Published online May 18, 2017. doi: 10.5312/wjo.v8.i5.385
Peer-review started: November 29, 2016
First decision: February 17, 2017
Revised: March 4, 2017
Accepted: March 23, 2017
Article in press: March 24, 2017
Published online: May 18, 2017
Processing time: 167 Days and 12.5 Hours
To measure single baseline deep posterior compartment pressure in tibial fracture complicated by acute compartment syndrome (ACS) and to correlate it with functional outcome.
Thirty-two tibial fractures with ACS were evaluated clinically and the deep posterior compartment pressure was measured. Urgent fasciotomy was needed in 30 patients. Definite surgical fixation was performed either primarily or once fasciotomy wound was healthy. The patients were followed up at 3 mo, 6 mo and one year. At one year, the functional outcome [lower extremity functional scale (LEFS)] and complications were assessed.
Three limbs were amputated. In remaining 29 patients, the average times for clinical and radiological union were 25.2 ± 10.9 wk (10 to 54 wk) and 23.8 ± 9.2 wk (12 to 52 wk) respectively. Nine patients had delayed union and 2 had nonunion who needed bone grafting to augment healing. Most common complaint at follow up was ankle stiffness (76%) that caused difficulty in walking, running and squatting. Of 21 patients who had paralysis at diagnosis, 13 (62%) did not recover and additional five patients developed paralysis at follow-up. On LEFS evaluation, there were 14 patients (48.3%) with severe disability, 10 patients (34.5%) with moderate disability and 5 patients (17.2%) with minimal disability. The mean pressures in patients with minimal disability, moderate disability and severe disability were 37.8, 48.4 and 58.79 mmHg respectively (P < 0.001).
ACS in tibial fractures causes severe functional disability in majority of patients. These patients are prone for delayed union and nonunion; however, long term disability is mainly because of severe soft tissue contracture. Intra-compartmental pressure (ICP) correlates with functional disability; patients with relatively high ICP are prone for poor functional outcome.
Core tip: Anterior and deep posterior compartments are commonly involved in acute compartment syndrome (ACS) of leg after tibial fracture. Assessment of functional outcome in these patients and correlation with deep posterior compartment pressure has never been reported. This study revealed that ACS in tibial fractures causes severe functional disability and about 48% patients were severely disabled at one year. But this study did not find statistically significant relation between fracture union rate and deep compartment pressure value. The intra-compartmental pressure correlates with functional disability. Patients with relatively high pressure are prone for severe residual pain and poor functional outcome.
- Citation: Goyal S, Naik MA, Tripathy SK, Rao SK. Functional outcome of tibial fracture with acute compartment syndrome and correlation to deep posterior compartment pressure. World J Orthop 2017; 8(5): 385-393
- URL: https://www.wjgnet.com/2218-5836/full/v8/i5/385.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i5.385
Acute compartment syndrome (ACS) is an orthopedic emergency which is commonly noticed in leg bones and forearm bones fracture[1-7]. The reported incidence of ACS is around 3% to 10% following tibial fracture. Prompt diagnosis with early fasciotomy to decompress the tense compartment is crucial in preserving the life and limb of the patient in this grave situation[1-7].
Although a constellation of clinical signs and symptoms are taken into consideration for diagnosis of ACS, these are poorly predictive of compartment syndrome and are often difficult to assess in obtunded patients[2,5,6,8-11]. Measurement of the intra-compartmental pressure (ICP) offers an objective method to confirm the clinical suspicion of compartment syndrome. Various techniques for measurement of compartment syndrome are available in the literature and the most widely accepted threshold for surgical intervention is ICP within 30 mmHg of patient’s diastolic blood pressure[12-20]. Adequate and timely fasciotomy is expected to provide good functional and cosmetic results. Delay in decompression of ACS can result in permanent neurological impairment, disabling muscle contractures and delay in fracture union causing severe functional disability[6,8,21-23]. The severity of disability and morbidity, even after fasciotomy in ACS, is dependent on several factors including ICP, time of fasciotomy, adequacy of fasciotomy and demographic profile of the patients[21-23]. Although it is established that anterior and deep posterior compartments are commonly involved in ACS of leg, researchers have used only anterior compartment pressure for diagnosis. Considering the superficial location of anterior compartment, a raised pressure within this compartment may be revealed clinically easily. This may not be true for deep posterior compartment and hence, Matsen et al[24] have warned the orthopaedic surgeons that isolated raised deep posterior compartment pressure may be missed in few patients.
This prospective study was designed to measure at least a single baseline deep posterior compartment pressure in patients of tibial fracture complicated by ACS and to correlate the raised pressures to the functional outcome.
Between May 2010 and October 2012, a prospective study was conducted to evaluate the functional outcome of tibial fractures complicated with ACS. The study also aimed at correlating the outcome with initial deep posterior compartment pressure. Patients of > 18 years old with tibial fracture and clinical suspicion of ACS were recruited in this study after getting their written informed consent. Patients with associated ipsilateral limb injury, vascular injury (Doppler confirmed absent blood flow), poor general status (GCS ≤ 13, patients in shock (SBP < 90 mmHg or MAP < 70 mmHg), pathological fractures or pre-existing disease in the limb (prior surgery, neuromuscular disorders; polio, etc.) were excluded. Institutional ethical committee permission was obtained before recruiting patient in this study.
All patients were evaluated initially by an orthopedic surgeon. Demographic profiles and injury mechanisms were mentioned in a predesigned proforma. Appropriate radiographs were taken to assess the fracture pattern and classified as per OTA classification and Schatzker classification for proximal tibial fractures. Doppler was done to confirm that there was no vascular injury in these patients.
The patients were evaluated clinically for signs and symptoms of ACS by two attending orthopaedic surgeons. If there were any signs or symptoms of ACS, then the deep posterior compartment pressure of the injured leg was measured and documented. The diagnosis of ACS was established if there were at least 3 clinical signs/symptoms (Figure 1), a differential pressure (∆P) of less than 30 mmHg between the diastolic and compartment pressures (McQueen and Court-Brown 1996) or a combination of both clinical and pressure indications. Fasciotomy was performed in patients diagnosed with ACS.
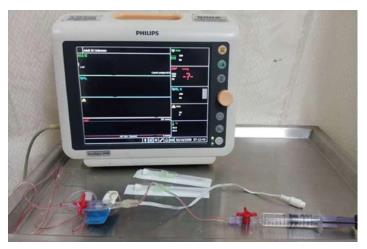
The pressure in the limb was measured in the deep posterior compartment of leg using modified Whiteside’s technique. The patient was positioned supine and limbs flat at rest on the bed. All measurements were made within 5 cm of the level of the fracture[25]. Under strict aseptic conditions a straight cannulated 18-gauge intravenous needle was inserted at an angle of approximately 45° relative to the skin surface skirting the posterior border of tibia to reach the posterior compartment. An arterial-line transducer (PHILIPS V-08) connected to a monitor was placed at the same level as the needle, saline flushed through the system to remove air, and the monitor was kept at zero. Half milliliter of normal saline was injected to allow the compartment to equilibrate with interstitial fluids. Measurement was recorded from the monitor after values were stabilized, usually within 20 to 30 s (Figure 2).
The patients were followed up regularly at an interval of two weeks till the fasciotomy wound was healed. After that they were followed up at 3 mo, 6 mo and one year. Time of clinical (no pain at fracture site with full weight bearing) union and radiological union (bridging trabeculae at the fracture site) and complications encountered during post-operative period were recorded in the predesigned proforma. Fractures which did not unite till 6 mo’ time were considered as delayed union and, if there was no progressive radiological evidence of union for further three consecutive months, it was considered as nonunion (> 9 mo since the time of injury). At the end of one year, the patients were examined particularly for any pain, toe deformity, ankle stiffness, residual paralysis of leg muscles, paraesthesia and limb contracture. Functional limitation of the patient to sit with 90° knee flexion, sitting cross-leg, squatting, walking, running and climbing stairs was evaluated on a Likert-Scale. Overall functional assessment of the limb was done using lower extremity functional scale (LEFS). LEFS score was calculated for each patient using questionnaire and percentage of disability calculated. The mean score was 51.03 (out of 80) corresponding to 63.78% of maximal function. The patients were categorized into five groups of disability based on their percentage of maximal function (LEFS/80 × 100): Bedbound - 0% to 20% score, crippled - 20% to 40% score, severe disability - 40% to 60% score, moderate disability - 60% to 80% score, minimal disability - 80% to 100% score).
Data was analyzed using commercial statistical package SPSS (Version 16, SPSS Inc, Chicago, IL) for MS-Windows. The data summary was presented in a descriptive fashion as mean, standard deviation, skewness and Kurtosis, etc. to describe the clinical characteristics and functional and radiological outcome. The relationship of the radiological union and functional outcome were analyzed and related to the fracture pattern, delay in fasciotomy, pressure threshold and clinical diagnosis of ACS.
Differences between variables were analysed using Pearson’s χ2 test. The strength of association was carried out using Karl Pearson’s or Spearman’s rank correlation coefficient. Various comparisons were made either using independent t-test or analysis of variance (ANOVA). Difference was considered significant with a P value of < 0.05. The statistical review of this study was performed by a biomedical statistician before submission.
Six hundred and three patients with tibial fractures were treated during this period. Of which, 48 patients with ACS met the inclusion criteria; 6 did not consent to participate in the study and data of 10 patients were incomplete. Remaining 32 patients were evaluated to assess functional outcome of ACS of leg. The mean age of the patients was 40.3 years (range, 25 to 64 years). There were 30 males and 2 females. Only one patient presented to us after 72 h of injury and remaining patients presented to our service after an average delay of 9.0 h (median 6.75 h, range 0.25 to 29.5 h). There were 16 diaphyseal and 16 proximal tibial fractures in this study. Among proximal tibial fracture patients, 15 had tibial plateau fracture (10 Schatzker type VI, 3 Schatzker type V, One type IV and one type I) and only one had extra-articular fracture. There were six open fractures and all were Gustilo Anderson type I injury.
Twenty-four patients (75%) had tense palpable swelling and 30 (93.75%) had pain on passive stretch. Paraesthesia and paralysis in the affected limb was noticed in 20 (62.5%) and 21 (65.63%) patients respectively. Three patients (9.38%) had pulselessness and only one patient (3.13%) had pallor in the leg. Clinical diagnosis (3 signs/symptoms) of ACS was established in 20 patients.
The mean ICP of deep posterior compartment of leg was 51.84 mmHg (range 32 to 73 mmHg). All patients had absolute ICP above 30 mmHg, and 26 (81%) patients had ICP above 45 mmHg (Figure 3). Mean differential pressure was (∆P) 23.97 + 13.389; 25 patients (78.1%) had ∆P above 20 mmHg and 15 patients (46.9%) had ∆P above 30 mmHg. Twenty patients had at least 3 clinical signs/symptoms and diagnosed clinically. They all underwent fasciotomy. Twelve patients who did not fit the clinical criteria for ACS had ∆P within 30 mmHg of diastolic pressure, but only 10 patients underwent fasciotomy; among the other two patients, one patient had > 48 h delay and the other showed clinical improvement; hence fasciotomy was avoided in both patients. Both single and double incision fasciotomy was used in equal frequency (15 each).
In our set of patients, there was an asymmetrical distribution for the time delay; therefore we considered median value (5.00 h, mean 7.91 h) for analysis. Seven (21.86%) fractures were definitely fixed at the time of fasciotomy and remaining patients were temporarily stabilized using external fixator (12, 37.5%) or POP (13, 40.6%). Ultimately, three patients had to undergo amputation as a result of complication of ACS and remaining patients were treated with IM nailing (14, 48.3%), plate osteo-synthesis (13, 44.8%) or external fixator (2, 6.9%) as a method of fracture fixation.
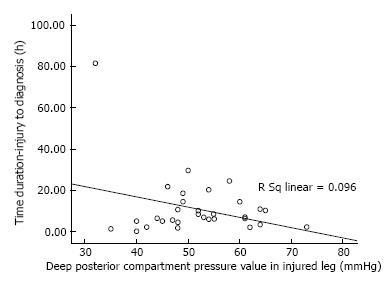
The effect of age on compartment pressure was analyzed by diving the patients into two groups (≥ 35 years and < 35 years). Patients < 35 years old had mean pressure of 52.33 mmHg compared to 51.25 mmHg in older age group (P = 0.777, independent sample t-test). The pressure values were also compared between the two age groups and it was found that older age patients were more within the diagnostic threshold for ACS, though again no statistical difference was seen. Gender, mechanism of injury, open/closed fracture and the site (diaphyseal or proximal tibia) of injury had no effect on pressure values (P > 0.05). We found that ICP was decreasing with the progression of time (Figure 4), contrary to the expectation, with pearson co-efficient -0.310; but it was not statistically significant (P = 0.084).
For follow up and outcome assessment, 3 patients who had to undergo amputation were not considered. Average follow up period was 93.1 wk (range 54 to 123 wk). Average time for clinical union was 25.2 ± 10.9 wk (ranging from 10 to 54 wk) and radiological union was 23.8 ± 9.2 wk (ranging 12 to 52 wk) (Figure 5). Nine patients had delayed union and 2 had nonunion who needed bone grafting to augment healing. Most common complaint at follow up was ankle stiffness (76%), which caused difficulty in walking, running and/or squatting (Tables 1 and 2, Figure 5). Out of 21 patients who had paralysis at diagnosis, 13 (62%) did not recover. Additional 5 patients developed paralysis at follow up even after fasciotomy (Table 1).
| Complication | No. of patients (%) |
| Amputation (n = 32) | 3 (9.4) |
| Infection (fasciotomy wound) | 5 (17.2) |
| Toe deformities (e.g., clawing) | 8 (27.6) |
| Ankle stiffness (affecting function) | 19 (76.0) |
| Residual paralysis (EHL/FHL/ankle DF/ankle PF) | 18 (62.1) |
| Paraesthesia or nerve dysfunction | 3 (10.3) |
| Limb contracture | 5 (17.2) |
| Muscle herniation (fasciotomy site) | 2 (6.9) |
| Pain (apart from fracture site) | 15 (51.7) |
| Others (DVT, limb edema) | 9 (31.0) |
| Function | No. of patients (%) | |
| (n = 29) | (None/mild) | (Moderate/severe) |
| Sitting 90° | 27 (93.1) | 2 (6.9) |
| Cross legged sitting | 22 (75.9) | 7 (24.1) |
| Squatting | 17 (58.6) | 12 (41.4) |
| Walking | 24 (84.8) | 5 (17.2) |
| Running | 13 (48.8) | 16 (55.2) |
| Stair climbing | 19 (65.5) | 10 (34.5) |
On LEFS evaluation, there were 14 patients (48.3%) with severe disability, 10 patients (34.5%) with moderate disability and 5 patients (17.2%) with minimal disability (Table 2).
Six out of 13 (46.2%) proximal tibial fractured patients and 5 out of 16 (31.2%) diaphyseal fractured patients had delayed union or nonunion, statistically no significant difference was observed between the type of fracture (P = 0.706). Eight patients with clinical ACS (3 signs/symptoms) and 3 patients without clinical ACS had delayed union or nonunion. Although it appears that patients diagnosed with clinical ACS had propensity to undergo delayed union or nonunion, there was no statistical difference (P = 0.332). The mean ICP in patients with normal union was 54.36 mmHg and it was 49.48 mmHg in patients with delayed union or nonunion (P = 0.214). So there was no effect of ICP on fracture union. Relatively high ICP was also noted in patients with residual disability and complications, but apart from persistent pain (P = 0.019), none of other group had statistically significant difference in pressures (Table 3).
| Pain | Ankle/toe deformity | Residual paralysis | Running difficulty | Squatting difficulty | |
| Yes | 55.4 (15) | 51.9 (18) | 53.7 (18) | 52.2 (16) | 52.2 (12) |
| No | 47.5 (14) | 51.1 (11) | 48.2 (11) | 50.8 (13) | 51.1 (17) |
| P value | 0.019 | 0.827 | 0.125 | 0.753 | 0.702 |
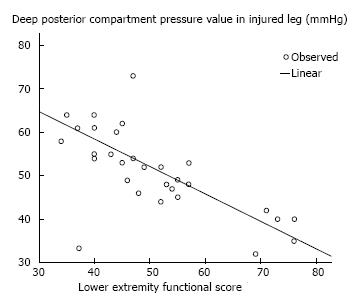
Functional scores were expected to be poor in patients with higher pressure values. The mean LEFS score in our patients was 51 (63.75%) which corresponded to moderate disability. We found pressure values to be higher in patients with lower LEFS score, also there was a negative correlation between the same. Significant difference in pressure was found in LEFS groups (Figure 6). The mean pressures in patients with minimal disability (n = 5), moderate disability (n = 10) and severe disability (n = 13) were 37.8, 48.4 and 58.79 mmHg respectively (one way ANOVA, P < 0.001).
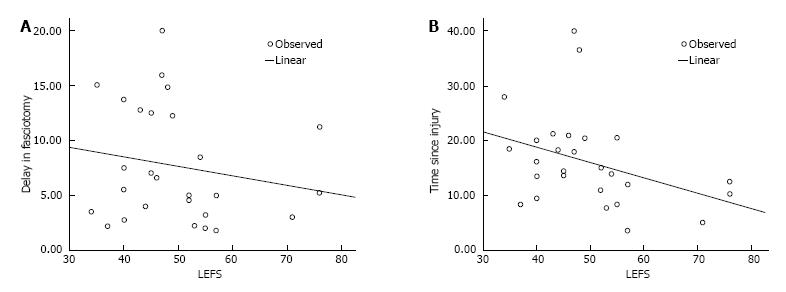
Thirty patients (30/32) had fasciotomy to decompress the compartment and 3 of these eventually ended up with amputation. We considered delay of more than 6 h to be significant and evaluated the outcome of patients. The average delay in fasciotomy was 9.8 h in patients who underwent amputation and 7.7 h in patients who didn’t end up with amputation; but, there was no statistically significant difference in these two groups (independent t-test, P = 0.564). There were 14 patients who were late for > 6 h in fasciotomy; 4 had good functional outcome (LEFS score > 60%) and 10 had poor outcome (LEFS score < 60% or amputation). Among remaining 16 patients who had fasciotomy done within 6 h, 9 patients had good functional outcome and 7 had poor outcome. Although it appears that delay in fasciotomy for more than 6 h effects the eventual functional outcome, it was not statistically significant in this study (Pearson’s χ2 = 2.330, P = 0.159). Both delay in fasciotomy and total time since injury showed negative relationship with LEFS with a slightly better correlation of time from injury to fasciotomy, but it was not statistically significant (Figure 7). No difference was found in single incision and double incision fasciotomy on LEFS outcome (P = 0.856).
ACS in tibial fracture is a serious complication and absence of prompt intervention can cause considerable morbidity or, even mortality[1-7]. Clinical judgment is based on subjective appraisal of the limb condition and there is a risk of missing the diagnosis or getting late. ICP of the anterior compartment has helped the surgeon in establishing the diagnosis. However, some reports have stressed on measurement of deep posterior compartment pressure as this compartment get involve equally or may involve in isolation[25]. In this study, we have evaluated the functional disability of the patient objectively and correlated it with deep posterior compartment pressure.
There are few limitations in this study. The number of patients was small and there was no control group. The technique of compartment measurement was not validated with a standard technique. Only single baseline deep compartment pressure was measured and it was correlated with functional outcome. Despite these limitations, this study has strength as it was based on prospective evaluation of patient and the measuring technique was reliable[26,27]. Several authors have reported that continuous pressure monitoring does not influence outcome in tibial fracture complicated with ACS[8,28-30]. Therefore, single deep posterior compartment pressure measurement was used as an adjunct to diagnosis and the effects of elevated pressure was evaluated. For clinical union, an ability to bear full weight without any pain at the fracture site was considered, however the residual effect of ACS may have some influence on the decision. Because of contracture some patients may have pain on weight bearing and that might have caused a longer clinical union (25 wk) time than the radiological union (24 wk).
Young males with high energy injuries of tibial shaft are prone for development of ACS[1,2,5]. But, we did not observe any statistically significant difference between proximal tibia and tibial shaft fractures. Also, patients < 35 years and older did not have any effect on ACS occurrence, this was because the mean age of our patients was 40 years and there was equal incidence of diaphyseal and proximal tibial fractures; majority (41%) of proximal tibial fractures were high impact injuries with severe comminution (OTA 41C1-3) and open fractures.
Systemic hypotension, vascular injuries and patients with decreased alertness pose difficulty in diagnosing compartment syndrome and interpretation of elevated pressure[6,31], therefore these patients were excluded. Diagnosis of ACS and the decision for fasciotomy was based on clinical judgement without any objective criteria. Ulmer proposed presence of 3 or more clinical symptoms to diagnose ACS[9]. Applying only these criteria, we would have diagnosed only 20 patients with diagnosis of compartment syndrome and missing the remaining patients. The patients usually have different threshold of pain, and clinical symptoms are also variable, thus we used pressure measurement to assess their risk of compartment syndrome. However, absolute ICP was not found to be diagnostic of ACS when considered alone. We found that applying the threshold of pressure difference from diastolic blood pressure (DBP) within 30 mmHg identified ACS in more than 75% cases. Using absolute ICP of 30 mmHg may result in overtreatment. Delta P within 20 mmHg of DBP would have resulted in missing 25%-70% patients of ACS. The duration of onset of compartment syndrome was not possible to predict from the time since injury in this study and we found decrease in compartmental pressure with progression of time. However, decreased LEFS score was found with the progression of time.
The long term functional outcome of ACS in tibial fractures can be evaluated on two broad aspects; first, the impact on fracture-healing and second about the impact on soft tissue leading to contracture. Increase in ICP compromises the perfusion of neuro-muscular tissues causing ischemia and cell death. Initial traumatic micro and macro muscle fibre damage, loss of haematoma from the fracture site because of fasciotomy, secondary neutrophilic microvascular dysfunction and reperfusion injury also contributes to the poor fracture healing, muscular contracture and persistent neuralgic pain[23,31,32]. We noticed 38% delayed or non-unions with a mean union time of 24 wk. A recent systematic review by Reverte et al[23], reported the mean time of tibial fracture union in ACS to be 31.7 wk and the incidence of delayed union and nonunion was 25% (in patients > 18 years). Other available literature reported the incidence of delayed union and nonunion to be 55%[22,23]. Our finding on fracture union is almost comparable to the available literature. Three factors such as fracture site, mode of diagnosis and ICP value were analysed to evaluate their effects on fracture healing. Although it seemed that proximal tibial fracture and clinically diagnosed ACS patients were at risk of delayed union and nonunion, it was statistically insignificant.
We found that the major long term functional disability of compartment syndrome is mainly because of soft tissue contracture. Ankle stiffness (76%) and toe deformities (62%) because of soft tissue contractures were the most common complications. Residual persistent pain was also seen in 55% of pain. The cause of pain in these patients may be multifactorial. Soft tissue contracture causes restriction of knee, ankle and toes movement and elicits pain on stretching or weight bearing. Ischemic damage of nerve fibre inducing neuralgic pain may also be contributory. Although a majority of patients were able to sit (with knee bending 90 degree and cross leg), climb stair and walk, there was difficulty in running and squatting. About 55% of patients were unable to run and 42% patients were unable to squat. A statistically significant correlation between persistent pain and raised ICP was noted, however none of the other sequelae/complications of ACS showed significant association.
The functional disability in ACS of leg has never been evaluated objectively. We found a severe functional disability in majority of patients because of residual disability as evaluated on LEFS. Fifty percent of patients had severe disability and 30% had moderate disability. More than 55% patients had LEFS score of less than 60% maximal functional capacity. We found lower LEFS scores had significant correlation with higher ICP (R = 0.814, P < 0.001). Outcome of ACS is most importantly determined by timing and adequate decompression of all the compartments. Both single and double incision fasciotomy have been proved to be effective. In our study also we did not find any difference in outcome of either surgical technique (P > 0.05). The average delay in fasciotomy in our study was 7.91 h which is higher than critical delay of 6 h and, this delay correlated with poor outcome scores; although not significantly (P > 0.05). We also noted that despite fasciotomy more than 50% patients still had poor outcome. This could be because of several reasons like, 40% of these had delay of more than 6 h, 3 patients ended up with amputation after fasciotomy. We also noted that the average time to diagnosis of ACS from the time of injury was about 9 h which could have contributed to significant tissue damage by the time ACS was diagnosed.
To conclude, ACS in tibial fractures leads to severe functional disability in majority of patients. These patients are prone for delayed union and nonunion; however, long term disability is mainly because of severe soft tissue contracture. ICP correlates with functional disability; patients with relatively high ICP are prone for poor functional outcome.
The intracompartmental pressure affects the union and functional capability of patients in tibial fracture complicated with acute compartment syndrome (ACS).
Tibial fractures with compartment syndrome are prone for delayed union and nonunion. These patients usually suffer from functional disabilities because of soft tissue contracture, neuralgic pain and residual paralysis. There is no literature about correlation of deep posterior compartment pressure of leg and functional outcome in tibial fracture with ACS. An objective assessment of the disabilities in such patients is lacking.
The deep posterior compartment pressure of the leg was measured in patients with clinically diagnosed compartment syndrome after a tibial fracture using modified Whiteside’s technique. The union rate, union time and functional disabilities in these patients were correlated to the pressure value. The average times for clinical and radiological union were 25 wk (10 to 54 wk) and 24 wk (12 to 52 wk) respectively. Thirty-eight percent patients had delayed union or nonunion. Most common complaint at follow up was ankle stiffness (76%) that caused difficulty in walking, running and squatting. On lower extremity functional scale evaluation, there were 48% patients with severe disability, 35% with moderate disability and 17% with minimal disability. The mean pressures in patients with minimal disability, moderate disability and severe disability were 37.8, 48.4 and 58.79 mmHg respectively.
Compartment syndrome in tibial fractures leads to severe functional disability in majority of patients. These patients are prone for delayed union and nonunion; however, long term disability is mainly because of severe soft tissue contracture. The deep posterior compartment pressure correlates with functional disability; patients with relatively high pressure are prone for poor functional outcome.
The authors evaluated patients with tibia fracture and compartment syndrome. The authors found the correlation between compartment pressure and the functional disability. The article is well-written.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sakamoto A, Wu CC S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Gelberman RH, Garfin SR, Hergenroeder PT, Mubarak SJ, Menon J. Compartment syndromes of the forearm: diagnosis and treatment. Clin Orthop Relat Res. 1981;161:252-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 53] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | McQueen MM, Christie J, Court-Brown CM. Acute compartment syndrome in tibial diaphyseal fractures. J Bone Joint Surg Br. 1996;78:95-98. [PubMed] |
| 3. | Tornetta P, Templeman D. Compartment syndrome associated with tibial fracture. Instr Course Lect. 1997;46:303-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Blick SS, Brumback RJ, Poka A, Burgess AR, Ebraheim NA. Compartment syndrome in open tibial fractures. J Bone Joint Surg Am. 1986;68:1348-1353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 133] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | McQueen MM, Gaston P, Court-Brown CM. Acute compartment syndrome. Who is at risk? J Bone Joint Surg Br. 2000;82:200-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Elliott KG, Johnstone AJ. Diagnosing acute compartment syndrome. J Bone Joint Surg Br. 2003;85:625-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 191] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 7. | Park S, Ahn J, Gee AO, Kuntz AF, Esterhai JL. Compartment syndrome in tibial fractures. J Orthop Trauma. 2009;23:514-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 87] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Harris IA, Kadir A, Donald G. Continuous compartment pressure monitoring for tibia fractures: does it influence outcome? J Trauma. 2006;60:1330-1335; discussion 1335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Ulmer T. The clinical diagnosis of compartment syndrome of the lower leg: are clinical findings predictive of the disorder? J Orthop Trauma. 2002;16:572-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 215] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 10. | McQueen MM, Court-Brown CM. Compartment monitoring in tibial fractures. The pressure threshold for decompression. J Bone Joint Surg Br. 1996;78:99-104. [PubMed] |
| 11. | Allen MJ, Stirling AJ, Crawshaw CV, Barnes MR. Intracompartmental pressure monitoring of leg injuries. An aid to management. J Bone Joint Surg Br. 1985;67:53-57. [PubMed] |
| 12. | Shadgan B, Menon M, O’Brien PJ, Reid WD. Diagnostic techniques in acute compartment syndrome of the leg. J Orthop Trauma. 2008;22:581-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 112] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 13. | Whitesides TE, Haney TC, Harada H, Holmes HE, Morimoto K. A simple method for tissue pressure determination. Arch Surg. 1975;110:1311-1313. [PubMed] [DOI] [Full Text] |
| 14. | Mubarak SJ, Hargens AR, Owen CA, Garetto LP, Akeson WH. The wick catheter technique for measurement of intramuscular pressure. A new research and clinical tool. J Bone Joint Surg Am. 1976;58:1016-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 240] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 15. | Rorabeck CH, Castle GS, Hardie R, Logan J. Compartmental pressure measurements: an experimental investigation using the slit catheter. J Trauma. 1981;21:446-449. [PubMed] |
| 16. | Heppenstall RB, Sapega AA, Scott R, Shenton D, Park YS, Maris J, Chance B. The compartment syndrome. An experimental and clinical study of muscular energy metabolism using phosphorus nuclear magnetic resonance spectroscopy. Clin Orthop Relat Res. 1988;226:138-155. [PubMed] |
| 17. | Mubarak SJ, Owen CA, Hargens AR, Garetto LP, Akeson WH. Acute compartment syndromes: diagnosis and treatment with the aid of the wick catheter. J Bone Joint Surg Am. 1978;60:1091-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 404] [Cited by in RCA: 319] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 18. | Matsen FA, Winquist RA, Krugmire RB. Diagnosis and management of compartmental syndromes. J Bone Joint Surg Am. 1980;62:286-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 517] [Cited by in RCA: 406] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 19. | Whitesides TE, Haney TC, Morimoto K, Harada H. Tissue pressure measurements as a determinant for the need of fasciotomy. Clin Orthop Relat Res. 1975;113:43-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 614] [Cited by in RCA: 486] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 20. | Whitesides TE, Heckman MM. Acute Compartment Syndrome: Update on Diagnosis and Treatment. J Am Acad Orthop Surg. 1996;4:209-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 173] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 21. | Sheridan GW, Matsen FA. Fasciotomy in the treatment of the acute compartment syndrome. J Bone Joint Surg Am. 1976;58:112-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 214] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Court-Brown C, McQueen M. Compartment syndrome delays tibial union. Acta Orthop Scand. 1987;58:249-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Reverte MM, Dimitriou R, Kanakaris NK, Giannoudis PV. What is the effect of compartment syndrome and fasciotomies on fracture healing in tibial fractures? Injury. 2011;42:1402-1407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 24. | Matsen FA, Clawson DK. The deep posterior compartmental syndrome of the leg. J Bone Joint Surg Am. 1975;57:34-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 105] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Heckman MM, Whitesides TE, Grewe SR, Rooks MD. Compartment pressure in association with closed tibial fractures. The relationship between tissue pressure, compartment, and the distance from the site of the fracture. J Bone Joint Surg Am. 1994;76:1285-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 137] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 26. | Wilson SC, Vrahas MS, Berson L, Paul EM. A simple method to measure compartment pressures using an intravenous catheter. Orthopedics. 1997;20:403-406. [PubMed] |
| 27. | Collinge C, Kuper M. Comparison of three methods for measuring intracompartmental pressure in injured limbs of trauma patients. J Orthop Trauma. 2010;24:364-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Triffitt PD, König D, Harper WM, Barnes MR, Allen MJ, Gregg PJ. Compartment pressures after closed tibial shaft fracture. Their relation to functional outcome. J Bone Joint Surg Br. 1992;74:195-198. [PubMed] |
| 29. | White TO, Howell GE, Will EM, Court-Brown CM, McQueen MM. Elevated intramuscular compartment pressures do not influence outcome after tibial fracture. J Trauma. 2003;55:1133-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 71] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | Janzing HM, Broos PL. Routine monitoring of compartment pressure in patients with tibial fractures: Beware of overtreatment! Injury. 2001;32:415-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 31. | Bourne RB, Rorabeck CH. Compartment syndromes of the lower leg. Clin Orthop Relat Res. 1989;240:97-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Gulli B, Templeman D. Compartment syndrome of the lower extremity. Orthop Clin North Am. 1994;25:677-684. [PubMed] |