Published online Jun 18, 2017. doi: 10.5312/wjo.v8.i6.484
Peer-review started: October 23, 2016
First decision: December 20, 2016
Revised: January 6, 2017
Accepted: May 18, 2017
Article in press: May 19, 2017
Published online: June 18, 2017
Processing time: 238 Days and 21.1 Hours
To determine the location of medial tibial plateau stress fractures and its relationship with tibial plateau morphology using magnetic resonance imaging (MRI).
A retrospective review of patients with a diagnosis of stress fracture of the medial tibial plateau was performed for a 5-year period. Fourteen patients [three female and 11 male, with an average age of 36.4 years (range, 15-50 years)], who underwent knee MRI, were included. The appearance of the tibial plateau stress fracture and the geometry of the tibial plateau were reviewed and measured on MRI.
Thirteen of 14 stress fractures were linear, and one of them stellated on MRI images. The location of fractures was classified into three types. Three fractures were located anteromedially (AM type), six posteromedially (PM type), and five posteriorly (P type) at the medial tibial plateau. In addition, tibial posterior slope at the medial tibial plateau tended to be larger when the fracture was located more posteriorly on MRI.
We found that MRI showed three different localizations of medial tibial plateau stress fractures, which were associated with tibial posterior slope at the medial tibial plateau.
Core tip: Stress fracture of the medial tibial plateau is a rare injury. No studies have investigated detailed magnetic resonance imaging features of this fracture type. We found three distinct location types of isolated stress fractures of the medial tibial plateau. Posterior tibial slope serves as an indicator to determine the fracture site at the medial tibial plateau.
- Citation: Yukata K, Yamanaka I, Ueda Y, Nakai S, Ogasa H, Oishi Y, Hamawaki JI. Medial tibial plateau morphology and stress fracture location: A magnetic resonance imaging study. World J Orthop 2017; 8(6): 484-490
- URL: https://www.wjgnet.com/2218-5836/full/v8/i6/484.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i6.484
Stress fractures of the lower extremity commonly occur in athletes and military personnel. The tibial shaft is the most common location for stress fractures during running and marching activities, whereas the medial tibial plateau is a relatively uncommon site. Engber et al[1] reported a series of 36 patients (57 fractures) including 21 bilateral in 1977. Harolds[2] also reported 105 fractures in 71 soldiers in 1981. They documented that this fracture type is difficult to detect on initial roentgenograms at the onset of symptoms. This injury is easily misdiagnosed because the location of pain and tenderness is very similar to the meniscal injury and pes anserinus bursitis, which are common problems in running activities.
Bone scintigraphy, computed tomography (CT), and magnetic resonance imaging (MRI) are widely used for early detection of stress fractures. Among them, MRI has been found to be more sensitive than CT and more specific than scintigraphy[3]. Clinical case reports have described that MRI is a more sensitive method for evaluating stress fractures of the medial tibial plateau compared with X-rays[4-6]. T2- and STIR-MR images are useful for detecting edema of the cancellous bone that usually presents as a linear fracture line at the medial tibial plateau[7]. However, no studies have investigated more detailed MRI features of medial tibial plateau stress fractures.
The purpose of this study was to determine the detailed MRI appearance of medial tibial plateau stress fractures including localization and morphology. We found three different types of location in stress fracture of the medial tibial plateau. Thus, the geometry of the tibial plateau in patients with stress fractures of medial tibial plateau and the relationship with the fracture location were also evaluated.
The study protocol was approved by the institutional review board, and the requirement for informed consent was waived. For the present study, we searched the key words “tibial plateau” and “stress fracture” using a database of our institutes’ medical records between April 2010 and March 2015, and identified 22 patients. The authors reviewed all medical records. No fractures were observed on MRI in 3 patients, and MRI was not taken in 4 other patients. We excluded these 7 patients in the present study. In addition, one patient was excluded because of a fracture of the medial tibial plateau for which a traumatic event of the affected knee could be identified. Finally, we selected a total of 14 patients [eleven men and three women; mean age, 36.4 years (range, 15-50 years)] with eight right and six left medial tibial plateau stress fractures (Table 1). All patients did not have any relevant medical co-morbidities, such as rheumatoid arthritis, metabolic disease, or osteoporosis in the medical record review, although we did not evaluate bone mineral density (BMD) in the present patients.
| MRI classification | Case No. | Age (yr) | Gender | Affected side | Activity | MRI after onset (d) | Fracture pattern | Medial slope (degrees) | Posterior slope (degrees) |
| AM type | 1 | 48 | Male | Right | Jog | 16 | Linear | 4.7 | 4.5 |
| 2 | 29 | Male | Right | Jog | 12 | Linear | 1.7 | 4.9 | |
| 3 | 15 | Male | Left | Jog | 13 | Linear | 6.1 | 5.5 | |
| PM type | 4 | 46 | Male | Right | Jog | 14 | Linear | 3.3 | 9.9 |
| 5 | 48 | Male | Left | Marathon | 0 | Linear | 2.4 | 6.7 | |
| 6 | 29 | Male | Right | Jog | 12 | Linear | 0.9 | 7 | |
| 7 | 44 | Female | Left | Jog | 9 | Linear | 4.5 | 7.7 | |
| 8 | 30 | Female | Right | Rope jump | 13 | Linear | 3.3 | 7.8 | |
| 9 | 40 | Male | Left | Jog | 14 | Linear | 0.9 | 8.2 | |
| P type | 10 | 33 | Male | Right | Jog | 18 | Linear | 5.4 | 10.1 |
| 11 | 50 | Male | Right | Jog | 99 | Linear | 4.8 | 12.2 | |
| 12 | 20 | Male | Left | Jog | 25 | Linear | -0.2 | 12.4 | |
| 13 | 39 | Male | Left | Jog | 127 | Stellate | 2.2 | 11 | |
| 14 | 38 | Female | Right | Jog | 17 | Linear | 0.9 | 11.4 |
The main complaint of all patients was pain in the medial aspect of the proximal part of the tibia, without any traumatic events. On physical examination, tenderness was consistent with the pain site. All cases had no limitation of knee range of motion for reasons other than pain. We did not identify an apparent joint effusion in any patients. All cases did not report sudden onset of discomfort. Thirteen cases were associated with long-distance running (jog or marathon), and one case was associated with rope jump. The delay between symptom onset and seeking medical service ranged from 0 to 120 d (average, 21.9 d).
Initial anterior-posterior and lateral plain radiographs of the affected knee were taken within 2 wk of onset of symptoms (average, 7.9 d) in 12 of 14 patients. No fracture lines on X-rays were observed in these patients.
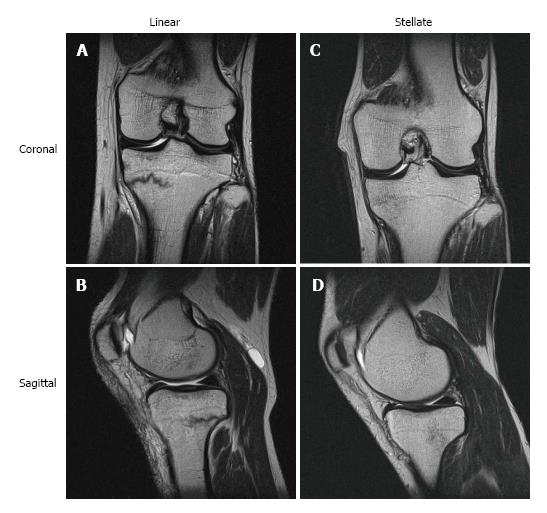
MRI scans were completed in all 14 patients. MRI of the knee was performed with a 1.5-T MRI scanner (EXCELART Vantage, TOSHIBA, Japan) using a knee coil. Proton density (PD) weighted MRI (TR/TE, 3750/18) and T2-weighted MRI scans (4100/90) sequences were performed in coronal, sagittal, and axial planes according to our routine knee MRI protocol. MRI parameters for all sequences were as follows: FOV, 16-16 cm; 1 excitation; matrix size, 256 × 368; section thickness, 3 mm for coronal, sagittal, and axial planes; and intersection gap, 1 mm. MRI revealed a linear or stellate PD and T2-low weighted image at the medial tibial plateau in all 14 cases (Figure 1). We did not identify any other associated findings on the MRI scans like osteoarthritis, ligament or meniscal pathology, or articular cartilage lesions.
Stress fractures of the medial tibial plateau were characterized on the basis of its regional location and morphology (linear or stellate). We classified fracture locations using both sagittal and coronal T2-weighted images. Images between the image slice that had the tibial insertion of both the anterior and posterior cruciate ligaments, to the most medial slice that included the tibial condyle at the fracture level, were 7 or 8 slices in the present cases. At first, we divided the fracture locations into the following two types: Anterior (more images that included a fracture line at the anterior tibial cortex) and posterior (more images that included a fracture line at the posterior tibial cortex). Next, they were divided into two subtypes (medial or not) based on whether the most medial slice included a fracture line or not.
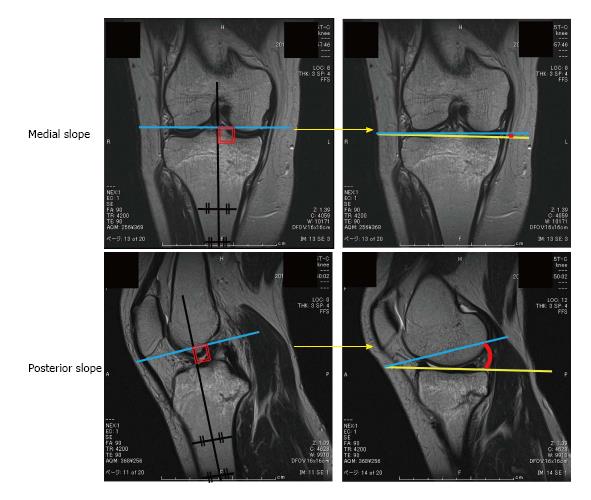
In addition, to investigate the relationship between the fracture location and the geometry of the medial tibial plateau, we measured the posterior tibial slope and medial tibial slope at the medial tibial plateau on the sagittal and coronal planes of T2-weighted images using ImageJ software according to the measurement reported by Hashemi et al[8]. Briefly, the transverse image passing through the tibiofemoral joint was used to identify the coronal plane that passed closest to the centroid of the tibial plateau and the sagittal plane that included both anterior and posterior cruciate ligaments. The longitudinal axis of the tibia in the coronal and sagittal planes was defined by determining the midpoint of the medial-to-lateral and anterior-to-posterior widths of the tibia at two points located approximately 3 cm apart and as distally in the image as possible (Figure 2). The medial slope in the coronal plane and the sagittal slope of the medial tibial plateau in the sagittal plane were then measured as the angle between a line joining the peak points on the medial-to-lateral, and the anterior-to-posterior aspects of the plateau and the longitudinal axis. The measured value was rounded off to the first decimal place. Two orthopaedic surgeons (KY and YU) separately measured both tibial posterior and medial slope of fourteen MRIs in a blind manner. Two investigators evaluated the parameters twice with a 1-wk interval. To test intra- and inter-observer reliability, the intraclass correlation coefficient (ICC) was calculated for two assessors.
All statistical analyses were performed with R2.8.1. Intra-interobserver agreement was assessed by ICC. The data was analyzed by Kruskal-Wallis and post-hoc Mann Whitney with Holm’s correction for determination of differences between three groups, and presented as the mean ± SE. P value < 0.05 was considered statistically significant.
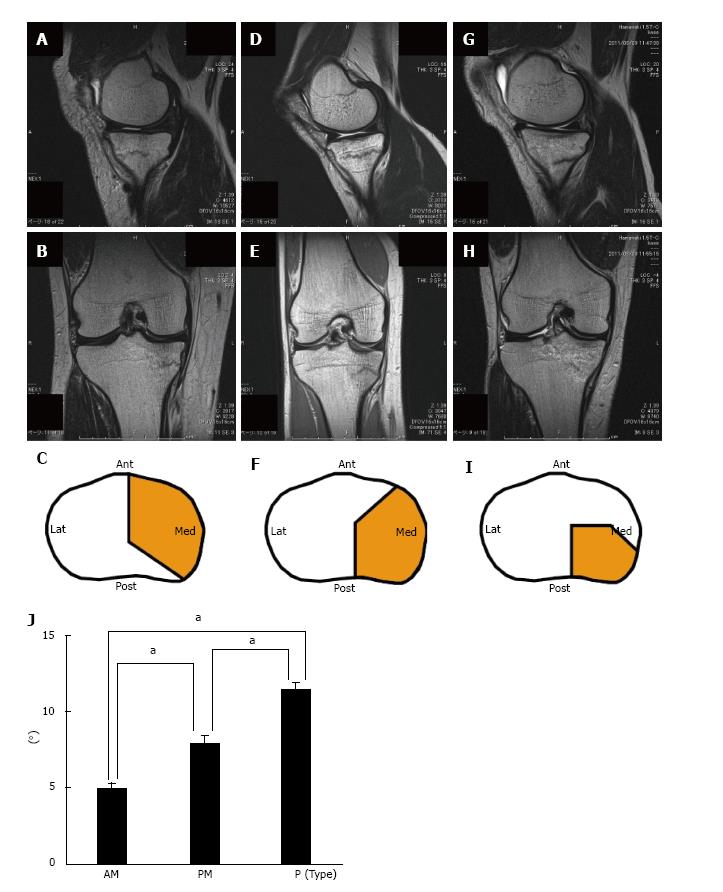
MRI of the affected knee demonstrated a PD-low and T2-low linear fracture line at the medial tibial plateau in 13 of 14 patients (Figure 1A and B). One patient had a stellate pattern at the posteromedial part of the tibial plateau (Figure 1C and D). In this case, a linear fracture line might have disappeared because initial MRI was taken at 127 d after the onset. Location of the medial tibial plateau stress fractures was divided into three groups; 3 fractures at the anteromedially (AM) type (Figure 3A-C), 6 posteromedially (PM) type (Figure 3D-F) and 5 posteriorly (P) type (Figure 3G-I). There were no fractures with anterior (A) type. We further investigated the correlation between the fracture type and tibial plateau geometry. Intra-interobsever agreement for the detection of the medial slope and posterior slope at the medial tibial plateau on MRI was very good (tibial posterior slope; intra (r = 0.972; 95%CI, 0.917-0.990), inter (r = 0.933; 95%CI, 0.811-0.978), tibial medial slope; intra (r = 0.935; 95%CI, 0.814-0.978), inter (r = 0.895; 95%CI, 0.715-0.965). The posterior slope in P type was average 11.4 degrees (range: 10.1-12.4 degrees), which was significantly larger than that in AM (average 5.0 degrees (range: 4.5-5.5 degrees) (P = 0.048) and PM (average 7.9 (range: 6.7-9.9 degrees) types (P = 0.013) (Figure 3J). The posterior slope in PM type was also significantly larger than that in AM type (P = 0.048). While, there were no differences between three fracture types about the medial slope.
Harolds[2] posited that the location of medial tibial plateau fatigue fractures are medial and posterior because it is here that weight-bearing stress is greatest. In agreement, the more frequent site of these stress fractures was medial and posterior in our study. But, we found that it occurred antero-medially in some cases. As a result, localization of the medial tibial plateau stress fracture was classified into the following three patterns based on MRI findings: AM, PM, and P types. Furthermore, fracture classification was correlated with the posterior slope of the medial tibial plateau.
Dynamic contact mechanics of the tibial plateau during running have not been elucidated, but cadaver studies have described the pressure distribution pattern of the knee during a simulated gait[9,10]. Bedi et al[9] demonstrated that the posterior portion of the plateau had higher peak contact pressures than the anterior portion in the stance phase of gait at 14% of the gait cycle, which correspond to 15° knee flexion with axial loads of 2280N. Wang et al[10] also reported that one of the most prominent contact stress patterns was observed at the posterior aspect of the medial tibial plateau in nine of 12 cadaveric knees with a single peak stress that occurred at 14%-18% of the gait cycle during the early stance phase. These results are consistent with the fact that more frequent location of medial tibial plateau stress fractures is posterior, although tibial posterior slope was not taken into consideration in their studies.
The tibial posterior slope is originally defined by the angle perpendicular to the longitudinal axis of the bone and tangent to the plateaus on the lateral radiographs. But, it is difficult to discriminate between the medial and lateral plateaus[11,12]. Recent studies have recommended separate assessment of tibial posterior slopes of the medial and lateral plateaus[8,13,14]. Matsuda et al[14] reported that the mean tibial posterior slope in the medial plateau on MRI examination was 10.7° (range, 5°-15.5°) in the normal knees of Japanese populations. This average value was similar to that of the present Japanese patients group. The present study indicated that increased the posterior slope caused the plateau to fracture more posteriorly. Giffin et al[15] reported that an increase in tibial posterior slope shifted the resting position of the tibia anteriorly relative to the femur. These data suggest that loading of the medial tibial plateau from the femoral condyle may shift from anterior to posterior due to the increased posterior tilt of the tibial plateau. However, the relationship between dynamic contact stress pattern on the tibial plateau and tibial posterior slope during gait and running still remains unclear.
In general, medial tibial plateau stress fractures are more common than stress fractures of the lateral tibial plateau[16,17]. Mizuta et al[16] reported a case of the lateral tibial plateau stress fracture, which was associated with knee valgus angulation with 92 degrees of medial tibial slope on radiographs. Hashemi et al[8] described that the lateral-to-medial slope of the tibial plateau, which they used the term “coronal tibial slope”, ranged between -1°and 6°, whereas the only one subject had a coronal tibial slope of 91° in normal subjects. In our cases of medial tibial plateau stress fractures, medial tibial slope ranged between -0.2° and 6.1°. These data suggest that the patient, who has medial tibial slope within normal limits, is subjected to medial tibial plateau stress fracture, but not lateral.
This fracture type most frequently occurs in soldiers and marathon runners[1,2]. In our series, thirteen of 14 cases were recreational runners. Running has positive effects on physical fitness including reduction in the incidence of obesity, cardiovascular disease, and the other chronic health problems. On the other hand, more people may sustain a running-related injury of the lower extremity. Physicians should be aware of a stress fracture at the medial tibial plateau when patients, particularly runners, present with medial knee pain. Tibial plateau stress fractures in athletes or soldiers are usually self-limiting disease without any persistent deformities because they are comparatively young and they do not have osteoporosis. In fact, all of the present cases did not have any changes of tibial plateau morphology in the follow-up X-rays. On the other hand, insufficiency fractures of the tibial plateau caused by osteoporosis, steroid-use, and rheumatoid arthritis occur in elderly patients[17,18]. We believe that BMD should be evaluated for older runners because delayed diagnosis and treatment can lead to deformity of the knee if osteoporosis is more severe.
One of the limitations of the present study is a small number of the patients because of its rarity. The second limitation is an insufficient length of the tibia on MRI because we used the knee MRI to measure the tibial and medial slopes, which includes only proximal one-third of the whole tibia. MR images of whole tibia might result in more precise slope measurements.
In conclusion, we found three distinct location types of isolated stress fractures of the medial tibial plateau based on MRI. MRI is the preferred technique to correctly diagnose these fracture types because X-rays might not detect the fracture for two week after the onset. Other modalities, such as ultrasound or CT, may be considered as alternatives to diagnose to tibial plateau stress fractures[4]. At that time, tibial posterior slope could serve as an indicator to find out the fracture location at the medial tibial plateau.
We are grateful to Dr. Abdelhakim Ezzat Montasser Marie, Department of Orthopedic surgery, Ogori Daiichi General Hospital, for his critical review of the manuscript.
Stress fractures of the lower extremity commonly occur in athletes and military personnel. The tibial shaft is the most common location for stress fractures during running and marching activities, whereas the medial tibial plateau is a relatively uncommon site. This fracture type is difficult to detect on initial roentgenograms at the onset of symptoms. This injury is easily misdiagnosed because the location of pain and tenderness is very similar to the meniscal injury and pes anserinus bursitis, which are common problems in running activities.
Bone scintigraphy, computed tomography (CT), and magnetic resonance imaging (MRI) are widely used for early detection of stress fractures. Among them, MRI has been found to be more sensitive than CT and more specific than scintigraphy. T2- and STIR-MR images are useful for detecting edema of the cancellous bone that usually presents as a linear fracture line at the medial tibial plateau. No studies have investigated more detailed MRI features of medial tibial plateau stress fractures.
The authors found three different types of location in stress fracture of the medial tibial plateau. The geometry of the tibial plateau in patients with stress fractures of medial tibial plateau and the relationship with the fracture location were also evaluated.
The authors found three distinct location types of isolated stress fractures of the medial tibial plateau based on MRI. Other modalities may be considered as alternatives to diagnose to tibial plateau stress fractures. Tibial posterior slope could serve as an indicator to find out the fracture location at the medial tibial plateau.
It is a very interesting study. The authors present a series of patients with imaging regarding stress fractures of the tibial plateau.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Baldwin K, Drosos GI, Emara KM, Tawonsawatruk T S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Engber WD. Stress fractures of the medial tibial plateau. J Bone Joint Surg Am. 1977;59:767-769. [PubMed] [DOI] [Full Text] |
| 2. | Harolds JA. Fatigue fractures of the medial tibial plateau. South Med J. 1981;74:578-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Gaeta M, Minutoli F, Scribano E, Ascenti G, Vinci S, Bruschetta D, Magaudda L, Blandino A. CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology. 2005;235:553-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 167] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 4. | Khy V, Wyssa B, Bianchi S. Bilateral stress fracture of the tibia diagnosed by ultrasound. A case report. J Ultrasound. 2012;15:130-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Kurklu M, Ozboluk S, Kilic E, Tatar O, Ozkan H, Basbozkurt M. Stress fracture of bilateral tibial metaphysis due to ceremonial march training: a case report. Cases J. 2010;3:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Vossinakis IC, Tasker TP. Stress fracture of the medial tibial condyle. Knee. 2000;7:187-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Wall J, Feller JF. Imaging of stress fractures in runners. Clin Sports Med. 2006;25:781-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Hashemi J, Chandrashekar N, Gill B, Beynnon BD, Slauterbeck JR, Schutt RC, Mansouri H, Dabezies E. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90:2724-2734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 354] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 9. | Bedi A, Kelly NH, Baad M, Fox AJ, Brophy RH, Warren RF, Maher SA. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010;92:1398-1408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 216] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 10. | Wang H, Chen T, Torzilli P, Warren R, Maher S. Dynamic contact stress patterns on the tibial plateaus during simulated gait: a novel application of normalized cross correlation. J Biomech. 2014;47:568-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Chiu KY, Zhang SD, Zhang GH. Posterior slope of tibial plateau in Chinese. J Arthroplasty. 2000;15:224-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 111] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Genin P, Weill G, Julliard R. [The tibial slope. Proposal for a measurement method]. J Radiol. 1993;74:27-33. [PubMed] |
| 13. | Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467:2066-2072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 268] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 14. | Matsuda S, Miura H, Nagamine R, Urabe K, Ikenoue T, Okazaki K, Iwamoto Y. Posterior tibial slope in the normal and varus knee. Am J Knee Surg. 1999;12:165-168. [PubMed] |
| 15. | Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 523] [Cited by in RCA: 572] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 16. | Mizuta H, Takagi K, Sakata H. An unusual stress fracture of the lateral tibial plateau. Arch Orthop Trauma Surg. 1993;112:96-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Manco LG, Schneider R, Pavlov H. Insufficiency fractures of the tibial plateau. AJR Am J Roentgenol. 1983;140:1211-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Prasad N, Murray JM, Kumar D, Davies SG. Insufficiency fracture of the tibial plateau: an often missed diagnosis. Acta Orthop Belg. 2006;72:587-591. [PubMed] |