BG, Zhang L S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Tan KG, Chew WY. Beware! The volar ulnar fragment in a comminuted Bartons fracture. Hand Surg. 2013;18:331-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Orbay JL, Touhami A. Current concepts in volar fixed-angle fixation of unstable distal radius fractures. Clin Orthop Relat Res. 2006;445:58-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Power D, Mishra A, Vetharajan N. Response to: Beware the volar ulnar fragment in a comminuted Bartons fracture. Hand Surg. 2014;19:325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Hanel DP, Lu TS, Weil WM. Bridge plating of distal radius fractures: the Harborview method. Clin Orthop Relat Res. 2006;445:91-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Hanel DP, Ruhlman SD, Katolik LI, Allan CH. Complications associated with distraction plate fixation of wrist fractures. Hand Clin. 2010;26:237-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Soong M, Earp BE, Bishop G, Leung A, Blazar P. Volar locking plate implant prominence and flexor tendon rupture. J Bone Joint Surg Am. 2011;93:328-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 276] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 7. | Kitay A, Swanstrom M, Schreiber JJ, Carlson MG, Nguyen JT, Weiland AJ, Daluiski A. Volar plate position and flexor tendon rupture following distal radius fracture fixation. J Hand Surg Am. 2013;38:1091-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 8. | Mehling I, Müller LP, Delinsky K, Mehler D, Burkhart KJ, Rommens PM. Number and locations of screw fixation for volar fixed-angle plating of distal radius fractures: biomechanical study. J Hand Surg Am. 2010;35:885-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Sahu A, Charalambous CP, Mills SP, Batra S, Ravenscroft MJ. Reoperation for metalwork complications following the use of volar locking plates for distal radius fractures: a United Kingdom experience. Hand Surg. 2011;16:113-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21:316-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 452] [Cited by in RCA: 448] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 11. | Musgrave DS, Idler RS. Volar fixation of dorsally displaced distal radius fractures using the 2.4-mm locking compression plates. J Hand Surg Am. 2005;30:743-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 103] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Ring D, Jupiter JB, Brennwald J, Büchler U, Hastings H. Prospective multicenter trial of a plate for dorsal fixation of distal radius fractures. J Hand Surg Am. 1997;22:777-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 200] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 13. | Dario P, Matteo G, Carolina C, Marco G, Cristina D, Daniele F, Andrea F. Is it really necessary to restore radial anatomic parameters after distal radius fractures? Injury. 2014;45 Suppl 6:S21-S26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |