Published online Mar 18, 2017. doi: 10.5312/wjo.v8.i3.242
Peer-review started: September 1, 2016
First decision: September 29, 2016
Revised: November 24, 2016
Accepted: December 16, 2016
Article in press: December 18, 2016
Published online: March 18, 2017
Processing time: 200 Days and 2.9 Hours
Stress fractures in sport are becoming increasing more common, comprising up to 10% of all of sporting injuries. Around 90% of such injuries are located in the lower limb. This articles aims to define the optimal management of lower limb stress fractures in the athlete, with a view to maximise return rates and minimise return times to sport. Treatment planning of this condition is specific to the location of the injury. However, there remains a clear division of stress fractures by “high” and “low” risk. “Low risk” stress fractures are those with a low probability of fracture propagation, delayed union, or non-union, and so can be managed reliably with rest and exercise limitation. These include stress fractures of the Postero-Medial Tibial Diaphysis, Metatarsal Shafts, Distal Fibula, Medial Femoral Neck, Femoral Shaft and Calcaneus. “High risk” stress fractures, in contrast, have increased rates of fracture propagation, displacement, delayed and non-union, and so require immediate cessation of activity, with orthopaedic referral, to assess the need for surgical intervention. These include stress fractures of the Anterior Tibial Diaphysis, Fifth Metatarsal Base, Medial Malleolus, Lateral Femoral Neck, Tarsal Navicular and Great Toe Sesamoids. In order to establish the optimal methods for managing these injuries, we present and review the current evidence which guides the treatment of stress fractures in athletes. From this, we note an increased role for surgical management of certain high risk stress fractures to improve return times and rates to sport. Following this, key recommendations are provided for the management of the common stress fracture types seen in the athlete. Five case reports are also presented to illustrate the application of sport-focussed lower limb stress fracture treatment in the clinical setting.
Core tip: This editorial article offers a current perspective on the treatment of lower limb stress fractures in the athlete. The authors focus on the most common “high risk” (Anterior Tibial Diaphysis, Fifth Metatarsal Base, Medial Malleolus, Lateral Femoral Neck, Tarsal Navicular, Great Toe Sesamoid) and “low risk” stress fractures (Postero-Medial Tibial Diaphysis, Metatarsal Shafts, Distal Fibula, Medial Femoral Neck, Femoral Shaft, Calcaneus), highlighting the optimal treatment methods for each, and assessing the most recent evidence which directs this. The value of preventative interventions is also discussed. Finally, five case reports are presented to demonstrate the evidence-based treatment process in clinical practice.
- Citation: Robertson GAJ, Wood AM. Lower limb stress fractures in sport: Optimising their management and outcome. World J Orthop 2017; 8(3): 242-255
- URL: https://www.wjgnet.com/2218-5836/full/v8/i3/242.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i3.242
Stress fractures represent one of the more serious injuries in sport[1]. Following such injuries, return times to sport are often prolonged, and failure to return to sport, chance of re-injury and persisting morbidity are all distinct possibilities[2-8]. As a group, stress fractures comprise just over 10% of all sport-related injuries, with this figure as high as 30% within certain sports, such as running[1,9-12]. The incidence of these injuries is around 1% within recreational athletes, and around 20% within elite level athletes[1,9-12]. Around 90% of these injuries are located within the lower limb[12,13]. Given the financial implications of sport within modern society, both with the substantial revenues associated with professional sport, as well as the economic implications associated with injuries to amateur athletes, the effect of such injuries is considerable[1].
The significance of this injury depends on the location and nature of the fracture[1]: The tibial diaphysis is the commonest reported location and comprises up to three quarters of all stress fractures[2]; other common sites include the metatarsals, the femoral neck, the tarsal naviculus, the fibula, the medial malleolus and the calcaneus[1,14,15]. Until the 1980’s, much of the stress fracture research had focussed on military cohorts, overlooking cohorts of sporting individuals[9,10]. Since then, there has been increasing attention paid to the epidemiology, management and outcome of these injuries in sporting individuals, along with optimisation of rehabilitation techniques and promotion of injury prevention[1]. However the optimal management plans for many stress fracture locations have still to be determined[1].
At present, there forms a clear division of stress fractures by those which are deemed “high risk”, with a predilection for fracture propagation, delayed union, or non-union[14]; and those which are deemed “low risk”, with reliable healing patterns and resolution of symptoms when managed accordingly[15]. Low risk fractures can often be investigated with radiographs alone, and are virtually always managed successfully through conservative management, with rest, activity modification and rehabilitation[15]. High risk fractures often require specialised imaging to better define and quantify the injury, particularly when first line imaging is equivocal; these injuries also may require surgical management, depending on the location of the injury and the response to initial conservative management[14]. As a consequence of this, return to sport is often more challenging with high risk injuries, and this proves particularly demanding with the high level professional athlete[4,7,14]. For individual fracture types, the severity of the injury can be graded from the extent of the radiological changes, using either generic (Fredericson et al[16] or Arendt et al[17]) or site-specific (Saxena et al[18] or Torg et al[19]) classifications[1,20]; such classifications can further guide management planning as well as provide prognostic information regarding return times to sport[1,20].
The management strategies of these injuries is constantly developing, and at present, the optimal treatment modality for many stress fracture locations remains unestablished[1]. Even with similar injuries, management and return to sport times can vary for different sport, with prolonged rehabilitation often required to return to repetitive loading sports such as long distance running and jumping[1,5]. Regular review of the emerging research in this area, in conjunction with pre-existing treatment protocols, is necessary to determine the best way to manage such athletes, and maximise return to sport[1]. In addition to this, given the overuse nature of such injuries, often demonstrating prodromal symptoms and resulting from the presence of risk factors, primary prevention programmes provide the best way of managing such injuries[21,22]. Ongoing research in this field provides continued resources which can benefit both the athlete and the sports medic to fully maximise the potential of such a practice[21,22].
From the clinical perspective, when defining the optimal method for managing each fracture type, seven major areas require addressing: (1) is the fracture High Risk or Low Risk? (2) what is the optimal imaging modality for the fracture? (3) should this fracture be managed conservatively or surgically? (4) if managed surgically, what is the best technique to employ? (5) if managed conservatively, what is the optimal rehabilitation schedule? (6) how quickly can sporting activities be resumed? and (7) are there any preventative programmes available for this fracture type?
This framework ensures that optimal treatment planning and outcome can be achieved for each individual athlete[1]. In this editorial, we aim to determine the optimal evidence-based management strategies for the most common “high” and “low” risk sport-related lower limb stress fractures, by reviewing the available literature in this field. With this, we also aim to discuss the areas that require further clarification to provide optimal care for the athlete, as well as to assess the emerging evidence for preventative strategy programmes that can avert such injuries from developing. To illustrate this treatment process in clinical practice, five case reports assessing the management of sport-related lower limb stress fractures are presented at the end of the article.
High risk stress fractures are those which have an increased risk of fracture propagation, delayed union, or non-union[14]. This is normally because they are located on the tension side of the bone, or because they develop in an area with limited vascularity. The most common high risk stress fractures are those of the Anterior Tibial Diaphysis, the Fifth Metatarsal Base, the Medial Malleolus, the Lateral Femoral Neck, the Tarsal Navicular and the Sesamoids of the Great Toe[1,14,15,23].
Common in running athletes, anterior tibial diaphyseal stress fractures (TDSFs) are visualised on radiographs as the “dreaded black line” on the anterior mid tibial cortex[1,2,14,24]. However, radiographic changes can be absent in up to 85% of cases[25]; with persisting symptoms and negative radiographs, the recommended second line imaging investigation is now magnetic resonance imaging (MRI) scan[24].
The severity of the fracture can be graded by presence of changes on each of the MRI sequences, using either the Fredericson[16] or the Arendt[17] Scale (Table 1). A higher grade of Fredericson Scale has been shown to be associated with an increased return to running time for TDSFs[16]. When both cortices of the tibia are involved, with completed fracture lines, this injury needs to be managed as an acute fracture[1,2,14].
| Arendt scale[17](MRI based) | Federicson scale[16](MRI based) | Saxena classification[18](CT based) | Torg classification[19](radiograph based) | |
| Location of use | Generic | Generic | Navicular | 5th Metatarsal Base |
| Grade 1 | STIR signal change | periosteal edema - bone marrow normal | Dorsal cortex involved | Acute fracture line, no intramedullary sclerosis or periosteal reaction |
| Grade 2 | STIR and T2 change | periosteal and bone marrow edema - T2 change only | Dorsal cortex and body involved | Widened fracture line with intramedullary sclerosis and periosteal reaction |
| Grade 3 | STIR, T1 and T2 change - no fracture line present | periosteal and bone marrow edema - T1 and T2 change - no fracture line | Dorsal and Volar cortices involved | Widened fracture line with complete intramedullary sclerosis and periosteal reaction |
| Grade 4 | STIR, T1 and T2 change - fracture line present | periosteal and bone marrow edema - STIR, T1 and T2 change - fracture line | - | - |
Current treatment protocols advocate a trial of 3 to 6 mo of conservative management, as initial treatment of these injuries[1,2,14]. Fredericson Grade 1 to 3 injuries are managed with crutch-assisted weightbearing until resolution of pain; bracing serves as a potential adjunct to reduce symptoms[16]. For Grade 4 injuries, initially casting is recommended for a period of 6 wk[16].
If symptoms persist following attempted conservative management, surgical intervention should be advised[1,2,14]. The available surgical techniques include tibial intra-meduallary (IM) Nailing, compression plating, or drilling of the stress fracture with bone grafting[2]. A recent systematic review by Robertson et al[2] found that intra-medullary nailing and compression plating provided the highest return rates and lowest return times of all the surgical treatments available; as such these are the preferred surgical techniques for this injury.
This review also found that conservative management of these injuries resulted in decreased return rates to sport compared to surgical management; return to sports rates were 71% for conservative management and 96% for surgical management[2]. Thus, clinicians must remain aware of the benefit of early surgical management in the high level athlete who fails to respond to conservative management[2]. Reported return times to sports for this injury included 7 mo for conservative management and 7 mo for surgical management[2].
For completed fractures, current protocols advocate conservative management (casting) for those which are undisplaced, and surgical management for those which are displaced, normally with an IM Nail[1,2,14]. Reported return times for these injuries included 11.5 mo for conservative management and 7 mo for surgical management, with return rates of 67% for conservative management and 100% for surgical management[2].
For conservative management, recommended rehabilitation techniques advise activity cessation, with avoidance of heavy loading of the tibia, limited weightbearing with crutches for between 3 to 6 mo[1,2,14]. During this time, bracing of the lower limb can be helpful to reduce symptoms[1,2,14]. Following this, progression of weightbearing and return to loading activities can be allowed as pain permits[1,2,14]. For surgical management, recommended rehabilitation techniques comprise commencement of a progressive weight-bearing programme, within the first week post-operatively, under the care of physiotherapy, with return to full loading activities between 6 and 8 wk post-operatively[1,2,14]. With both conservative and surgical management, full level sport should not be commenced until there is clear evidence of clinical and radiological union[1,2,14].
Validated prevention interventions for this injury type include the use of shock absorbing insoles as well as the optimisation of athlete fitness prior to the commencement of vigorous exercise[21,22,26].
Common in soccer, american football and basketball players, these injuries appear on plain radiographs as a sclerotic or radiolucent line at the proximal aspect of the fifth metatarsal[1,14,23,24]. However, radiographic changes can be absent in up to 69% of patients[25]. In such cases, the second line imaging investigation is now MRI scan[24]. Computed tomography (CT) scan can be of value in assessing fracture union if conservative management is attempted[24]. These injuries are graded using the Torg Classification[19] (Table 1), which provides a helpful guide to direct treatment[13,27].
Torg 1 injuries can be managed either surgically or conservatively[13,27]. Surgical techniques comprise either percutaneous intramedullary cannulated screw fixation or modified tension band wire; screw fixation is the recommended modality as this has the higher volume of evidence at present[4,23]. Conservative management comprises non-weightbearing in a below knee cast or moon boot for 6 wk followed by partial weightbearing for a further 6 wk[27].
There is a growing trend for surgical management of such injuries in high level athletes and athletes in high intensity repetitive loading sports (running, jumping), with a recent systematic review from Mallee et al[4] showing proven benefit of surgical management, in terms of return times and rates to sport. Reported return rates following surgical management ranged from 75% to 100%[27-31], with return times of 13.8 wk[28]. Return rates for conservative management ranged from 33% to 100%[27,28], with return times 19.2 wk[28]. Conservative management however remains a realistic option for the low level athlete.
As conservative management remains a recognised acceptable alternative to surgery, all athletes being advised to undertake surgical treatment should be fully informed of the available treatment options[5,14,23]. The risks and benefits for both surgical and conservative should be fully explained: For conservative management the main benefit being the avoidance of surgery, while the main risk being the development of non-union; for surgical management, the main benefit being an improved return rate and time to sport, while the main risk being that of infection and structural damage[5,14,23].
Torg 2 (delayed union) and Torg 3 (non-union) injuries are advised to be managed with surgical intervention, in the form of internal fixation and bone grafting, to facilitate union[5,14,23]. A higher Torg grading and a plantar gap greater than 1 mm are predictive of a prolonged return times to sport[4,29].
For surgical management, current rehabilitation recommendations advise 3 wk non-weightbearing in a short leg cast, followed by progressive weightbearing over the following 3 to 6 wk in protective footwear[5,14,23]. An over accelerated rehabilitation must be avoided as this significantly increases the chances of treatment failure[5,14,23]. For conservative management, current rehabilitation recommendations advise 6 wk non weightbearing in a cast or boot, followed by 6 wk partial weightbearing in a functional splint, and then by a graduated return to sport under the guidance of the physiotherapists[5,14,23]. With both forms of treatment, full level sport should only be commenced once there is clear evidence of clinical and radiological union[5,14,23]. There are no validated prevention interventions for this fracture type at present[21,22].
Common in athletes involved in running and jumping sports, radiographs form the first line imaging of this condition, but can be negative in up to 55% of cases[25]. With persisting symptoms and no clear radiographic changes, the second line imaging investigation is now MRI scan[24].
Current management protocols direct treatment based on fracture displacement and the level of the athlete[1,5,6,14,23]. All displaced fractures should be treated with surgical reduction and fixation to aid fracture union, reduce post-injury symptoms and facilitate return to sport[1,5,6,14,23]. Undisplaced fractures in the low level athlete are recommended for conservative management, minimal weightbearing with crutches in a short leg cast or moon-boot for 6 to 8 wk[1,5,6,14,23]. Undisplaced fractures in the high level athlete and in athletes who participate in high intensity repetitive loading sports (such as running and jumping) are, however, now recommended for the surgical fixation, as this has been shown to reduce return to sport times, compared to conservative management[1,5,6,14,23]. A recent systematic review by Irion et al[6] found similar return to sport rates for surgical vs conservative management of these injuries (both 100%), but the mean return to sport time was three times higher with conservative management (2.4 wk for surgical management vs 7.6 wk for conservative management).
Surgical techniques include cannulated cancellous screw fixation or modified tension band wire technique[1,5,6,14,23]. The preferred surgical technique is screw fixation, as this has the stronger evidence-base[1,5,6,14,23]. Any athlete undergoing surgical management, when conservative management form a reasonable alternative, should be fully informed of the benefits and risks of both treatments, particularly outlining the surgical risks involved, which include infection, bleeding, structural damage and requirement for revisional surgery[1,5,6,14,23].
Recommended rehabilitation for surgical management comprises 1 to 3 wk limited weightbearing in a cast or moonboot, while that for conservative comprises 6 to 8 wk limited weightbearing in a cast or moonboot[1,5,6,14,23]. This is then followed by a progressive strengthening, range of motion and proprioception programme under the care of the physiotherapist, with a graduated return to sport[1,5,6,14,23]. For both forms of management, return to full level sport should only be performed when there is clear evidence of clinical and radiological union[1,5,6,14,23]. There are no validated prevention interventions for this fracture type at present[21,22].
Most commonly seen in marathon and long distance runners, plain radiographs form the initial imaging investigation for lateral-sided (tension) femoral neck stress fracture (FNSFs)[1,5,8,14,24]; however radiographic changes can be absent in up to 80% of cases[25]. When radiographs are negative, and the history and exam findings are suggestive of the diagnosis, the second line imaging investigation is MRI Scan[24]. The severity of these fractures can be graded using the Arendt[17] or Fredericson[16] Classification; however this type of FNSF is managed universally with surgical fixation, so such gradings have no significant influence on treatment planning[1,5,8,14,24].
Current management protocols advocate urgent surgical fixation of this fracture type, to prevent fracture displacement and its associated risks of avascular necrosis (AVN) of the femoral head[1,5,8,14,24]. Surgical fixation is ideally performed with a Dynamic Hip Screw (DHS) (with or without a de-rotation screw) as compared to multiple cannulated screws (MCS), as the DHS confers more stability of fixation for the unstable shear-pattern of these fractures[1,5,8,14,32-34]. There is limited data for return to sport rates and times for lateral femoral neck fractures, as the majority of studies reported are case reports or series[1,5,8,14]. In a recent systematic review by Neubauer et al[8], which recorded all published FNSFs in runners, 28 out of 48 patients were noted to return running. Displaced fractures had significantly lower return rates (6/18), than non-displaced fractures (22/30)[8]; this has been noted by previous authors[35]. Reported return to sport times varied from 3 to 12 mo[8].
Recommended rehabilitation techniques advise toe-touch weight-bearing with crutches for 6 wk, followed by partial weight-bearing with crutches for a further 6 wk[1,5,8,14,36]. Hydrotherapy and upper limb exercises can be commenced 2 wk post-surgery[36]. Following this, weight-bearing is permitted as tolerated, with commencement of physiotherapy to focus on hip and lower limb muscle strengthening and range of motion exercises, facilitating a graduated return to sport[1,5,8,14,36]. Full level sport should only be commenced once there is clear evidence of clinical and radiological union[1,5,8,14,36]. Clinical and radiographic follow-up should be maintained for a minimum of 2 years to ensure delayed post-treatment AVN does not ensue[1,5,8,14,36].
Validated prevention interventions include education programmes to promote physiological optimisation prior to engaging in rigorous activity, as well performing progressive training regimes (limit training volume increases to 10%,) and limiting training volumes within recommended targets (around 160 km over a 12 wk when starting)[8,37-39].
Common in sprinting athletes, these are visualised on plain radiographs as a sclerotic or radiolucent line extending from the superior tension side of the navicular[1,3,5,14,23]. However, radiographic changes can be absent in up to 40% of cases[25]. Thus, with persisting symptoms and negative radiographs, the second line imaging investigation is either CT or MRI Scan[24]. CT Scanning allows visualisation and quantification of the fracture line, which is useful for management planning[24]. This enables these injuries to be classified by the Saxena Classification[18] (Table 1). This can guide management planning, as well as well provide prognostic information regarding return to sport, with a higher Saxena Grade correlating with a prolonged return to sport[4]. MRI scanning provides a comprehensive picture of the stress injury as well as visualising the surrounding soft tissue structures[24].
Current management protocols are guided by the extent of the fracture line (Saxena Classification) and displacement of the fracture[1,3,5,14,18,23]. At present, for partial undisplaced fractures (Saxena Grade 1 and 2), conservative management with short leg cast and non-weight-bearing for 6 wk is recommended[1,3,5,14,18,23]. In a systematic review by Torg et al[3], such treatment was found to offer superior results over other treatment modalities, with return to sports rates of 96% and return times on mean of 4.9 mo. For displaced or completed fractures (Saxena Grade 3), surgical management, with reduction with internal fixation, is recommended[1,3,5,14,18,23]. Reported return times following surgical management range from 16.4 wk to 5.2 mo, with return to sport rates of 82%[3,4]. The available surgical techniques include screw fixation or fracture site drilling, both with or without bone graft[3,4,18,40]. The preferred technique at present is screw fixation, as this offer improved return times and rates to sport[3,4,40].
To note, developing evidence suggests that surgical management of all navicular stress fractures may offer improved return to sport times for high level athletes[4]; however, such evidence fails to stratify outcome by severity of fracture or Saxena Classification, and, as such, further well designed randomised controls are necessary to confirm this[1,3,5,14,18,23].
Recommended rehabilitation techniques both for conservative and surgical management consist of non-weightbearing in a below knee cast or moon boot for 4 to 6 wk, followed by progressive partial weight bearing for a further 6 wk until painfree[1,3,5,14,18,23]. This is then followed by a graduated return to sporting activities under the supervision of the physiotherapists. For both forms of management, return to full level sport should only be performed when there is clear evidence of clinical and radiological union.
Validated prevention interventions include physiological optimisation programmes for the athlete before embarking upon rigorous physical activity as well as performing progressive training regimes and limiting training volumes within recommended targets[37].
Commonly seen in sports which involve repeated, forced dorsiflexion of the great toe (dancing, gymnastics and sprinting), the medial (tibial) sesamoid is most frequently injured due to its positioning directly beneath the head of the first metatarsal[1,14,23,41,42]. Radiographs are the first line imaging, though changes can be absent in up to 95% of cases[25]. In such cases, with persisting symptoms, MRI is the second line imaging investigation[24]. CT scan can be useful in assessing the progression of union of these fractures[24].
Current management protocols advocate conservative management as the first line treatment for all such injuries. This comprises activity cessation, with a period of 4 to 8 wk limited-weightbearing in below knee cast, or moonboot[1,14,23,41,42]. Following this, weightbearing should be progressed, using a forefoot offloading shoe or modified orthotic, as required for comfort[1,14,23,41,42]. Return rates to sport following successful conservative management include 100%, with return times ranging 3 wk to 1 year[43,44]. There is however a high rate of delayed union, nonunion, and recurrence with this treatment, so if the patient remains symptomatic after 3 to 6 mo of conservative treatment, surgical intervention should be considered[1,14,23,41,42]. Conversion from conservative management to surgical management ranges from 33% to 100% in the published studies[43-45]. There is a variety of surgical techniques available, which include closed reduction and percutaneous fixation, drilling with bone grafting, partial-sesamoidectomy and sesamoidectomy with soft tissue reconstruction[1,14,23,41,42]. Where possible retention of sesamoids should be performed to preserve joint biomechanics and avoid the development of hallux deformities[1,14,23,41,42]. If sesamoidectomy is required, soft tissue reconstruction should be performed in conjunction to try restore such biomechanics[1,14,23,41,42]. The preferred choice of surgical management is guided by the fracture plane (tranverse or longitudinal) and fracture displacement[44]. Transverse undisplaced fractures should be managed by either by screw fixation or drilling and grafting[44]. Transverse displaced fractures should be managed by screw fixation when possible, however partial or complete sesamoidectomy can often be required[44]. Longitudinal fractures are best managed by either drilling and grafting or sesamoidectomy[44]. Reported return rates following surgery range from 90% to 100% with return times ranging 2.5 to 6 mo[43-51].
For conservative management, recommended rehabilitation techniques advise activity cessation and limited weightbearing in a below knee cast or moonboot for 6 wk followed by progressive weightbearing in modified footwear as pain allows[1,14,23,41,46,51]. For operative management, recommended rehabilitation techniques now advocate a more accelerated recovery with crutch-assisted weight-bearing for 1 wk post-operatively, followed by full unassisted weightbearing as pain allows[1,14,23,41,46,49-51]. Under guidance of the physiotherapists, running activities can normally be commenced around 6 wk post-operatively, followed by a return to full level sport as symptoms and physical fitness allow[1,14,23,41,46,49-51]. There are no validated prevention interventions for this fracture type at present[21,22].
Low risk stress fractures are those with a low risk of fracture propagation, delayed union, or non-union, with reliable healing patterns and resolution of symptoms when managed accordingly[15]. This is because they are often located on the compression side of the involved bone, and they develop in an area with robust vascularity. The most common low risk stress fractures are those of the Postero-Medial Tibial Diaphysis, the Metatarsal Shafts, the Distal Fibula, the Medial Femoral Neck, the Femoral Shaft and the Calcaneus[1,9-12,15].
Common in running athletes, these injuries appear as a sclerotic line on the postero-medial border of the proximal to mid tibial diaphysis[1,2,15]. However, radiographic changes can be absent in up to 85% of cases[25]; with persisting symptoms and negative radiographs, the second line imaging of choice is now MRI Scan[24]. If however, the history and examination findings are high suggestive of the diagnosis, the injury can be managed expectantly, with repeated radiographs alone, due to the benign nature of the condition[15].
The severity of the fracture can be graded by presence of changes on each of the MRI sequences, using either the Fredericson[16] or the Arendt[17] Scale (Table 1). The Fredericson Scale was developed from a cohort of postero-medial stress fractures, within which the severity of grading was shown to be associated with return to running times: Grade 1 injuries took 2 to 3 wk to return to running; Grade 2 injuries 4 to 6 wk; Grade 3 injuries 6 to 9 wk; and Grade 4 injuries 12 wk, with initial cast treatment for 6 wk[16]. To note, there is growing evidence that “shin splints” or “tibial periostitis” form a continuum with tibial stress fractures injuries, with MR Studies demonstrating periosteal and bone oedema in cohorts of athletes with “shin splints”[20]. When present, it is advised to treat “tibial periostitis” as Grade 1 injuries, in order to present progression and prolongation of the injury[1,5,15].
Current management protocols advocate conservative management for these stress fractures[1,2,15]. The standard treatment is cessation of activities, with restricted weightbearing, until symptoms resolve[1,2,15]. Adjuncts such as ultrasound and pneumatic bracing can improve return to sport times[1,2,15]. A recent systematic by Robertson et al[2] found that return rates following posterior TDSFs are universally good with all studies reporting return rates of 100%. Return to sport times averaged around 2 mo: Use of pneumatic bracing reduced return times to 1 mo post-injury; use of pulsed ultrasound enabled return to sport immediately post-treatment. Surgical management is reserved for non-unions, with delayed unions treated expectantly; these however are extremely rare due to the well vascularised nature of the postero-medial tibial diaphysis[1,2,15].
Recommended rehabilitation techniques advise cessation of activities which provoke symptoms, with weightbearing as per pain allows[1,2,15]. Some studies advocate immediate return to full weightbearing and sporting activities using an aircast brace, if the patient is completely painfree with the orthotic[2,52]. This is the followed by a graduated return to exercise programmes under the care of the physiotherapists[1,2,15]. Return to full level sport should only be performed with clear evidence of clinical and radiological union[1,2,15].
Validated prevention interventions include the use of shock absorbing insoles, as well as physiological optimisation of the athlete prior to the commencement of vigorous exercise, performing progressive training regimes and limiting training volumes within recommended targets[21,22,26].
Commonly seen in distance runners and ballet dancers, these most often develop in the second metatarsal, followed by the third and fourth metatarsals[1,15,23,53]. The first line imaging of these injuries is plain radiographs; however radiographic changes can be absent in up to 69% of cases[25]. With persisting symptoms, the second line imaging investigation is MRI Scan[24]; however this injury can initially be imaged with serial radiographs, if the history and clinical exam are conclusive with the diagnosis[15]. Current management protocols advocate conservative management for these injuries[5,15,23,53].
This is in the form of activity restriction for 6 to 8 wk, either in a moonboot, short leg cast or fore-foot offloading shoe, with a progressive return to exercise as pain allows[5,15,23,53]. Further adjuncts, such as a firm-based insoles or midfoot taping, can progress mobility and relieve symptoms during the rehabilitaion period[5,15,23,53]. Occasionally, with delayed union or in the presence of severe pain, protracted application of cast may be necessary, for around 12 wk post injury[5,15,23,53]. However, most of these stress fractures heal after 4 wk of compliant conservative management[5,15,23,53]. While, delayed unions can be treated expectantly with prolonged casting, non-unions require surgical intervention in the form of plating and bone graft; this however happens very rarely with compliant treatment[5,15,23,53]. Reported return to sport times range from 4 to 12 wk, with second (10 wk) and third (12 wk) metatarsal fractures taking longer to return than 4th metatarsal fractures (4 wk)[53].
Recommended rehabilitation techniques advise 6 to 8 wk limited weightbearing in a short leg cast, moonboot or forefoot offloading shoe followed by commencement of a graduated activity program once the symptoms have resolved[5,15,23,53]. Following this, a graduated return to sport programme should be undertaken under the care of the physiotherapist[5,15,23,53]. Full level sport should only be commenced once there is clear evidence of clinical and radiological union[5,15,23,53]. Validated prevention interventions include use of viscoelastic insoles, as well as appropriate limitation of training volumes, as athletes who run over 20 m/wk are at increased risk of developing these injuries[14,21-23].
These injuries are most commonly seen in running and jumping athletes; the distal third region is the most common site for stress fracture in the fibula[1,15,23,53]. Standard radiographic changes consist of a sclerotic or radiolucent line at the level of lateral malleolus[15,23]; however radiographs can be negative in up to 40% of cases[25]. In such situations, the second line imaging investigation is currently MRI Scan[24]; however, if the history and clinical exam are conclusive with the diagnosis, the injury can be managed with serial radiographs initially[15].
Current management protocols advocate conservative management for this injury, with cessation of sports, activity modification and immobilisation in a moonboot, air cast or below knee cast for 6 wk, followed by a graduated return to activities as symptoms allow[1,15,23,53]. Immobilisation is preferable with a moonboot or air cast, as this allows ongoing physiotherapy exercises to be performed during treatment[1,15,23,53]. Reported return times to sport are around 13 wk[53]. Some studies advocate immediate return to sporting activities using an aircast brace, if the patient is completely painfree with the orthotic[52]. However, the authors advise caution with this as an over-accelerated return to full level sport, particularly in the high level athlete, can prevent adequate healing and provoke development of a delayed or non-union[1,15,23,53]. Any athlete treated as such should be followed up closely to avoid this occurring[1,15,23,53]. While delayed unions can normally treated with prolonged casting, non-unions will most often require surgical intervention, in the form of plating and bone graft[1,15,23,53].
Recommended rehabilitation techniques advise limited weightbearing with crutches for 6 to 8 wk, in a moonboot, air cast or below knee cast, followed by a graduated return to activities, as symptoms allow, under the care of the physiotherapists. If an accelerated return to sport is attempted using an aircast, clinicians must remain vigilant for development of a delayed or non-union[1,15,23,53]. In order to avoid this, return to full level sport should only be performed when there is clear evidence of clinical and radiological union[1,15,23,53]. There are no validated prevention interventions for this injury type at present[21,22].
Most often recorded in marathon and long distance runners, these injuries are visualised on plain radiographs as an area of sclerosis or radiolucency at the medial aspect (compression side) of the femoral neck, perpendicular to the osseous trabeculae[1,5,8,15,54,55]. However, radiographic changes can be absent in up to 80% of cases[25]; when radiographs are negative, and the history and examination findings are suggestive of this condition, the second line imaging investigation is now MRI Scan[24]. This can allow grading of severity of the stress fracture using the Arendt Scale, which has been found to predict return times to sport post-treatment (Table 1)[17,24,56].
Current management protocols guide management based on the extent and displacement of the fracture, as per the Naval Medical Centre San Diego Classification[1,5,8,15,54,55]. Compression FNSFs which span less than 50% of the femoral neck width can be treated conservatively, with limited weightbearing followed by a graduated return to exercise programme[1,5,8,15,54,55]. However, if the fracture line spans more than 50% of the femoral neck width, or if there is displacement, surgery is indicated to stabilise the fracture[1,5,8,15,54,55]. The compression fracture is oblique in nature, and biomechanically more stable than the tension fracture; so MCS can be used as the preferred fixation method[32-34]. Other surgical techniques include DHS plus or minus de-rotation screw. With the largest series of sport-related compression FNSFs to date (n = 27), Ramey et al[56] reported a return to sport rate of 100% for conservative management, with a mean return to sport time of 14.1 wk. Return times were noted to increase with worsening severity of fracture on the Arendt Scale (Grade 1: 7.4 wk, Grade 2: 13.8 wk, Grade 3: 14.7 wk, Grade 4: 17.5 wk)[56]. Reports of surgically managed compression FNSFs in the athlete are limited, and none provide formative sporting outcome data[57].
For both conservative and surgical management, recommended rehabilitation techniques advise 6 wk toe-touch weightbearing with crutches, followed by 6 wk partial to full weightbearing with crutches[1,5,8,15,54-56]. Hydrotherapy and upper limb exercises can be commenced 2 wk post-immobilisation[36]. After this, weight-bearing is permitted as tolerated, and return to sport is performed in a graduated manner under the care of the physiotherapy team[1,5,8,15,54-56]. Full level sport should only be commenced once there is clear evidence of clinical and radiological union. Clinical and radiographic follow-up should be maintained for a minimum of 2 years to ensure delayed post-treatment AVN does not ensue[1,5,8,15,54-56].
Validated prevention interventions include education programmes to promote physiological optimisation prior to engaging in rigorous activity, as well performing progressive training regimes (limit training volume increases to 10%) and limiting training volumes within recommended targets (around 160 km over a 12 wk when starting)[8,37-39].
Most commonly seen in running athletes and lacrosse players, these fractures mainly develop on the medial compression side of the femoral shaft, within the proximal and middle thirds of the bone[1,5,15,24]. Plain radiographs form the first line of imaging; however, radiographic changes can be absent in up to 80% of cases[25]. With persisting symptoms and negative radiographs, the second line imaging of choice is now MRI Scan[24].
Current management protocols direct management based on the extent, nature and location of the fracture[1,5,15,24]. The majority of femoral shaft stress fractures are incomplete, non-displaced and compression-sided, and these can be successfully treated by a period of activity cessation, restricted weightbearing with crutches, for 4 wk, followed by a graduated return to activity[1,5,15,24]. Return times to sport following such regimes are normally around 12 wk[1,5,15,24,58]. Surgical intervention should be considered for displaced fractures, tension-sided (lateral cortex) fractures, delayed union, and non-unions[1,5,15,24]. Surgical techniques available include femoral IM Nailing and lateral sided compression plating. The preferred surgical technique is currently the femoral IM Nail as this provides the strongest biomechanical construct to stabilise the fracture site and allow healing[1,5,15,24].
For conservative management, recommended rehabilitation programmes advise 4 wk toe-touch weightbearing, with progression to full weightbearing as pain permits[1,5,15,24,58]. With this injury, it is normally possible to return to light athletic training within 6 wk and to commence full level sport-within 3 mo[1,5,15,24,58]. Regular follow-up, with interval radiographs, is required to ensure the fracture progresses to union; return to full level sport should only be performed with clear evidence of clinical and radiological union[1,5,15,24,58]. For surgical management, recommended rehabilitation programmes advise commencement of a progressive weight-bearing programme within 1 wk post-operatively, with return to full-impact loading activities between 6 to 8 wk post-operatively[1,5,15,24]. This is then followed by a progressive return to activity programme, under the guidance of the physiotherapists, with return to sport often achieved between 12 to 16 wk post-operatively[1,5,15,24]. Full level sport should only be commenced once there is clear evidence of clinical and radiological union[1,5,15,24].
Validated prevention interventions include education programmes to promote physiological optimisation prior to engaging in rigorous activity, as well as performing progressive training regimes and appropriate limitation of training volumes[8,37-39].
Reported in long distance runners and basketball players, these fractures most commonly develop on the posterosuperior aspect of the calcaneus, but can also develop on the anterior process or the medial tuberosity of the calcaneus[15,23,41]. Plain radiographs form the initial imaging investigation, and are often positive when the condition is present, with as many as 87% of cases showing positive X-ray findings[25]. This is most often seen as an area of sclerosis, which traverses perpendicular to the trabeculae of the postero-superior calcaneus[15,23,24,41]. When radiographs are negative, and symptoms persist, MRI scan is the preferred second line imaging investigation, allowing exclusion of associated differential diagnoses such as plantar fasciitis, Achilles tendinosis and retrocalcaneal bursitis[24].
Current management protocols advocate conservative management for these injuries, in the form of cessation of activity and immobilisation in a moon boot or below knee cast, non-weightbearing for 4 wk, then partial weight-bearing for a further 4 wk[15,23,41,59]. For conservative management, return rates post injury is 100%, with return times ranging between 11 to 12 wk[23,59]. Surgical management is reserved for fracture which fail to unite despite prolonged compliant conservative management; the current recommended treatment is drilling of the fracture site, with or without bone graft[60]. Occasionally the fracture is associated with a Calcaneo-Navicular Coalition; in such cases, if the fracture fails to heal with conservative management, excision of the coalition with fixation of the fracture should be considered[61,62].
Recommended rehabilitation techniques following conservative management advise 4 wk of non-weight-bearing with crutches in a moonboot, followed by 4 wk partial weightbearing, and then a progressive return to exercise programme under the care of the physiotherapy team[15,23,41,59].
There are no validated primary prevention interventions for the fracture type at present[21,22]. However, padded heel orthotics and stretching exercises of the calf muscles and plantar fascia have been shown to be valuable secondary prevention measures[15,23,41].
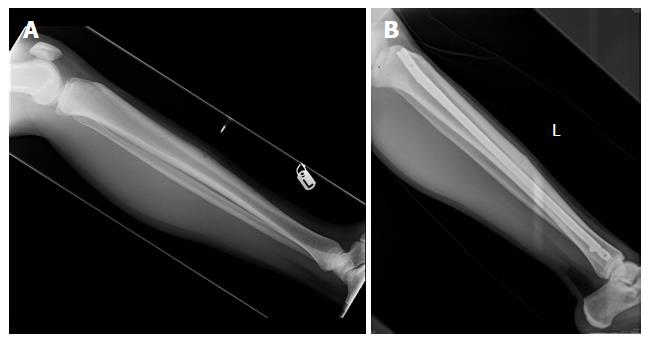
A 25-year-old professional ballet dancer presented to the Sports Medicine Clinic with a 6 mo history of atraumatic left anterior shin pain. She was otherwise in good health. Radiographs revealed an anterior stress fracture of the tibial diaphysis (Figure 1A). The limb was distally neuro-vascularly intact and the overlying skin was healthy. Her blood tests (bone profile and biochemistry) were normal and her body mass index (BMI) was 20 kg/m2. With the distinct radiographic changes, demonstrating a clear fracture line, MRI scan was not felt to be necessary.
Following an informed discussion in clinic, she was advised that the first line treatment for this injury was conservative management, with activity cessation, cast immobilisation for 6 wk and limited weightbearing for at least 3 mo, followed by progression of weightbearing, as pain allowed. She was in agreement with this.
After 3 mo of conservative treatment, she was still very painful at the fracture site, with limited evidence of healing on radiographs. She was advised that, given the limited clinical and radiological progress, surgical intervention was now recommended to aid fracture union. Following an informed discussion regarding the risks and benefits of surgery, she decided to proceed with surgical management, and, later that week, underwent a tibial intra-medullary nail uneventfully (Figure 1B).
Post-operatively, she engaged upon a progressive weight-bearing programme over the following 3 mo, under the care of physiotherapy. She returned to light dancing activities 4 mo post-surgery, and returned to full-level dancing 6 mo post-surgery.
At 2 years follow-up, she reports occasional anterior knee pain, but has no pain at the fracture site and radiographs show complete healing of the stress fracture.
Key message: Primary management of anterior tibial diaphyseal stress fractures comprise conservative management with rest, limited weight-bearing and activity modification, with a graduated return to activities as able. However, if, the patient remains symptomatic after 4 to 6 mo of conservative management, with limited evidence of healing on radiographs, surgical management should be considered, with either an intra-medullary nail or a compression plate.
A 24-year-old middle distance runner presented to the Sports Medicine Clinic with a 4 mo history of atraumatic posterior right lower limb pain. He was otherwise in good health. Radiographs revealed a posterior stress fracture of the tibial diaphysis (Figure 2). The limb was distally neuro-vascularly intact and the overlying skin was healthy. His blood tests (bone profile and biochemistry) were normal and his BMI was 23 kg/m2. An MRI scan showed a Fredericson Grade 3 Postero-Medial Tibial Diaphyseal Stress Fracture.
Following an informed discussion in clinic, he was advised the recommended treatment for this injury was conservative management, with activity restriction and limited weightbearing in a well-padded moonboot, with progression of weightbearing as pain permits. He was in agreement with this.
Following 3 mo of conservative treatment, he was painfree over the fracture site, with clear evidence of healing on radiographs. He had returned to running training at 4 mo post-treatment, and competed successfully in a running race 6 mo post-treatment.
At 2 years follow-up, he reports no symptoms and continues to participate at high level middle distance running.
Key message: Primary management of posterior tibial diaphyseal stress fractures is conservative management with activity modification and limited weightbearing with a graduated return to activities as able. This can be supplemented by pneumatic bracing and ultrasound therapy, both of which has been shown to improve return to sport times.
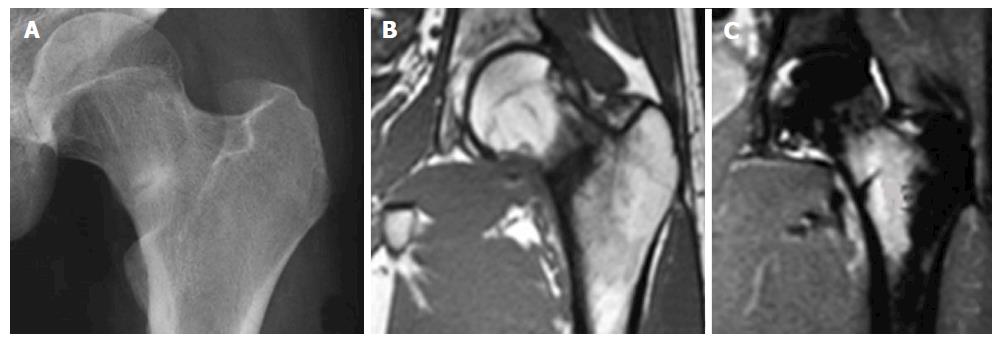
A 24-year-old marathon runner presented to the Emergency Department with severe right groin pain after completing a marathon the previous day. She had been training incrementally for this over the last 3 mo and has noted worsening right groin pain for the last month. This was only present during exercise and her coach diagnosed it as ilio-psoas tendinitis. There was no preceding trauma. She was otherwise in good health. Radiographs revealed a minimally displaced tension-sided fracture of the lateral femoral neck (Figure 3A). The limb was distally neuro-vascularly intact and the overlying skin was healthy. She reported pain with full flexion of the hip and with axial compression of the hip. Otherwise her pain was minimal at rest. Her blood tests (bone profile and biochemistry) were normal and her BMI was 19 kg/m2. With the distinct radiographic changes, demonstrating a clear fracture line, MRI Scan was not felt to be necessary.
She was admitted as an in-patient and kept on strict bed rest. Following discussion with the on-call consultant in the morning ward round, she underwent Dynamic Hip Screw fixation that day (Figure 3B).
Post-operatively she was kept toe-touch weight-bearing with crutches for 6 wk, followed by partial weight-bearing with crutches for a further 6 wk. After this, she was allowed to weight-bear as pain permitted, and progressed in a graduated exercise programme under the care of the physiotherapists. Lower limb athletic activity was commenced 18 wk post-surgery, with clear evidence of fracture union radiologically and no pain clinically. With further input from physiotherapy, she returned to running at 6 mo post-surgery, and competed in a marathon again 10 mo post-surgery.
She had dedicated follow-up over 2 years with sequential radiographs to assess that the fracture united and that the fixation did not lose reduction or displace.
At 2 years follow-up, she reports occasional pain at the fracture site with prolonged exercise, particularly in the cold, though her radiographs show complete healing of the stress fracture.
Key message: Primary management of a minimally displaced lateral femoral neck stress fracture comprises of surgical fixation, with a Dynamic Hip Screw, ideally within 24 h of presentation.
A 20-year-old middle distance runner presented to the Sports Medicine Clinic with a 3 mo history of worsening atraumatic exercise-related left groin pain. He had been training incrementally over the last 4 mo and had noted worsening left groin pain for the last month. This was initially felt to be a groin sprain and treated with analgesia and exercise modification. He was otherwise in good health. Radiographs revealed a compression sided fracture of the medial femoral neck (Figure 4A). The limb was distally neuro-vascularly intact and the overlying skin was healthy. He had mild pain at full flexion of the hip as well on axial compression, but otherwise the hip was painfree. His blood tests (bone profile and biochemistry) were normal and his BMI was 22 kg/m2.
He was placed on crutches, non-weightbearing, and underwent a MRI scan which showed a compression fracture which extended 25% across the width of the femoral neck (Figure 4B and C).
Following discussion in clinic, he was advised that the recommended treatment for this was conservative management, with limited weightbearing on crutches, followed by a progressive weight-bearing regime, as pain allows, under the supervision of the physiotherapists.
He was kept partial weight-bearing, with crutches for 6 wk, and then underwent progressive weightbearing as pain allowed. Lower limb athletic activity was commenced in a graduated manner 10 wk post-diagnosis, with input from physiotherapy, as there was clear evidence of fracture union radiologically, and clinically there was no pain. With further guidance from physiotherapy, he returned to running at 6 mo post-diagnosis, and returned to racing 9 mo post diagnosis.
He had dedicated follow-up over 2 years with sequential radiographs to assess that the fracture united and did not displace.
At 2 years follow-up, he reports no symptoms and his radiographs show complete healing of the stress fracture.
Key message: The first line management of undisplaced medial-sided compression femoral neck stress fractures, which extend less than 50% of the femoral neck width, is conservative management, with limited weight bearing using crutches, followed by a progressive weight-bearing programme and then a return to exercise programme, under the supervision of the physiotherapy team.
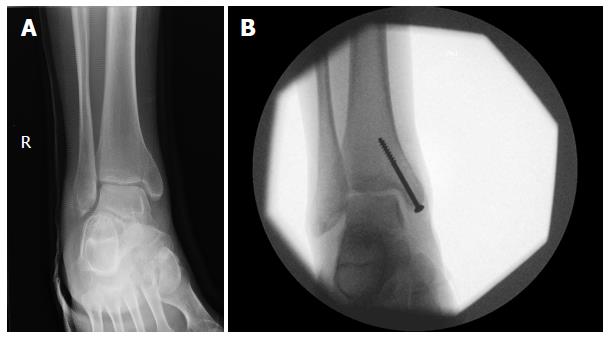
A 21-year-old high performance middle distance runner presented to the Sports Medicine Clinic with a 4 mo history of atraumatic medial ankle pain. He was otherwise in good health. Radiographs revealed an undisplaced completed medial malleolar stress fracture (Figure 5A). The limb was distally neuro-vascularly intact and the overlying skin was healthy. His blood tests (bone profile and biochemistry) were normal and his BMI was 23 kg/m2. With the distinct radiographic changes, demonstrating a clear fracture line, MRI Scan was not felt to be necessary.
During an informed discussion in clinic, he was advised that both surgical and conservative management were options, with surgical management most likely offering a quicker return time to sport but with the risk of developing surgical complications. Due to a desire to return to sport as quickly as possible, he chose to undergo surgical management of his fracture. The following day, he underwent fixation of his fracture with two 4.0-mm AO cannulated cancellous screws (Figure 5B).
Post-operatively, he was non-weight-bearing for 3 wk, and then he progressed to full weight-bearing in an Aircast cast boot. He returned to light running training 2 mo post-surgery, and to full-level sports 3 mo post-surgery.
At 2 years follow-up, he continues to participate at the same level of running he was at pre-injury. He reports occasional pain at the fracture site, particularly on prolonged running in the cold, but otherwise is asymptomatic and radiographs show complete healing of the stress fracture.
Key message: Primary surgical management of undisplaced completed medial malleolar stress fractures can result in improved return to sport times compared to conservative management, though this exposes the patient to the risk of surgical complications.
Within this editorial, we have outlined the currently recommended management strategies for the most common sport-related lower limb stress fractures, determining the treatments which offer the best proven results for the athlete, as well as the proven rehabilitation methods to allow the earliest return to sport possible. This is based on the most recent high quality literature in the field, derived from either systematic reviews or high impact clinical studies on each fracture type. With this, we have also reviewed the current evidence-based preventative interventions for each of the fracture types. Integration of the case studies then provides clinicians with a realistic perspective of how to manage such injuries in clinical practice. From this, we hope to provide clinicians with both a management framework for these injuries, along with, the most up-to-date evidence-based information on their treatment; this should allow provision of a systematic and evidence-based approach to assessing and treating lower limb sport-related stress fractures in their practice.
Areas found to be of particular value in the management of these injuries, were the site specific classifications, which were effective in guiding treatment and prognosis of these injuries[1,16-19,54]. As such, we recommend the development of further evidence-based classifications for lower limb sport-related stress fractures.
Areas requiring further clarification in the management of these injuries include the role for surgical management of certain high risk injuries, the optimal surgical modality in such cases, and the optimal rehabilitation methods for each fractures type, particularly the role for various adjuncts such as air casts[1-6,14,15,44]. Further work is required in these areas to better define the optimal treatment methods of these injuries.
The provision of optimal care when managing sport-related stress fractures is vital to maximise return rates to sport, to minimise return times and to limit persisting symptoms and recurrence of injury[1,14,15,23]. The treatment of these injuries is specific to the location and the nature of the fracture, and a specialist knowledge of the topic is required to provide optimal management[1-4,6,8,14,15,23]. It is vital for clinicians to be appropriately informed of the common mode of presentation of these injuries, their optimal imaging modality and the most effective treatment strategies, in order to maximise the care of the athlete[1,14,15,23,24]. The use of preventative measures against such injuries is an evolving concept, and can be a valuable aid to athletes and sports teams accordingly[21,22]. Management of the high profile athlete remains a pressurised a situation, as time away from sport can have significant financial and social consequences, so specialist input from experienced personnel should be co-ordinated to ensure optimal care[1].
In order to maximise the management and outcome of these injuries, it is essential that clinicians continue to participate and support in research in this area[1,14,15,23]. All treating clinicians should keep documentation of their management and outcome of such injuries, allowing regular publication of relevant case series[1,14,15,23]. Furthermore, well established specialists centres should co-ordinate more extensive cohort studies and epidemiological studies, to further establish the effects of variations in practice on outcomes[1,14,15,23]. Where possible, randomised controlled trials in this field should be funded and supported, as these will provide “gold standard” evidence to determine the optimal treatment modalities of sport-related stress fractures[1,14,15,23].
When managing such injuries, clinicians should remember to provide a holistic approach, performing a detailed assessment of each patient to establish pre-disposing risk factors, such as abnormal gait biomechanics or nutritional deficiencies, which should be addressed appropriately, to avoid recurrence of the condition. Similarly, when managing the female athlete, clinicians should always consider the female athlete triad as an underlying cause of the condition, assessing and managing this accordingly[1,14,15,23]. Lastly, it should be noted that all athletes and clinicians should adhere to the established treatment principles that have been developed for these conditions[1,14,15,23]. Such treatment protocols have been developed from well-organised research within military and sporting populations, both of which provide robust patient cohorts. Thus any attempt to over-accelerate rehabilitation in the athlete, is likely to results in inadequate treatment and recurrence of the condition[1,14,15,23]. With appropriate compliance to the recommended treatment, athletes should be reassured that outcomes from these injuries are largely positive, with high return rates to previous level sport and favourable return times[1,14,15,23]. Given the importance of providing well-informed, individually directed care for such injuries in the high level athlete, it remains important that specialised sport physicians and sports surgeons provide care for these individuals, in order to optimise their management and outcome[1,14,15,23].
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Ito K, Pedret C, Weel H S- Editor: Qiu S L- Editor: A E- Editor: Li D
| 1. | Behrens SB, Deren ME, Matson A, Fadale PD, Monchik KO. Stress fractures of the pelvis and legs in athletes: a review. Sports Health. 2013;5:165-174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 2. | Robertson GA, Wood AM. Return to sports after stress fractures of the tibial diaphysis: a systematic review. Br Med Bull. 2015;114:95-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Torg JS, Moyer J, Gaughan JP, Boden BP. Management of tarsal navicular stress fractures: conservative versus surgical treatment: a meta-analysis. Am J Sports Med. 2010;38:1048-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Mallee WH, Weel H, van Dijk CN, van Tulder MW, Kerkhoffs GM, Lin CW. Surgical versus conservative treatment for high-risk stress fractures of the lower leg (anterior tibial cortex, navicular and fifth metatarsal base): a systematic review. Br J Sports Med. 2015;49:370-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Kaeding CC, Yu JR, Wright R, Amendola A, Spindler KP. Management and return to play of stress fractures. Clin J Sport Med. 2005;15:442-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 71] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Irion V, Miller TL, Kaeding CC. The treatment and outcomes of medial malleolar stress fractures: a systematic review of the literature. Sports Health. 2014;6:527-530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Dobrindt O, Hoffmeyer B, Ruf J, Seidensticker M, Steffen IG, Fischbach F, Zarva A, Wieners G, Ulrich G, Lohmann CH. Estimation of return-to-sports-time for athletes with stress fracture - an approach combining risk level of fracture site with severity based on imaging. BMC Musculoskelet Disord. 2012;13:139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Neubauer T, Brand J, Lidder S, Krawany M. Stress fractures of the femoral neck in runners: a review. Res Sports Med. 2016;24:185-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes. A study of 320 cases. Am J Sports Med. 1987;15:46-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 663] [Cited by in RCA: 542] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 10. | Hulkko A, Orava S. Stress fractures in athletes. Int J Sports Med. 1987;8:221-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 138] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Iwamoto J, Takeda T. Stress fractures in athletes: review of 196 cases. J Orthop Sci. 2003;8:273-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 164] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 12. | Iwamoto J, Sato Y, Takeda T, Matsumoto H. Analysis of stress fractures in athletes based on our clinical experience. World J Orthop. 2011;2:7-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in CrossRef: 35] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 13. | Pegrum J, Dixit V, Padhiar N, Nugent I. The pathophysiology, diagnosis, and management of foot stress fractures. Phys Sportsmed. 2014;42:87-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Boden BP, Osbahr DC. High-risk stress fractures: evaluation and treatment. J Am Acad Orthop Surg. 2000;8:344-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 229] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 15. | Boden BP, Osbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29:100-111. [PubMed] |
| 16. | Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23:472-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 355] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 17. | Arendt EA, Griffiths HJ. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sports Med. 1997;16:291-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 156] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 18. | Saxena A, Fullem B, Hannaford D. Results of treatment of 22 navicular stress fractures and a new proposed radiographic classification system. J Foot Ankle Surg. 2000;39:96-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 94] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Torg JS, Balduini FC, Zelko RR, Pavlov H, Peff TC, Das M. Fractures of the base of the fifth metatarsal distal to the tuberosity. Classification and guidelines for non-surgical and surgical management. J Bone Joint Surg Am. 1984;66:209-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 275] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Spitz DJ, Newberg AH. Imaging of stress fractures in the athlete. Radiol Clin North Am. 2002;40:313-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 97] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Shaffer SW, Uhl TL. Preventing and treating lower extremity stress reactions and fractures in adults. J Athl Train. 2006;41:466-469. [PubMed] |
| 22. | Rome K, Handoll HH, Ashford R. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 2005;CD000450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 48] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Mayer SW, Joyner PW, Almekinders LC, Parekh SG. Stress fractures of the foot and ankle in athletes. Sports Health. 2014;6:481-491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 24. | Fredericson M, Jennings F, Beaulieu C, Matheson GO. Stress fractures in athletes. Top Magn Reson Imaging. 2006;17:309-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 186] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 25. | Greaney RB, Gerber FH, Laughlin RL, Kmet JP, Metz CD, Kilcheski TS, Rao BR, Silverman ED. Distribution and natural history of stress fractures in U.S. Marine recruits. Radiology. 1983;146:339-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 159] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 26. | Schwellnus MP, Jordaan G, Noakes TD. Prevention of common overuse injuries by the use of shock absorbing insoles. A prospective study. Am J Sports Med. 1990;18:636-641. [PubMed] |
| 27. | Chuckpaiwong B, Queen RM, Easley ME, Nunley JA. Distinguishing Jones and proximal diaphyseal fractures of the fifth metatarsal. Clin Orthop Relat Res. 2008;466:1966-1970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 102] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 28. | Ekstrand J, van Dijk CN. Fifth metatarsal fractures among male professional footballers: a potential career-ending disease. Br J Sports Med. 2013;47:754-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 29. | Lee KT, Park YU, Young KW, Kim JS, Kim JB. The plantar gap: another prognostic factor for fifth metatarsal stress fracture. Am J Sports Med. 2011;39:2206-2211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Pecina M, Bojanic I, Smoljanovic T, Ivkovic A, Mirkovic M, Jelic M. Surgical treatment of diaphyseal stress fractures of the fifth metatarsal in competitive athletes: long-term follow-up and computerized pedobarographic analysis. J Am Podiatr Med Assoc. 2011;101:517-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Popovic NJA, Georis P, Gillett P. Proximal Fifth Metatarsal Diaphyseal Stress Fractures in Football Players. Foot and Ankle Surgery. 2005;11:135-141. [DOI] [Full Text] |
| 32. | Lee CH, Huang GS, Chao KH, Jean JL, Wu SS. Surgical treatment of displaced stress fractures of the femoral neck in military recruits: a report of 42 cases. Arch Orthop Trauma Surg. 2003;123:527-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 73] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 33. | Enocson A, Lapidus LJ. The vertical hip fracture - a treatment challenge. A cohort study with an up to 9 year follow-up of 137 consecutive hips treated with sliding hip screw and antirotation screw. BMC Musculoskelet Disord. 2012;13:171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 34. | Fullerton LR, Snowdy HA. Femoral neck stress fractures. Am J Sports Med. 1988;16:365-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 108] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 35. | Johansson C, Ekenman I, Törnkvist H, Eriksson E. Stress fractures of the femoral neck in athletes. The consequence of a delay in diagnosis. Am J Sports Med. 1990;18:524-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 107] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 36. | Scott MP, Finnoff JT, Davis BA. Femoral neck stress fracture presenting as gluteal pain in a marathon runner: case report. Arch Phys Med Rehabil. 1999;80:236-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 37. | Chalupa RL, Aberle C, Johnson AE. Observed Rates of Lower Extremity Stress Fractures After Implementation of the Army Physical Readiness Training Program at JBSA Fort Sam Houston. US Army Med Dep J. 2016;6-9. [PubMed] |
| 38. | Scott SJ, Feltwell DN, Knapik JJ, Barkley CB, Hauret KG, Bullock SH, Evans RK. A multiple intervention strategy for reducing femoral neck stress injuries and other serious overuse injuries in U.S. Army Basic Combat Training. Mil Med. 2012;177:1081-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 39. | Pihlajamäki HK, Ruohola JP, Weckström M, Kiuru MJ, Visuri TI. Long-term outcome of undisplaced fatigue fractures of the femoral neck in young male adults. J Bone Joint Surg Br. 2006;88:1574-1579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 40. | McCormick JJ, Bray CC, Davis WH, Cohen BE, Jones CP, Anderson RB. Clinical and computed tomography evaluation of surgical outcomes in tarsal navicular stress fractures. Am J Sports Med. 2011;39:1741-1748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 41. | Welck MJ, Hayes T, Pastides P, Khan W, Rudge B. Stress fractures of the foot and ankle. Injury. 2015; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 42. | McInnis KC, Ramey LN. High-Risk Stress Fractures: Diagnosis and Management. PM R. 2016;8:S113-S124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 43. | Hulkko A, Orava S, Pellinen P, Puranen J. Stress fractures of the sesamoid bones of the first metatarsophalangeal joint in athletes. Arch Orthop Trauma Surg. 1985;104:113-117. [PubMed] |
| 44. | Ribbans W, Hintermann B. Hallucal Sesamod Fractures Athletes: Diagnosis and Treatment. Sports Orthop and Traumatol. 2016;32:295-303. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 45. | Van Hal ME, Keene JS, Lange TA, Clancy WG. Stress fractures of the great toe sesamoids. Am J Sports Med. 1982;10:122-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 99] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 46. | Biedert R, Hintermann B. Stress fractures of the medial great toe sesamoids in athletes. Foot Ankle Int. 2003;24:137-141. [PubMed] |
| 47. | Anderson RB, McBryde AM. Autogenous bone grafting of hallux sesamoid nonunions. Foot Ankle Int. 1997;18:293-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 48. | Lee S, James WC, Cohen BE, Davis WH, Anderson RB. Evaluation of hallux alignment and functional outcome after isolated tibial sesamoidectomy. Foot Ankle Int. 2005;26:803-809. [PubMed] |
| 49. | Bichara DA, Henn RF, Theodore GH. Sesamoidectomy for hallux sesamoid fractures. Foot Ankle Int. 2012;33:704-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 50. | Saxena A, Krisdakumtorn T. Return to activity after sesamoidectomy in athletically active individuals. Foot Ankle Int. 2003;24:415-419. [PubMed] |
| 51. | Blundell CM, Nicholson P, Blackney MW. Percutaneous screw fixation for fractures of the sesamoid bones of the hallux. J Bone Joint Surg Br. 2002;84:1138-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 52. | Dickson TB, Kichline PD. Functional management of stress fractures in female athletes using a pneumatic leg brace. Am J Sports Med. 1987;15:86-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 53. | Heaslet MW, Kanda-Mehtani SL. Return-to-activity levels in 96 athletes with stress fractures of the foot, ankle, and leg: a retrospective analysis. J Am Podiatr Med Assoc. 2007;97:81-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 54. | Shin AY, Gillingham BL. Fatigue Fractures of the Femoral Neck in Athletes. J Am Acad Orthop Surg. 1997;5:293-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 55. | Egol KA, Koval KJ, Kummer F, Frankel VH. Stress fractures of the femoral neck. Clin Orthop Relat Res. 1998;72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 64] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 56. | Ramey LN, McInnis KC, Palmer WE. Femoral Neck Stress Fracture: Can MRI Grade Help Predict Return-to-Running Time? Am J Sports Med. 2016;44:2122-2129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 57. | O’Brien J, Taunton J, Larsen J, Forster BB. 31-year-old female runner with 5-week history of hip pain. Br J Sports Med. 2011;45:136-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 58. | Kang L, Belcher D, Hulstyn MJ. Stress fractures of the femoral shaft in women’s college lacrosse: a report of seven cases and a review of the literature. Br J Sports Med. 2005;39:902-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 59. | Serrano S, Figueiredo P, Páscoa Pinheiro J. Fatigue Fracture of the Calcaneus: From Early Diagnosis to Treatment: A Case Report of a Triathlon Athlete. Am J Phys Med Rehabil. 2016;95:e79-e83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 60. | Taketomi S, Uchiyama E, Iwaso H. Stress fracture of the anterior process of the calcaneus: a case report. Foot Ankle Spec. 2013;6:389-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Pearce CJ, Zaw H, Calder JD. Stress fracture of the anterior process of the calcaneus associated with a calcaneonavicular coalition: a case report. Foot Ankle Int. 2011;32:85-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 62. | Nilsson LJ, Coetzee JC. Stress fracture in the presence of a calcaneonavicular coalition: a case report. Foot Ankle Int. 2006;27:373-374. [PubMed] |