Published online Mar 18, 2017. doi: 10.5312/wjo.v8.i3.212
Peer-review started: September 5, 2016
First decision: September 29, 2016
Revised: October 16, 2016
Accepted: December 13, 2016
Article in press: December 14, 2016
Published online: March 18, 2017
Processing time: 196 Days and 23.7 Hours
Anterior cruciate ligament (ACL) injury is a traumatic event that can lead to significant functional impairment and inability to participate in high-level sports-related activities. ACL reconstruction is considered the treatment of choice for symptomatic ACL-deficient patients and can assist in full functional recovery. Furthermore, ACL reconstruction restores ligamentous stability to normal, and, therefore, can potentially fully reinstate kinematics of the knee joint. As a consequence, the natural history of ACL injury could be potentially reversed via ACL reconstruction. Evidence from the literature is controversial regarding the effectiveness of ACL reconstruction in preventing the development of knee cartilage degeneration. This editorial aims to present recent high-level evidence in an attempt to answer whether ACL injury inevitably leads to osteoarthritis and whether ACL reconstruction can prevent this development or not.
Core tip: This editorial aims to present recent evidence in an attempt to answer the following questions: (1) does anterior cruciate ligament (ACL) injury inevitably leads to osteoarthritis (OA)? (2) can ACL reconstruction prevent cartilage degeneration and to what extend is this possible? and (3) what are the risk factors for OA development after ACL injury?
- Citation: Paschos NK. Anterior cruciate ligament reconstruction and knee osteoarthritis. World J Orthop 2017; 8(3): 212-217
- URL: https://www.wjgnet.com/2218-5836/full/v8/i3/212.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i3.212
Anterior cruciate ligament (ACL) tear is a devastating injury with both short and long term consequences. Short-term knee functional impairment is successfully addressed with ACL reconstruction and rehabilitation that allows patients to return to previous sports activities. However, the long-term consequences of ACL injury and the role of ACL reconstruction towards fully restoring knee biomechanics and potentially preventing cartilage degeneration post-traumatically is surrounded with controversy. The aim of this editorial is to discuss the recent literature for the long-term effects of ACL reconstruction, in an attempt to seek answers on whether ACL reconstruction can prevent development of osteoarthritis (OA).
ACL deficiency leads to anteroposterior and rotational instability as well as functional impairment, as evidenced by subjective and objective knee functional scores. The role of instability as a predisposing factor for cartilage degeneration was highlighted early[1]. Using regression analysis, a prospective analysis of 292 patients with knee injury, revealed a linear correlation between radiographic scores and maximum displacement measurements[1].
ACL reconstruction is the treatment of choice for symptomatic ACL deficient knees. Undeniably, ACL reconstruction restores knee stability, knee kinematics are also reinstated, and functional scores can be also equivalent to ACL-intact knees[2,3]. As a result, if knee instability and its resultant abnormal forces to cartilage was the sole factor for future OA development, ACL reconstructed knees would theoretically have similar incidence of OA compared to ACL uninjured knees.
ACL tear was reported to be associated with a higher risk for knee OA regardless reconstruction. A meta-analysis of six studies evaluating progression of OA after ACL injury showed that ACL-reconstructed knees had a relative risk of 3.62 vs uninjured knees (206 out of 395 vs 62 out of 395) in OA development, indicating that ACL reconstruction cannot fully prevent OA. Non-operative treated ACL-deficient knees showed a relative risk of 4.98 (40 out of 120 vs 8 out of 120), suggesting that ACL reconstruction can act preventively for OA compared to non-operative treatment[4]. A relative risk of 3.89 for ACL-injured knees existed towards OA (240 out of 465) compared to contralateral knees (73 out of 507)[4]. These data suggest that ACL reconstruction can prevent OA development to a certain degree. The presence of a higher risk for OA compared to the uninjured knee, demonstrates that ACL reconstruction cannot fully eliminate the increased risk of OA progression.
Some studies demonstrated that ACL reconstruction not only cannot fully prevent development of OA, but, in certain occasions, ACL reconstruction may be associated with a higher prevalence of knee OA. Specifically, a retrospective cohort study at 11 years post ACL injury showed that only 25% of conservatively treated knees developed OA vs 42% in ACL reconstructed knees[5]. Similarly, another report demonstrated that patients that underwent ACL reconstruction had a higher incidence of knee OA[1]. Furthermore, a more severe degree of OA using radiographic criteria was shown after ACL reconstruction compared to ACL-injured knees. Specifically, the relative risk of progression to severe OA in ACL-injured knees using Kellgren and Lawrence grade III or IV was found to be 3.84 compared to the controls[4]. In contrast, the relative risk in ACL-reconstructed knees was 4.71[4]. These findings are typically attributed to the higher incidence of meniscus injury in these patients[1,4]. However, most studies that compare the degree of cartilage degeneration between patients undergoing ACL reconstruction and patients with non-operative treatment showed either reduction in the risk of OA development or no difference in risk[4]. The phenomena that can potentially lead to increased OA prevalence after ACL reconstruction are poorly understood. Further research that can identify additional risk factors that play a major role in OA development - apart from knee stability - is of paramount importance.
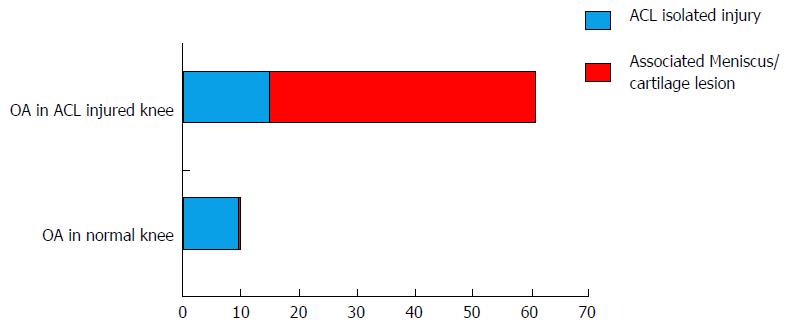
A key factor that contributes to the development of OA is the presence of combined injuries, i.e., the presence of meniscal or chondral injury combined with ACL tear. Specifically, patients suffering from a combined injury had a significantly higher chance to develop radiographic knee OA (Kellgren and Lawrence grade 2 or higher) compared to subjects with isolated ACL injuries[6]. Indeed, 80% of the ACL reconstructed knees with associated meniscal or chondral injuries developed knee OA after 10-15 years vs only 62% of subjects with isolated ACL reconstructed injuries[6]. In the same cohort study, the percentage of subjects that developed knee OA at the contralateral uninjured knee was 15%[6]. The importance of menisci and cartilage status at the time of the ACL reconstruction was confirmed in another study with 7.5 years follow-up that demonstrated that IKDC radiographic score was abnormal in only 3% of patients with intact menisci and cartilage, while an abnormal IKDC score was obtained in 32% of patients that had both menisci damaged as well as cartilage lesions at the time of the initial surgery[7]. Similar results were highlighted by a systematic review that reported a prevalence of knee OA after isolated ACL injury ranging between 0% to 13%. In contrast, when a meniscal injury was present, the prevalence of OA increased between 21% to 48%, highlighting the significant role of meniscal injuries to subsequent osteoarthritis[8]. Unquestionably, the presence of a meniscal or chondral injury at the time of initial ACL tear is considered the most important predictor for the development of subsequent OA. Figure 1 describes the degree of contribution of ACL and associated injuries in the percentage of OA development.
The major role of meniscus and cartilage lesions at the time of surgery in the future development of OA was shown clearly by the findings of a recent study with long term follow-up that excluded patients with concomitant injuries at the initial surgery at its assessment. Specifically, it was shown that, 20 years after ACL reconstruction, in 122 patients, 80% of those treated with patellar tendon graft and 87% of those treated with hamstrings tendon graft, respectively, had normal or nearly normal IKDC scores. Considering that the mean age of patients during the 20-year follow-up assessment was approximately 50 years of age, the prevalence of 20% and 13%, respectively, for OA presence in that age group can be considered comparable to that of normal population[9].
One theory that aims to explain the increased incidence of OA in ACL injured knees without associated injuries is the theory of the initial impact. According to this theory, acute impact trauma to the articular cartilage initiates a degeneration process that can progress to osteoarthritis over the next years after the event. During ACL injury, pro-inflammatory cytokines, such as interleukin-6, interleukin-8, tumor necrosis factor-alpha, and keratan sulfate are increased and can remain elevated even three months after the injury[10-12]. These changes, as well as changes in gene expression post impact injury could trigger cartilage catabolism and potentially initiate the process of cartilage degeneration[11,13]. An indirect sign that supports this theory is the significant cartilage thickening seen in MRIs 5 years following an ACL tear, that can be attributed to abnormal swelling due to disruption of cartilaginous matrix integrity[14]. However, the exact role of cartilage thickness change after ACL injury is yet to be determined.
A recent prospective case-controlled study that measured MRI T2 relaxation times, cartilage oligomeric matrix protein (COMP) - an indicator of cartilage breakdown-, and C-reactive protein levels attempted to shed more light in the phenomena occurring after ACL injury that may be associated with OA development[15]. Specifically, it was shown that the cartilage at the lateral knee compartment of ACL-injured patients with associated bone marrow edema exhibited prolonged T2 relaxation times, suggesting that the bone marrow edema may represent areas of initial cartilage injury that could potentially predispose to cartilage degeneration[15]. This study also demonstrated that cartilage that was not directly impacted may also be the subject of future degeneration due to changes in joint homeostasis, as shown by the elevated levels of serum COMP and the prolonged T2 relaxation times in areas where no bone marrow edema was present. At 1-year post ACL reconstruction, T2 relaxation time remained prolonged in certain areas, indicating that the alterations seen in cartilaginous matrix may persist[15]. A cohort study with yearly follow-up assessment for 11 years showed that cartilage degradation as a result of the initial impact typically accelerates after 5 years from the injury[16]. These recent data suggest that at the time of ACL injury a degradation process of the cartilaginous matrix initiates, either as the result of direct impact or due to alterations in joint homeostasis after the impact injury to the joint.
A second theory for the high incidence of OA after ACL injury involves chronic derangement of local joint-loading patterns that introduce high shear and compressive forces on the menisci and cartilage that lead to irreversible changes to cartilage homeostasis regardless of restoration of ligamentous stability[17]. Specifically, ACL deficiency leads to increase in contact forces at the cartilage and alteration of knee joint kinematics[18,19]. Furthermore, increased anterior tibial translation can increase stress at both menisci and this explains the high incidence of meniscal tears in ACL-deficient knees[5,20,21]. These secondary injuries could be responsible for subsequent cartilage degeneration in the ACL-deficient knee.
The type of graft used in ACL reconstruction was recently considered that could play a role in future OA development. A recent study evaluating PT and HT grafts at 20 years post ACL reconstruction confirmed previous suggestions for OA development. Specifically, it was demonstrated that further surgery subsequently to ACL reconstruction as well as the use of patellar tendon as a graft increased the odds ratio of abnormal radiographic appearance of the knee by 2.6 and 2.4, respectively. PT grafts were associated with radiographic OA in 61% of patients vs only 41% in HT grafts[9]. In contrast, other reports did not confirm this difference[22]. Additional high-level studies are necessary to further evaluate whether the use of patellar tendon predisposes towards OA progression and to further recognize potential pathogenetic mechanisms of this association.
Identification of factors that are associated with the development of knee OA after ACL injury is clinically important (Table 1). Apart from meniscal and chondral injury at the time of ACL reconstruction, advanced age and high BMI have also been suggested as risk factors for OA development after ACL reconstruction. Every 10 years of age was proposed that add 1.7 odds ratio risk towards OA, while other studies report age greater than 25 years at the time of ACL reconstruction as a predisposing factor[5,23]. Every increment of BMI was associated with a 1.2 odds ratio for progression to OA[5]. Other predisposing factors suggested were an interval of more than 6 mo between injury and reconstruction, loss of knee extension, and poor performance at the single-legged hop test 1 year postoperatively[23,24]. A greater degree of laxity, as documented with Lachman test, was also associated with OA development[25], which re-introduces the question how successfully can ACL reconstruction address anteroposterior and rotation instability post ACL tear[26,27]. The recent interest in the anterolateral structures of the knee and their contribution in rotational knee stability led to techniques that combine ACL reconstruction with lateral extra-articular tenodesis[28,29]. It would be interesting to evaluate long-term results of these procedures towards the development of OA.
| Associated injuries at the time of ACL injury |
| Meniscus tear |
| Cartilage lesion |
| Demographic characteristics |
| Advanced age |
| High BMI |
| Reconstruction related factors |
| Patellar tendon graft |
| Loss of knee extension |
| Laxity in Lachman test |
| > 6 mo interval between injury and reconstruction |
| Poor performance at the single-legged hop test 1 yr postoperatively |
Interestingly, ACL-reconstructed patients traditionally performed significantly better compared to non-operated patients in both subjective and objective scores and demonstrated significantly less laxity at KT-1000[4]. This performance resulted in maintaining a higher participation in high risk pivoting activities and sports involvement. As a consequence, it may difficult to compare the development of OA between patients that fully participate in sports and return to their pre-injury level of activity with patients that cannot fully participate in sports. Furthermore, in a study that evaluated performance on return in elite football players after ACL reconstruction, it was found that there was a significant descent in mean performance compared to controls[30]. Therefore, ACL-reconstruction may contribute to restoration of most functional scores, but a minor deficit - that is obvious only in elite athletes - may still persist. This deficit could be associated with OA progression. For these patients, anterolateral ligament augmentation was recently suggested as a significant contributor to full restoration of function in these athletes[31].
Lastly, the importance of rehabilitation programs after ACL reconstruction has been highlighted over the last few years and certain controversies have been resolved. Specifically, evidence suggests that accelerated rehabilitation protocols that introduce sequential phases are associated with better outcomes[32]. Rehabilitation in phase 1 typically aims towards pain and oedema reduction, and regaining of range of motion. Phase 2 usually introduces progressive improvement of quadriceps and hamstring strength. The next phase adds improvement in neuromuscular control to the above[32,33]. When strength and endurance are maximized, specific exercises that aim to fulfill return to sports criteria are introduced. The criteria used for return to sports are still subject of controversy; however, recent data suggest that functional test assessment, such as single-leg hop test, and muscle strength criteria, such as percentage of isokinetic strength should be introduced[32,34,35]. The importance of maintaining an advanced level of physical activity is critical, as it appears to benefit both physical and mental health[36,37]. In the future, this can be extremely important as new biological treatments for early osteoarthritis become available and, therefore, interventions that can confront the initial phenomena post ACL injury and prevent at the progression to osteoarthritis would be available[38].
ACL tear is associated with an increased risk for OA development. This risk increases remarkably when an associated meniscal or chondral lesion is present. ACL reconstruction potentially restores knee stability and appears to reduce the risk of OA, but it cannot fully eliminate the increased risk. The initial impact of injury at the time of ACL tear could explain the association between OA and ACL tear, but additional research is needed to understand the exact pathogenesis of post-ACL injury OA. Identification of risk factors that can further increase the risk of knee OA is important in an attempt to control the natural history of cartilage degeneration after ACL tear.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Fenichel I, Musumeci G, Tawonsawatruk T, Zayni R S- Editor: Qiu S L- Editor: A E- Editor: Li D
| 1. | Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22:632-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 945] [Cited by in RCA: 865] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 2. | Georgoulis AD, Ristanis S, Moraiti CO, Paschos N, Zampeli F, Xergia S, Georgiou S, Patras K, Vasiliadis HS, Mitsionis G. ACL injury and reconstruction: Clinical related in vivo biomechanics. Orthop Traumatol Surg Res. 2010;96:S119-S128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL. Knee stability and graft function following anterior cruciate ligament reconstruction: Comparison between 11 o’clock and 10 o’clock femoral tunnel placement. 2002 Richard O’Connor Award paper. Arthroscopy. 2003;19:297-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 554] [Cited by in RCA: 502] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 4. | Ajuied A, Wong F, Smith C, Norris M, Earnshaw P, Back D, Davies A. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014;42:2242-2252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 297] [Cited by in RCA: 323] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 5. | Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc. 2008;16:442-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 284] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 6. | Oiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, Fosdahl MA, Risberg MA. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38:2201-2210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 312] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 7. | Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Five- to fifteen-year evaluations. Am J Sports Med. 2000;28:446-452. [PubMed] |
| 8. | Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434-1443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 507] [Cited by in RCA: 545] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 9. | Thompson SM, Salmon LJ, Waller A, Linklater J, Roe JP, Pinczewski LA. Twenty-Year Outcome of a Longitudinal Prospective Evaluation of Isolated Endoscopic Anterior Cruciate Ligament Reconstruction With Patellar Tendon or Hamstring Autograft. Am J Sports Med. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 10. | Cameron M, Buchgraber A, Passler H, Vogt M, Thonar E, Fu F, Evans CH. The natural history of the anterior cruciate ligament-deficient knee. Changes in synovial fluid cytokine and keratan sulfate concentrations. Am J Sports Med. 1997;25:751-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 164] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 11. | Bigoni M, Sacerdote P, Turati M, Franchi S, Gandolla M, Gaddi D, Moretti S, Munegato D, Augusti CA, Bresciani E. Acute and late changes in intraarticular cytokine levels following anterior cruciate ligament injury. J Orthop Res. 2013;31:315-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 141] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 12. | Irie K, Uchiyama E, Iwaso H. Intraarticular inflammatory cytokines in acute anterior cruciate ligament injured knee. Knee. 2003;10:93-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 212] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 13. | Natoli RM, Scott CC, Athanasiou KA. Temporal effects of impact on articular cartilage cell death, gene expression, matrix biochemistry, and biomechanics. Ann Biomed Eng. 2008;36:780-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 58] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Eckstein F, Wirth W, Lohmander LS, Hudelmaier MI, Frobell RB. Five-year followup of knee joint cartilage thickness changes after acute rupture of the anterior cruciate ligament. Arthritis Rheumatol. 2015;67:152-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 15. | Palmieri-Smith RM, Wojtys EM, Potter HG. Early Cartilage Changes After Anterior Cruciate Ligament Injury: Evaluation With Imaging and Serum Biomarkers-A Pilot Study. Arthroscopy. 2016;32:1309-1318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 16. | Potter HG, Jain SK, Ma Y, Black BR, Fung S, Lyman S. Cartilage injury after acute, isolated anterior cruciate ligament tear: immediate and longitudinal effect with clinical/MRI follow-up. Am J Sports Med. 2012;40:276-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 199] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 17. | Louboutin H, Debarge R, Richou J, Selmi TA, Donell ST, Neyret P, Dubrana F. Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee. 2009;16:239-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 217] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 18. | Wang L, Lin L, Feng Y, Fernandes TL, Asnis P, Hosseini A, Li G. Anterior cruciate ligament reconstruction and cartilage contact forces--A 3D computational simulation. Clin Biomech (Bristol, Avon). 2015;30:1175-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Yoo JD, Papannagari R, Park SE, DeFrate LE, Gill TJ, Li G. The effect of anterior cruciate ligament reconstruction on knee joint kinematics under simulated muscle loads. Am J Sports Med. 2005;33:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Fithian DC, Paxton EW, Stone ML, Luetzow WF, Csintalan RP, Phelan D, Daniel DM. Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am J Sports Med. 2005;33:335-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 229] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 21. | Arner JW, Irvine JN, Zheng L, Gale T, Thorhauer E, Hankins M, Abebe E, Tashman S, Zhang X, Harner CD. The Effects of Anterior Cruciate Ligament Deficiency on the Meniscus and Articular Cartilage: A Novel Dynamic In Vitro Pilot Study. Orthop J Sports Med. 2016;4:2325967116639895. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38:448-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 159] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 23. | Seon JK, Song EK, Park SJ. Osteoarthritis after anterior cruciate ligament reconstruction using a patellar tendon autograft. Int Orthop. 2006;30:94-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35:564-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 456] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 25. | Salmon LJ, Russell VJ, Refshauge K, Kader D, Connolly C, Linklater J, Pinczewski LA. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med. 2006;34:721-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 163] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 26. | Tashman S, Collon D, Anderson K, Kolowich P, Anderst W. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:975-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 567] [Cited by in RCA: 510] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 27. | Ristanis S, Stergiou N, Patras K, Vasiliadis HS, Giakas G, Georgoulis AD. Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:1323-1329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 167] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 28. | Kittl C, El-Daou H, Athwal KK, Gupte CM, Weiler A, Williams A, Amis AA. The Role of the Anterolateral Structures and the ACL in Controlling Laxity of the Intact and ACL-Deficient Knee. Am J Sports Med. 2016;44:345-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 239] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 29. | Slette EL, Mikula JD, Schon JM, Marchetti DC, Kheir MM, Turnbull TL, LaPrade RF. Biomechanical Results of Lateral Extra-articular Tenodesis Procedures of the Knee: A Systematic Review. Arthroscopy. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 133] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 30. | Carey JL, Huffman GR, Parekh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receivers in the National Football League. Am J Sports Med. 2006;34:1911-1917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 154] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 31. | Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, Claes S. Outcome of a Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Technique With a Minimum 2-Year Follow-up. Am J Sports Med. 2015;43:1598-1605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 346] [Article Influence: 34.6] [Reference Citation Analysis (1)] |
| 32. | van Grinsven S, van Cingel RE, Holla CJ, van Loon CJ. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1128-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 257] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 33. | van Melick N, van Cingel RE, Brooijmans F, Neeter C, van Tienen T, Hullegie W, Nijhuis-van der Sanden MW. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 617] [Cited by in RCA: 531] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 34. | Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1697-1705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 370] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 35. | Shah VM, Andrews JR, Fleisig GS, McMichael CS, Lemak LJ. Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med. 2010;38:2233-2239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 166] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 36. | Musumeci G. Effects of exercise on physical limitations and fatigue in rheumatic diseases. World J Orthop. 2015;6:762-769. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 43] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 37. | Musumeci G, Loreto C, Imbesi R, Trovato FM, Di Giunta A, Lombardo C, Castorina S, Castrogiovanni P. Advantages of exercise in rehabilitation, treatment and prevention of altered morphological features in knee osteoarthritis. A narrative review. Histol Histopathol. 2014;29:707-719. [PubMed] |
| 38. | Paschos NK. Recent advances and future directions in the management of knee osteoarthritis: Can biological joint reconstruction replace joint arthroplasty and when? World J Orthop. 2015;6:655-659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |