Published online May 18, 2017. doi: 10.5312/wjo.v8.i5.424
Peer-review started: October 10, 2016
First decision: November 11, 2016
Revised: January 3, 2017
Accepted: February 8, 2017
Article in press: February 13, 2017
Published online: May 18, 2017
Processing time: 214 Days and 16.3 Hours
To systematically search literature and determine a preferable surgical procedure in patients with failed conservative treatment of calcifying tendinitis of the shoulder.
The electronic online databases MEDLINE (through PubMed), EMBASE (through OVID), CINAHL (through EB- SCO), Web of Science and Cochrane Central Register of Controlled Trials were systematically searched in May 2016. Eligible for inclusion were all available studies with level II and level III evidence (LoE). Data was assessed and extracted by two independent review authors using a specifically for this study designed data extraction form.
Six studies (294 surgically treated shoulders) were included in this review. No significant differences between the three available treatment options (acromioplasty with the removal of the calcific deposits, acromioplasty or solely the removal of the calcific deposits) were detected regarding the functional and clinical outcome. The follow-up ranged from 12 mo to 5 years. Complication rates were low. No reoperations were necessary and the only reported complication was adhesive capsulitis, which in all cases could be treated conservatively with full recovery.
We found that all three available treatment options show good functional and clinical outcomes in the short and midterm. However, a favorable procedure is difficult to determine due to the lack of high-quality comparing studies.
Core tip: All three available surgical treatment options (acromioplasty with the removal of the calcific deposits, acromioplasty or solely the removal of the calcific deposits) show good functional and clinical results and low complication rates. However, more high-quality comparative research is needed to appoint a preferential procedure.
- Citation: Verstraelen FU, Fievez E, Janssen L, Morrenhof W. Surgery for calcifying tendinitis of the shoulder: A systematic review. World J Orthop 2017; 8(5): 424-430
- URL: https://www.wjgnet.com/2218-5836/full/v8/i5/424.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i5.424
Calcifying tendinitis (CT) of the shoulder is a common disease. It is one the most frequent causes of non-traumatic shoulder pain and has a high disease burden. In a healthy population the incidence of subacromial calcific deposits is 2.7%[1]. In patients with shoulder complaints this number rises to 6.8%. CT mainly affects individuals between 30 and 60 years of age. Males and females are equally affected[1-3]. The calcific deposits are most frequently (80%) seen in the supraspinatus tendon, at a typical location of 1.5 to 2.0 cm of its insertion on the major tuberculum. CT is primarily treated conservatively, though in about 10% of the cases this fails. Then often surgery is a last resort. The etiology of CT remains unclear and is still a matter of dispute. Some authors state that CT is not related to subacromial impingement[2]. This is supported by the histological finding in the study of Uhthoff et al[4]. In this study only minimal signs of inflammation in the rotator cuff of patients with CT were seen. Conversely, other authors observed that there was neovascularization and influx of phagocytes around the calcific deposits. As they state this could lead to subsequent edema of the rotator cuff and an increase of the intratendinous pressure. This theoretically can lead to secondary subacromial impingement as the thickened and calcified tendon decreases the subacromial space. Others state that impingement causes rotator cuff tendinitis, which when chronically apparent leads to CT, due to decreased local oxygen tension or hypoxia[1,2,5,6].
There are several surgical procedures available, mostly in accordance with the above-mentioned theories. In the current orthopedic literature three major surgical strategies have been postulated. The first is an acromioplasty in combination with removal of the calcific deposits, the second is an acromioplasty without removing the calcific deposits and the third surgical procedure is to solely debride the calcific deposits and leave the acromion untouched. However, there is still some debate what is the most preferable procedure. It remains unclear whether the calcific deposits need to be, completely or partially, removed and if an additional acromioplasty is beneficial.
Therefore, the objective of this study is to determine if there is a preferable surgical procedure in patients with conservative treatment resistant CT. We performed a systematic review with two clear research questions: (1) Is there a difference in functional and clinical outcomes after debridement of the calcifications in comparison with debridement and additional acromioplasty on the short- and mid-term; and (2) Is there a difference in the functional and clinical outcomes after acromioplasty compared to acromioplasty with debridement of the calcifications on the short- and mid-term?
This review was performed and written down following the principles of the PRISMA statement[7]. Five relevant electronical databases (MEDLINE through PubMed, EMBASE through OVID, CINAHL through EBSCO, Web of Science and Cochrane Central Register of Controlled Trials) were systematically searched by one review author (FV) in May 2016 for studies in English, German and Dutch. Furthermore, the reference lists of the included articles and available reviews were crosschecked for possible relevant studies. The search was set up using a PICO format [patient (or disease), intervention (drug or treatment), comparison (another drug of treatment) and outcome], from which search terms were deduced, as can be seen in Table 1. Studies eligible for inclusion were Level of Evidence (LoE) II (randomized controlled trials) and LoE III (comparative cohort studies) that compared different surgical procedures for CT of the shoulder. From the selected articles, the authors, their institutions and the journal name were masked, a few weeks before data assessment took place.
| Population | Patients with radiographically confirmed symptomatic tendinitis calcarea of the shoulder (search terms: Shoulder joint, rotator cuff, shoulder, supraspinatus, infraspinatus, subscapular or teres, impingement syndrome, tendinopathy, tendonitis or tendinitis, tendinosis, calcinosis, calcifying, calcification, calcified, calcific, calcarea) |
| Intervention | Surgery (search terms: Surgery, surgical, orthopaedic surgery, shoulder surgery, acromioplasty, debridement, bursectomy, arthroscopic, Neer) |
| Comparison | Surgery (search terms: Surgery, surgical, orthopaedic surgery, shoulder surgery, acromioplasty, debridement, bursectomy, arthroscopic, Neer) |
| Outcome | Functional and clinical outcome |
| Limits | Language: English, German, Dutch Publication year: 1996-2016 Human |
Risk of bias and the quality of the included studies were assessed independently by two authors (FV, EF). The included RCTs and quasi-RCTs were assessed using the 12 quality criteria of Furlan et al (2008). High-Quality was defined as a “yes” score in ≥ 50% of all items[8]. The non-randomized studies were assessed using the Newcastle-Ottawa assessment scale[9]. Disagreements were resolved by consensus, or when necessary a third review author (JWM) was consulted. Data was independently extracted by two reviewers (FV, EF) and crosschecked for accuracy. The reviewers were blinded to the authors of the included articles, their institutions, and the journals in which they were published. Data from each individual study was extracted in a standardized way using a specifically designed extraction form (appendix 1 in supplemental material). Discrepancies were resolved by scrutinizing the original article until a consensus was reached. Extracted data included information such as inclusion and exclusion criteria, inclusion period, method of randomization, specific characteristics of the patient groups, specific surgical information, primary and secondary outcomes, baseline characteristics, statistics used, results and complications (appendix 2 in supplemental material). In case of missing information, we tried to contact the authors of the identified studies.
Whenever possible data was pooled. When pooling was not possible, due to clinical heterogeneity of the included studies based on the included intervention and/or study population, data is presented in a quality synthesis.
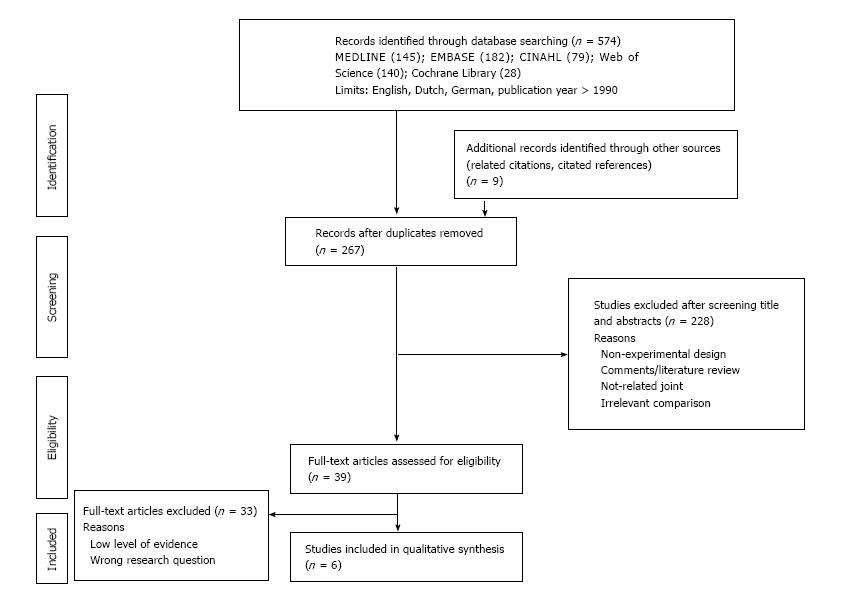
Using the above-mentioned search strategy (appendix 3 in supplemental material) 574 potential relevant studies were identified (Figure 1); of which 267 remained after removing the duplicates. After screening of the titles and abstracts 228 studies were excluded. The main reasons for exclusion were that the studies did not concern the shoulder, were non-experimental studies, or made an irrelevant comparison. The full-texts were read in 39 studies. Finally, 6 studies were included in this review, concerning 294 surgically treated shoulders with CT.
Study characteristics of the included studies are summarized in Table 2. Of these 6 studies there were two were RCTs (118 participants), one quasi-RCT (40 participants) and three comparative cohort studies (136 participants). The data could not be pooled because of the incompleteness of the extracted data and owing to the diversity in timing of the outcome moments (range, 6 wk-5 years).
| Ref. | Study design (LoE) | Population | Mean age (range) | Duration of symptoms in months (range) | Interventions | Outcome measures | Findings | |
| Baseline | Follow-up | |||||||
| Rubenthaler et al[10] | RCT (II) | 38 | 51.1 (-) | - | Arthroscopic debridement + acromioplasty vs Open debridement + acromioplasty | Patte score, VAS, CMS | No significant baseline differences | 16 mo: CMS: 86.0 vs 85.3 (NS) VAS: 1.4 vs 1.8 (NS) Patte score: 84.4 vs 84.6 (NS) |
| Clement et al[11] | RCT (II) | 80 | 49 (32-75) | 6.2 (-) | Arthroscopic debridement + acromioplasty vs arthroscopic debridement | VAS, DASH, CMS, SF-12 | No significant baseline differences | 6 wk: CMS: 62.2 vs 64.1 (NS) DASH: 24.5 vs 24.0 (NS) VAS: 4.4 vs 4.5 (NS) SF-12: 45.7 vs 44.3 (NS) 12 mo: CMS: 82.4 vs 77.5 (NS) DASH: 14.5 vs 14.0 (NS) VAS: 1.6 vs 2.5 (NS) SF-12: 43.0 vs 42.5 (NS) |
| Hofstee et al[12] | Quasi-RCT (III) | 40 | 52.3 (41-62 | 14.5 (6-36) | Arthroscopic debridement + acromioplasty vs arthroscopic debridement | DASH, VAS, satisfaction, ROM | No significant baseline differences | 36 mo: DASH: 3.14 vs 3.04 (NS) VAS: 4.3 vs 4.2 satisfied, yes: 80% vs 75% |
| Marder et al[13] | Retrospective case-control study (III) | 50 | 44 (27-67) | 13 (-) | Arthroscopic debridement vs arthroscopic debridement + acromioplasty | QuickDASH, RTW, UCLA | No significant baseline differences | 6 wk: RTW: 60% vs 20% (P = 0.004) 5 yr: QuickDASH: 6.3 vs 11.1 (NS) VAS: not well recorded UCLA: 32.0 vs 32.4 (NS) |
| Tillander et al[14] | Matched pair analysis (III) | 50 | 50 (40-67) | 66 (12-216) | Arthroscopic acromioplasty in patients with vs without CT | CMS, satisfaction, radiological | No significant baseline differences | 24 mo: CMS: 78 vs 79 (NS) Satisfaction, yes: 72% vs 80% (NS) |
| Maier et al[15] | Comparative cohort study (III) | 36 | 48.9 (29-70) | 35.2 (9-84) | Open debridement vs open debridement + acromioplasty | CMS | No significant baseline differences | 34 mo: CMS: 74.9 vs 73.4 (NS) |
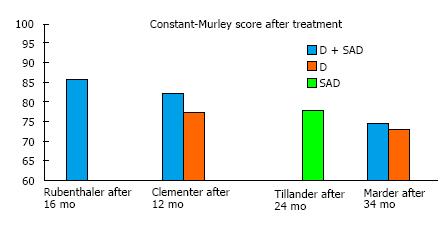
The risk of bias was assessed by two independent review authors (FV, EF). Three studies were evaluated with the 12 criteria of Furlan et al[8], and three studies were evaluated with the Newcastle-Ottawa scale[9]. Two RCTs were assessed as high-quality RCTs (Table 3), whereas in the non-randomized group one study received the maximum score and the other two studies had a near to maximum score (Table 4). Results of the functional outcome are presented using different outcome measures, namely the Constant-Murley score (CMS), Patte score and the University of California-Los Angeles score (UCLA). The results of the clinical outcome are presented with various outcomes measures, including the Disabilities of Arm, Shoulder and Hand score (DASH) and return to work, as can be seen in Table 2.
| Ref. | Adequate randomization? | Allocation concealment? | Blinding patients? | Blinding caregiver? | Blinding outcome assessors? | Incomplete outcome data addressed? dropouts | Incomplete outcome data? ITT-analysis? | No selective outcome reporting? |
| Rubenthaler et al[10] | + | + | + | - | ? | + | - | + |
| Clement et al[11] | + | + | + | - | + | + | - | + |
| Hofstee et al[12] | - | - | ? | - | ? | + | - | + |
The studies of Rubenthaler et al[10], Clement et al[11], Marder et al[12] and Maier et al[13] aided in answering the first research question (Figure 2).
Functional outcome: For the comparison of the functional outcome on the short and midterm only the RCT of Clement et al[11] reported data 6 wk and 12 mo after debridement vs debridement with acromioplasty. They reported no significant difference after 6 wk (mean CMS 62.2 vs 64.1) and 12 mo (mean CMS 82.4 vs 77.5). Rubenthaler et al[10] reported the results after debridement with acromioplasty in an open vs arthroscopic procedure (mean CMS 86.0 vs 85.3). Marder et al[13] and Maier et al[15] reported data of debridement vs debridement with acromioplasty after 5 years and 34 mo, respectively. The mean UCLA of 32.0 vs 32.4 after 5 years did not differ significantly and the mean CMS of 74.9 vs 73.4 after 34 mo did not differ either.
Clinical outcome: The clinical outcome was reported by Clement et al[11] and Marder et al[13] using the DASH score and QuickDASH score. The clinical outcome did not differ significantly in the short and midterm (6 wk: mean DASH 24.5 vs 24.0 and 12 mo: mean DASH 14.5 vs 14.0). After 5 years the mean QuickDASH did not differ significantly either (6.3 vs 11.1).
The studies of Hofstee et al[12] and Tillander et al[14] were helpful in answering the second research question. There was no information available for the comparison of the results in the short term.
Functional outcome: Tillander et al[14] reported results of the functional outcome after 24 mo after solitary acromioplasty in patients with and without CT. The mean CMS was 78.0 and 79.0, respectively. As an indication of the functional outcome Hofstee et al[12] reported the ROM after 36 mo. In all six planes the ROM did not differ significantly between patients after acromioplasty in comparison with patients after acromioplasty with debridement.
Clinical outcome: Hofstee et al[12] reported a DASH score of 3.1 vs 3.0 after 36 mo of surgery which was not significantly different.
Four of the included six studies reported information about adverse events or complications[10,11,13,15]. There were no intraoperative complications reported, none of the included patients required reoperation. The only complication reported was adhesive capsulitis. In the studies of Clement et al[11] and Marder et al[13], one patient (1.3%) and three patients (6%) showed signs of adhesive capsulitis. These patients could all could be treated conservatively and showed full recovery at the end of the follow-up.
CT is often a self-limiting disease which in the majority of the patients can be managed with conservative measures, such as physical therapy, subacromial infiltrations, shock wave therapy or needling. However, in some patients these conservative measures fail and surgery is needed. Based on the results of this systematic review of LoE II and III evidence, we found that all three available treatment options show good functional and clinical outcomes in the short and midterm. However, a favored procedure is difficult to determine due to the lack of high-quality comparing studies.
Regarding the first research question four studies aided in answering this “question”[10,11,13,15]. The functional and clinical outcome did not differ after debridement vs debridement with an additional acromioplasty. It could be postulated that CT is not correlated with subacromial impingement and an acromioplasty does not seem to be beneficial. This supports the aforementioned theory of Gärtner et al[2]. Of the other outcomes extracted from the included studies, only in the study of Marder et al[13] did significantly more patients return to work after six weeks (Table 2). In the included RCT[11] an additional acromioplasty was not found to be beneficial. Though, in this study the (patho)anatomy (e.g., classification of Bigliani[16]) of the acromion was not considered. It has been postulated that if there are any radiological or intraoperative signs of impingement an acromioplasty can be performed[16,17].
The studies of Hofstee et al[12] and Tillander et al[14] aided in answering the second research question. They found good functional and clinical results 24 and 36 mo after an acromioplasty and an acromioplasty with an additional debridement of the calcifications. They found no significant differences. Short term results were not available. Other variables (VAS and satisfaction) also did not differ significantly. These results support the correlation between CT and subacromial impingement. Whereas, this suggests that the complete or partial debridement of the calcific deposits is not necessary.
All three available treatment options are safe; the complication rates are low and the reported complications were treated conservatively and showed full recovery. In the included studies the percentage of adhesive capsulitis was low, comparing to the current literature where rates as high as 18% are reported[18-20]. In the included studies in which a debridement was performed the rotator cuff defect was not sutured afterwards, even though no rotator cuff tears were seen in our entire study population.
Some limitations apply to this systematic review. The main limitation is the lack of high-quality, preferably randomized, comparing trials between the different treatment options. Two high-quality RCTs were included of which one did not make the exact comparison we were interested in. The other one was valuable, however the follow-up was rather short (one year). Therefore, there is a need for more research on this topic. The data could not be pooled due to heterogeneity of the included studies and therefore no quantitative analysis could be made. We analyzed the causes of this heterogeneity. But, we could not improve this sufficiently; therefore data is presented in a narrative fashion. On the other hand, we were able to detect all relevant LoE II and III evidence regarding the surgical treatment options of CT and describe their results in this concise review.
All three available surgical treatment options for patient with conservative therapy resistant CT of the shoulder show good functional and clinical outcome and are safe procedures. Based on this systematic review a preferable treatment option could not be appointed and therefore recommendations cannot be made. Future research should be aimed at comparing all three available options. This is preferably done in a randomized fashion including a short, mid and long term follow-up.
There still is no consensus on what is the best surgical treatment of therapy resistant calcifying tendinitis of the shoulder. Different authors opt different surgical procedures. The authors tried to identify the surgical treatment with the best functional and clinical outcome.
Calcifying tendinitis was probably first diagnosed by Plenk et al in 1953. Up till to today the exact etiology is still unclear. In the majority of the cases the disease resolves spontaneously or with conservative measures. However, sometimes surgery is necessary. Several authors have pointed out the beneficial effect of an additional acromioplasty with the debridement of the calcific deposits.
Although this disease is extensively studied the exact surgical management has not been clarified yet. There were several comparative studies available but Clement et al were in 2015 the first to publish a randomized study on this particular subject. They stated that an additional acromioplasty was not beneficial.
This review suggests that all three available surgical options are safe and effective. However, a preferable could not be appointed.
SAD is a subacromial decompression which is the resection of the anterolateral part of acromion and release of the coracoacromial ligament.
This is a very interesting and well planned study.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: the Netherlands
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cui Q, Fernandez-Fairen M, Guerado E, Rothschild BM S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Diehl P, Gerdesmeyer L, Gollwitzer H, Sauer W, Tischer T. [Calcific tendinitis of the shoulder]. Orthopade. 2011;40:733-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Mouzopoulos G, Stamatakos M, Mouzopoulos D, Tzurbakis M. Extracorporeal shock wave treatment for shoulder calcific tendonitis: a systematic review. Skeletal Radiol. 2007;36:803-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Uhthoff HK, Sarkar K. Classification and definition of tendinopathies. Clin Sports Med. 1991;10:707-720. [PubMed] |
| 5. | Hurt G, Baker CL. Calcific tendinitis of the shoulder. Orthop Clin North Am. 2003;34:567-575. [PubMed] |
| 6. | Speed CA, Hazleman BL. Calcific tendinitis of the shoulder. N Engl J Med. 1999;340:1582-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 129] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47111] [Article Influence: 2944.4] [Reference Citation Analysis (0)] |
| 8. | Furlan AD, Pennick V, Bombardier C, van Tulder M; Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34:1929-1941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1129] [Cited by in RCA: 1260] [Article Influence: 78.8] [Reference Citation Analysis (0)] |
| 9. | Pastorino R, Milovanovic S, Stojanovic J, Efremov L, Amore R, Boccia S. Quality Assessment of Studies Published in Open Access and Subscription Journals: Results of a Systematic Evaluation. PLoS One. 2016;11:e0154217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Rubenthaler F, Ludwig J, Wiese M, Wittenberg RH. Prospective randomized surgical treatments for calcifying tendinopathy. Clin Orthop Relat Res. 2003;278-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Clement ND, Watts AC, Phillips C, McBirnie JM. Short-Term Outcome After Arthroscopic Bursectomy Debridement of Rotator Cuff Calcific Tendonopathy With and Without Subacromial Decompression: A Prospective Randomized Controlled Trial. Arthroscopy. 2015;31:1680-1687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Hofstee DJ, Gosens T, Bonnet M, De Waal Malefijt J. Calcifications in the cuff: take it or leave it? Br J Sports Med. 2007;41:832-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Marder RA, Heiden EA, Kim S. Calcific tendonitis of the shoulder: is subacromial decompression in combination with removal of the calcific deposit beneficial? J Shoulder Elbow Surg. 2011;20:955-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Tillander BM, Norlin RO. Change of calcifications after arthroscopic subacromial decompression. J Shoulder Elbow Surg. 1998;7:213-217. [PubMed] |
| 15. | Maier M, Krauter T, Pellengahr C, Schulz CU, Trouillier H, Anetzberger H, Refior HJ. [Open surgical procedures in calcifying tendinitis of the shoulder - concomitant pathologies affect clinical outcome]. Z Orthop Ihre Grenzgeb. 2002;140:656-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Seil R, Litzenburger H, Kohn D, Rupp S. Arthroscopic treatment of chronically painful calcifying tendinitis of the supraspinatus tendon. Arthroscopy. 2006;22:521-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 110] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Balke M, Bielefeld R, Schmidt C, Dedy N, Liem D. Calcifying tendinitis of the shoulder: midterm results after arthroscopic treatment. Am J Sports Med. 2012;40:657-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 18. | Merolla G, Bhat MG, Paladini P, Porcellini G. Complications of calcific tendinitis of the shoulder: a concise review. J Orthop Traumatol. 2015;16:175-183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 19. | Gosens T, Hofstee DJ. Calcifying tendinitis of the shoulder: advances in imaging and management. Curr Rheumatol Rep. 2009;11:129-134. [PubMed] |
| 20. | ElShewy MT. Calcific tendinitis of the rotator cuff. World J Orthop. 2016;7:55-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |