Published online May 18, 2017. doi: 10.5312/wjo.v8.i5.436
Peer-review started: October 11, 2016
First decision: November 14, 2016
Revised: February 7, 2017
Accepted: February 28, 2017
Article in press: March 2, 2017
Published online: May 18, 2017
Processing time: 214 Days and 12.9 Hours
The aim of this paper is to report an exceptional case of multiple internal exostoses of the ribs in a young patient affected by multiple hereditary exostoses (MHE) coming to our observation for chest pain as the only symptom of an intra-thoracic localization. A 16 years old patient with familiar history of MHE came to our observation complaining a left-sided chest pain. This pain had increased in the last months with no correlation to a traumatic event. The computed tomography (CT) scan revealed the presence of three exostoses located on the left third, fourth and sixth ribs, all protruding into the thoracic cavity, directly in contact with visceral pleura. Moreover, the apex of the one located on the sixth rib revealed to be only 12 mm away from pericardium. Patient underwent video-assisted thoracoscopy with an additional 4-cm mini toracotomy approach. At the last 1-year follow-up, patient was very satisfied and no signs of recurrence or major complication had occured. In conclusion, chest pain could be the only symptom of an intra-thoracic exostoses localization, possibly leading to serious complications. Thoracic localization in MHE must be suspected when patients complain chest pain. A chest CT scan is indicated to confirm exostoses and to clarify relationship with surrounding structures. Video-assisted thoracoscopic surgery can be considered a valuable option for exostoses removal, alone or in addiction to a mini-thoracotomy approach, in order to reduce thoracotomy morbidity.
Core tip: This is a report of an exceptional case of multiple internal exostoses of the ribs in a young patient affected by multiple hereditary exostoses observed for chest pain as symptom of an intra-thoracic localization. Chest pain could be the only symptom of an intra-thoracic localization, possibly leading to serious complications. Thoracic localization must be suspected when patients complain chest pain. Computed tomography scan in indicated to confirm exostoses and to clarify relationship with surrounding structures. Video-assisted thoracoscopy surgery can be considered a valuable option for exostoses removal, alone or in addiction to a mini-thoracotomy approach, in order to reduce thoracotomy morbidity.
- Citation: Mazza D, Fabbri M, Calderaro C, Iorio C, Labianca L, Poggi C, Turturro F, Montanaro A, Ferretti A. Chest pain caused by multiple exostoses of the ribs: A case report and a review of literature. World J Orthop 2017; 8(5): 436-440
- URL: https://www.wjgnet.com/2218-5836/full/v8/i5/436.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i5.436
The aim of this paper is to report an exceptional case of multiple internal exostoses of the ribs in a young patient affected by multiple hereditary exostoses (MHE), who came to our observation complaining chest pain as the only symptom of an intra-thoracic localization. MHE is also known as diaphyseal aclasia, osteochondromatosis or multiple osteochondroma. It is an autosomal dominant disorder with growth plate-like exostoses next to long bones and other skeletal elements.
Usually, all affected individuals are diagnosed by age 12 years, but the median age of diagnosis is three years. The risk for malignant degeneration to osteochondrosarcoma increases with age[1].
The diagnosis of MHE is based on clinical-radiographic results of multiple exostoses in members of a family. The two genes involved are known to cause MHE are EXT1 and EXT2. Mutations in both EXT1 and EXT2 are detected in 70%-95% of affected individuals[2]. Exostoses of the rib are extremely rare, contributing to approximately 1% of all exostoses in MHE[3-5]. We report the case of a patient, complaining only chest pain, affected by MHE with three exostoses protruding directly into the thoracic cavity.
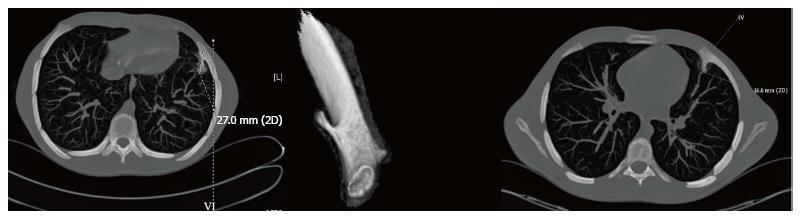
A 16 years old patient with familiar history of MHE, came to our observation for a right sided knee-pain caused by an exostoses of the distal femur irritating the surrounding aponeurotic structures. The patient had undergone several surgical procedures for exostoses removal on both femur, tibia and fibula, left radius and fourth finger of the right hand, all performed by our Unit. During physical examination, patient reported even having a left-sided chest pain. This pain had increased in the last months with no correlation to a traumatic event and was exacerbated by physical activity and cough. Palpation didn’t reveal any subcutaneous swelling. There was no sign of coughing, sputum, nausea, tremor or fever and his laboratory values were all normal. The chest x-ray revealed the presence of three exostoses located on the right second and twelfth and on the tenth left ribs, not related to the pain complained by the patient. We therefore performed a computed tomography (CT) (Figure 1) of the chest with 3-dimension reconstruction which even showed the presence of three exostoses on the left third, fourth and sixth ribs. All the three exostoses protruded into the thoracic cavity, directly in contact with visceral pleura. Moreover, the apex of the one located on the sixth rib revealed to be only 12 mm away from pericardium. Because of symptoms complained by the patient and the particular location of exostoses with potential serious complication, we therefore decided for surgical intervention.
The patient received general anesthesia. Unilateral ventilation with a tidal volume of 300 mL was obtained using a double-lumen endotracheal tube.
A lateral decubitus position was used and a 4-cm long mini-thoracotomy incision was performed at the fifth intercostal space in addition to a standard thoracoscopic portal at the eighth intercostal space in order to completely resect exostoses avoiding recurrence and organ injury.
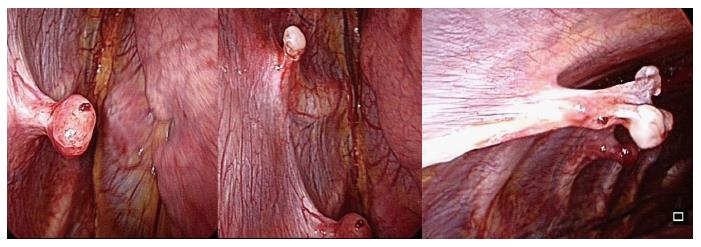
The surgeon identified by thoracoscopy three significant exostoses originating from the ribs within the left side of the chest (Figure 2); one of them hurt the pericardium during cardiac pulsations, as visualized under unilateral right ventilation after exclusion of the left lung. This scratching caused a thickening of the adjacent pericardium and visceral. Each exostoses were completely resected using a chisel and the specimens obtained were sent to the pathologist. In the apex of the chest cavity a single thoracotomy tube was inserted and positioned.
The incisions were closed and the lung was re-expanded to evaluate correct ventilation. The postoperative course was ordinary, and the patient was discharged on the seventh postoperative day. Pathological examination of the specimens obtained were consistent for exostoses, measuring 2 cm in length and 1 cm in width in the third rib, in the fourth one 2 cm in length and 0.5 cm in width and in the sixth one 2.5 cm in length and 1.5 cm in width (Figure 3). At the last 1-year follow-up, patient was very satisfied and no signs of recurrence or major complication had occurred.
The most common localization of exostoses is distal femur, proximal tibia, fibula and humerus, bones that develop from cartilage. Angular deformities, leg-length inequalities and pain resulting from inflammation of skin, tendons or nerves often require surgery.
The flat bones like iliac and scapula are less frequently involved. Rarely ribs, spine, metatarsals, metacarpals, phalanges are involved[1]. Costal exostoses may be difficult to recognize on the chest using only X-ray and the chest CT scan is usually suitable[3-5]. Malignant transformation is seen in 0.5%-5% cases of MHE. Axial sites as ribs, spine, pelvic hips and shoulder are sites of increased risk of malignant transformation. Average age at malignant transformation in MHE is 25-30. It is rare before 20 years of age.
Generally, exostoses grow and gradually ossify during skeletal growth and stop growing with skeletal maturity. The proportion of individuals with MHE who have clinical symptoms rises from approximately 5% at birth to 96% at age 12 years[1].
MHE doesn’t require therapy in the absence of clinical symptoms, but it should be recommended in selected patients. Despite several studies exist in literature regarding costal exostoses, only few Authors have reported surgical management and outcomes of intra-thoracic localization (Table 1).
| Ref. | Year | Age | No. of exostoses | Procedure | Outcomes |
| [6] | 1980 | 9 | 1 | Thoracotomy | Good |
| [7] | 1981 | 20 | 1 | Thoracotomy | Good |
| [8] | 1989 | 7 | 1 | Thoracotomy | Good |
| [9] | 1990 | 14 | 1 | Thoracotomy | Good |
| [10] | 1993 | 19 | 1 | Thoracotomy | Good |
| [11] | 1994 | 36 | 1 | Thoracotomy | Good |
| [12] | 1994 | 3 | 1 | Thoracoscopy | Good |
| [13] | 1997 | 19 | 1 | Thoracotomy | Good |
| [14] | 1998 | 15 | 1 | Thoracotomy | Good |
| [15] | 1997 | 17 | 1 | Thoracoscopy | Good |
| [16] | 2001 | 21 | 1 | Thoracotomy | Good |
| [17] | 2005 | 6 | 3 | Thoracoscopy | Good |
| [4] | 2005 | 15 | 1 | Thoracotomy | Good |
| [18] | 2005 | 11 | 1 | Thoracotomy | Good |
| [19] | 2006 | 14 | 1 | Thoracotomy/thoracoscopy | Good |
| [20] | 2008 | 17 | 2 | Thoracotomy | Good |
| 15 | 1 | Thoracotomy | Good | ||
| 23 | 2 | Thoracotomy | Good | ||
| 12 | 1 | Thoracotomy | Good | ||
| 3 | 1 | Thoracotomy | Good | ||
| [21] | 2009 | 15 | 1 | Thoracoscopy | Good |
| [22] | 2009 | 16 | 1 | Thoracoscopy | Good |
| [23] | 2010 | 17 | 1 | Thoracoscopy | Good |
| [3] | 2011 | 14 | 2 | Thoracotomy | Good |
| 6 | 2 | Thoracotomy | Good | ||
| [24] | 2012 | 25 | 1 | Thoracotomy/thoracoscopy | Good |
| [25] | 2013 | 2 | 1 | Thoracotomy | Good |
| [26] | 2013 | 5 | 1 | Thoracoscopy | Good |
| [27] | 2012 | 21 | 1 | Thoracotomy/thoracoscopy | Good |
| [28] | 2014 | 16 | 2 | Thoracoscopy | Good |
| [29] | 2014 | 15 | 1 | Thoracotomy | Good |
| 5 | Multiple intra/extrathoracic | Thoracotomy | Good | ||
| [30] | 2015 | 18 | 1 | Thoracoscopy | Good |
Most of the cases described concern about a single exostoses, alone or associated to MHE, while very few papers report the management of multiple intra-thoracic exostoses[3,16,19,27,28]. The majority of cases were treated with a thoracotomy approach, with an increase of less invasive surgery such as video-assisted thoracoscopy in the last two decades[12,15,17,21-23,26,28,30]. However, some Authors have underlined the needs of an additional mini-thoracotomy incision depending on the localization of rib involvement and the dimension of the exostoses[19,24,27]. Therefore, considering our case, we sought to completely resect exostoses avoiding recurrence and organ injury preferring a 4-cm mini-thoracotomy approach instead of an additional standard thoracoscopic portal.
The outcomes of surgical management were favorable in all previously reported cases with no significant complications, as in our case. Only Cowles et al[17] reported a persistent post-operative pneumothorax related to a malfunction of chest drainage system, resolved without consequence[17].
Interestingly, in most of the cases reported the diagnosis was made due to complication, potentially fatal, caused by interference with surrounding structures, as was the choice to surgically treat the exostoses. On the contrary, only two cases are described in literature with pain caused by intra-thoracic localization of exostoses as the only reason for exostoses removal[14,29], as in our case.
The patient described in this report revealed only chest pain, but localization and dimension of exostoses could have had a possible risk of dangerous thoracic organ damage or risk of haemothorax due to traumas or vascular wound directly caused by the tip of the exostoses, as widely reported in literature.
Chest pain could be the only symptom of an intra-thoracic exostoses localization, possibly leading to serious complications. Thoracic localization in MHE must be suspected when patients complain chest pain. A chest CT scan is indicated to confirm exostoses and to clarify relationship with surrounding structures. Video-assisted thoracoscopic surgery can be considered a valuable option for exostoses removal, alone or in addiction to a mini-thoracotomy approach, in order to reduce thoracotomy morbidity.
The patient, a 16 years old Caucasian male, reported having a left-sided chest pain, increased in the last months with no correlation to a traumatic event and was exacerbated by physical activity and cough.
Palpation don’t showed evidence of any subcutaneous swelling and there was no sign of coughing, sputum, vomiting, palpitation or fever.
Neuropathic pain, rib fracture, pneumothorax, haemothorax, pneumonia, pleuritis, chest or pleural or lung neoplastic process were excluded by the clinical and objective sign, laboratory tests and imaging.
Hemoglobin level, hematocrit, electrolytes, liver enzymes and coagulation parameters were all normal.
The chest X-ray and computed tomography (CT) revealed the presence of three exostoses located on the right second and twelfth and on the tenth left ribs, not related to the pain complained and other of the three exostoses on the left third, fourth and sixth ribs.
The imaging suggested the diagnosis of multiple exostoses of the rib and it was confirmed after the surgical excision by the pathological examination of the speciments.
All the exostoses were removed by a thoracoscopy approach with a chisel.
Costal exostoses may be difficult to recognize on the chest X-ray. The chest CT scan is usually useful for diagnosis and malignant transformation is seen in 0.5%-5% cases of multiple hereditary exostoses (MHE).
MHE, also known as Multiple Osteochondroma, Osteochondromatosis and Diaphyseal Aclasia, is an autosomal dominant disorder characterized by formation of ectopic, cartilage-capped, growth plate-like exostoses next to long bones and other skeletal elements.
Thoracic localization in MHE can be suspected when patients complain chest pain and a chest CT scan is indicated to confirm exostoses and to clarify relationship with surrounding structures.
This is an interesting and well presented case report of a rare genetic disease.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Leithner A, Sicari R S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Bovée JV. Multiple osteochondromas. Orphanet J Rare Dis. 2008;3:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 200] [Cited by in RCA: 206] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 2. | Zak BM, Schuksz M, Koyama E, Mundy C, Wells DE, Yamaguchi Y, Pacifici M, Esko JD. Compound heterozygous loss of Ext1 and Ext2 is sufficient for formation of multiple exostoses in mouse ribs and long bones. Bone. 2011;48:979-987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Assefa D, Murphy RC, Bergman K, Atlas AB. Three faces of costal exostoses: case series and review of literature. Pediatr Emerg Care. 2011;27:1188-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Pham-Duc ML, Reix P, Mure PY, Pracros JP, Moreux N, Bellon G. Hemothorax: an unusual complication of costal exostosis. J Pediatr Surg. 2005;40:e55-e57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Chazono M, Masui F, Kawaguchi Y, Hazama H, Ueda J, Saito S, Ito Y, Kasama K, Liu K, Marumo K. Dumbbell-shaped osteochondroma of the fifth rib causing spinal cord compression. J Orthop Sci. 2009;14:336-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Propper RA, Young LW, Wood BP. Hemothorax as a complication of costal cartilaginous exostoses. Pediatr Radiol. 1980;9:135-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Camera A, Potter RT, Siegel M. Hemothorax: unusual complication of hereditary multiple exostosis. N Y State J Med. 1981;81:243-244. [PubMed] |
| 8. | Teijeira FJ, Baril C, Younge D. Spontaneous hemothorax in a patient with hereditary multiple exostoses. Ann Thorac Surg. 1989;48:717-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Reynolds JR, Morgan E. Haemothorax caused by a solitary costal exostosis. Thorax. 1990;45:68-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Castells L, Comas P, González A, Vargas V, Guardia J, Gifré L. Case report: haemothorax in hereditary multiple exostosis. Br J Radiol. 1993;66:269-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Harrison NK, Wilkinson J, O’Donohue J, Hansell D, Sheppard MN, Goldstraw PG, Davison AG, Newman Taylor AJ. Osteochondroma of the rib: an unusual cause of haemothorax. Thorax. 1994;49:618-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Tomares SM, Jabra AA, Conrad CK, Beauchamp N, Phoon CK, Carroll JL. Hemothorax in a child as a result of costal exostosis. Pediatrics. 1994;93:523-525. [PubMed] |
| 13. | Uchida K, Kurihara Y, Sekiguchi S, Doi Y, Matsuda K, Miyanaga M, Ikeda Y. Spontaneous haemothorax caused by costal exostosis. Eur Respir J. 1997;10:735-736. [PubMed] |
| 14. | Cottalorda J, Stephan JL, Varlet F, Maatougui K, Chavrier Y. [Intra-thoracic costal sites of osteogenic exostoses in the child]. Rev Chir Orthop Reparatrice Appar Mot. 1998;84:563-566. [PubMed] |
| 15. | Simansky DA, Paley M, Werczberger A, Bar Ziv Y, Yellin A. Exostosis of a rib causing laceration of the diaphragm: diagnosis and management. Ann Thorac Surg. 1997;63:856-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Buchan KG, Zamvar V, Mandana KM, Nihal E, Kulatilake P. Juxtacardiac costal osteochondroma presenting as recurrent haemothorax. Eur J Cardiothorac Surg. 2001;20:208-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Cowles RA, Rowe DH, Arkovitz MS. Hereditary multiple exostoses of the ribs: an unusual cause of hemothorax and pericardial effusion. J Pediatr Surg. 2005;40:1197-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Jin W, Hyun SY, Ryoo E, Lim YS, Kim JK. Costal osteochondroma presenting as haemothorax and diaphragmatic laceration. Pediatr Radiol. 2005;35:706-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Abdullah F, Kanard R, Femino D, Ford H, Stein J. Osteochondroma causing diaphragmatic rupture and bowel obstruction in a 14-year-old boy. Pediatr Surg Int. 2006;22:401-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Kim S, Lee S, Arsenault DA, Strijbosch RA, Shamberger RC, Puder M. Pediatric rib lesions: a 13-year experience. J Pediatr Surg. 2008;43:1781-1785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Kuo SM, Chen KC, Diau GY, Hua YM. Dangerous costal exostosis: hemothorax mimicking empyema in a child. J Pediatr. 2010;156:853, 853.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Asmat A, Tam J. Spontaneous haemothorax from an osteochondroma. Eur J Cardiothorac Surg. 2009;36:394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Khosla A, Parry RL. Costal osteochondroma causing pneumothorax in an adolescent: a case report and review of the literature. J Pediatr Surg. 2010;45:2250-2253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Rolli L, Ampollini L, Carbognani P, Rusca M. Intrathoracic costal exostosis. Eur J Cardiothorac Surg. 2012;42:1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Pelc HJ, Walker J, Davies G. Successful operative management of an asymptomatic chest lesion in hereditary multiple exostosis. J Pediatr Orthop B. 2013;22:505-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Huang HR, Lin TY, Wong KS. Costal exostosis presenting with hemothorax: report of one case. Eur J Pediatr. 2006;165:342-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Nakano T, Endo S, Nokubi M, Tsubochi H. Hemothorax caused by a solitary costal exostosis. Ann Thorac Surg. 2009;88:306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Imai K, Suga Y, Nagatsuka Y, Usuda J, Ohira T, Kato H, Ikeda N. Pneumothorax caused by costal exostosis. Ann Thorac Cardiovasc Surg. 2014;20:161-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Bakhshi H, Kushare I, Murphy MO, Gaynor JW, Dormans JP. Chest wall osteochondroma in children: a case series of surgical management. J Pediatr Orthop. 2014;34:733-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 30. | Rodrigues JC, Mathias HC, Lyen SM, Mcalindon E, Bucciarelli-Ducci C, Batchelor TJ, Hamilton MC, Manghat NE. A Novel Cause of Acute Coronary Syndrome Due to Dynamic Extrinsic Coronary Artery Compression by a Rib Exostosis: Multimodality Imaging Diagnosis. Can J Cardiol. 2015;31:1303.e9-1303.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |