Published online Feb 18, 2017. doi: 10.5312/wjo.v8.i2.208
Peer-review started: August 10, 2016
First decision: September 12, 2016
Revised: September 22, 2016
Accepted: November 21, 2016
Article in press: November 22, 2016
Published online: February 18, 2017
Processing time: 190 Days and 22.1 Hours
Fractures of the scapula are rare and have been reported to account for only 1% of all fractures and 3%-5% of upper extremity fractures. Several studies have reported successful outcomes with non-operative treatment of scapula fractures. Although non-operative treatments are successful in a very high percentage of patients, very few cases of non-union of scapular body fractures have been reported. In our review of the literature, we found two case reports of scapular body fractures developed into non-unions. In both of these cases, open reduction and internal fixation with reconstruction plates and bone graft was successful at eliminating pain and restoring function. This is a case report of a patient with a symptomatic, extra-articular scapular body defect from a non-union that was treated successfully with an acellular dermal extracellular matrix and bone graft using a novel technique
Core tip: Scapular fracture complicated by non-union requiring surgical intervention is extremely rare and seldom reported in the literature. This study demonstrates successful surgical treatement of a symptomatic scapular body defect using a novel technique that has never been described for this condition.
- Citation: Grau L, Chen K, Alhandi AA, Goldberg B. Novel technique for a symptomatic subscapularis herniation through a scapular defect. World J Orthop 2017; 8(2): 208-211
- URL: https://www.wjgnet.com/2218-5836/full/v8/i2/208.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i2.208
Several studies have reported successful outcomes with non-operative treatment of scapula fractures[1-3]. In reviewing the literature, we found only two case reports of scapular body fractures that developed into non-unions[4,5]. In both of these cases, open reduction and internal fixation with reconstruction plates and bone graft was successful at eliminating pain and restoring function. This is a case report of a patient with symptomatic, extra-articular scapular body defect from a non-union, which was treated successfully with acellular dermal extracellular matrix and bone graft using a novel technique.
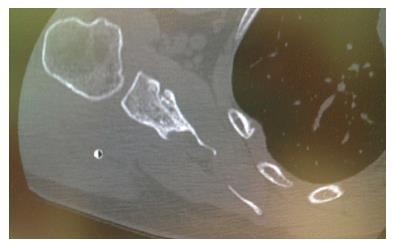
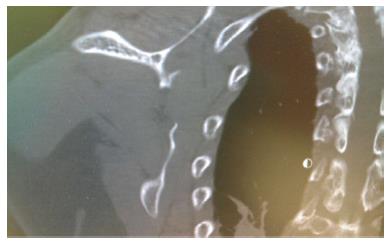
A 52-year-old female sustained a right scapular body and right clavicle fracture in a motorcycle accident 14 mo prior to presenting to our clinic. She was treated non-operatively for the scapular body fracture and with open reduction and internal fixation of the clavicle fracture at an outside hospital. The patient complained that she continued to have constant, posterior shoulder pain along her right scapula after the accident. She came to our clinic because her pain was preventing her from sleeping at night and affecting her activities of daily living. A computed tomography (CT) scan showed a 4 cm × 2 cm elliptical defect of the inferior scapular body with herniation of the subscapularis muscle through the defect (Figures 1 and 2).
On physical exam the patient had tenderness to palpation over the inferior aspect of the scapular body on her right side. Her range of motion was intact with forward flexion of 180 degrees, abduction of 180 degrees, internal rotation of 90 degrees and external rotation of 55 degrees. She was neurologically intact in the axillary, median and ulnar nerve distributions. Her strength was 5/5 in all planes of motion in her upper extremity.
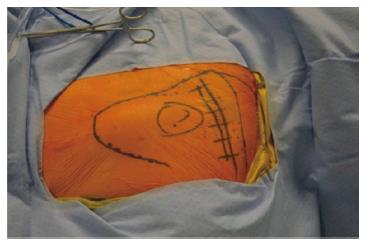
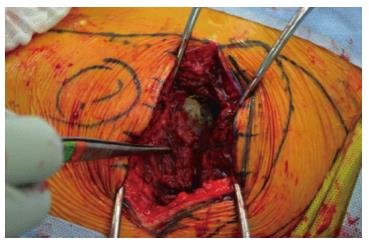
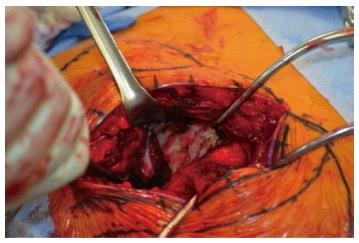
After the nonunion site was marked (Figure 3), an oblique 10 cm incision was made just inferior to the scapular spine running from medial to lateral (Figure 4). A portion of the deltoid was incised in a longitudinal manner to help expose the scapular spine. The infraspinatus muscle was peeled off to expose the nonunion site that was approximately 4 cm in length and 2 cm in width (Figure 5). A herniation of the subscapularis muscle through the defect was noted.
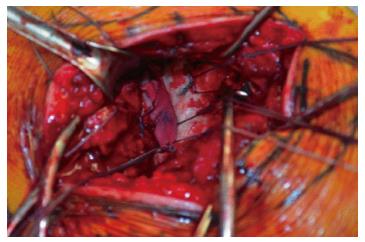
Several drill holes around the edge of the defect were made circumferentially with K-wires and two #2 FiberWires were passed through each of these holes. An Arthroflex jacket (Arthrex, Naples, Florida), which is an acellular dermal extracellular matrix, was sewn into the undersurface of the scapula using #2 FiberWires. Approximately 7 cc of Graft-on bone product was placed on top of the jacket into the defect. The jacket was then folded onto the Grafton and sewn onto the posterior aspect of the scapular creating a pouch and barrier between the anterior and posterior aspects of the scapula (Figure 6). The infraspinatus was then attached back to its origin using O Vicryl and repair the deltoid muscle was performed with O Vicryl sutures in a figure of eight fashion. The dermis and epidermis was closed in standard fashion and dressings were applied. There were no complications postoperatively.
At 2 wk follow up, the patient could sleep through the night, which she could not do prior to the operation. At her two month follow up visit the patient no longer complained of any right shoulder pain. She was also able to get back to doing activities such working out and riding her motorcycle. Her range of motion, strength, and sensation of the right shoulder were fully intact.
In our review of the literature, we found two case reports on scapular nonunion, Gupta et al[5] and Ferraz et al[4] both had excellent results with open reduction and internal fixation using reconstruction plates and bone graft. In both cases the patients had a fracture pattern that was unstable and causing functional limitations. Ferraz et al[4] reported that their patient had pain and decreased range of motion of the shoulder joint secondary to intra-articular involvement of the fracture and cartilage damage. In the case reported by Gupta et al[5] the patient had a transverse comminuted fracture with displacement and overlap of the fracture fragments that was causing winging with forward flexion and decreased range of motion.
Non-union is rare in patients treated conservatively for scapular body fractures and it is perhaps even rarer for these to be symptomatic. Persistent pain following injury requires further work up and possible surgical intervention.
Herniation of the subscapularis muscle through the scapular defect was likely the cause of our patient’s pain. This could be seen on the pre-operative CT scan (Figures 1 and 2). The patient had excellent preoperative function because the defect was not unstable and the scapula remained functioning as a unit and there was no involvement of the joint. For these reasons the authors believed that mechanical stabilization with plates and screws was not necessary. Similar to mesh that is used for intestinal herniation in general surgery the use of the extracellular dermal matrix with bone graft was successful at preventing herniation of the subscapularis, which was likely the patient’s source of pain. This was confirmed by the success of our surgery in providing relief for the patient as early as 2 wk after the procedure and at later follow-up. We believe this to be rare case of scapular nonunion with a unique etiology for pain that was treated with a novel technique.
A 52-year-old women, 14 mo status post non-operative treatment of scapular fracture, presented with constant pain that interrupted her sleep and daily activities.
Intact range of motion and neurovascular exam, with tenderness to palpation over the inferior aspect of the scapular body on her right side.
Subscapularis herniation, painful scapula non-union, rotator cuff pathology, and scapula dyskinesia.
Within normal limits.
Computed tomography scan showed a 4 cm × 2 cm elliptical defect of the inferior scapular body with herniation of the subscapularis muscle through the defect.
Pathological samples were not taken.
Surgical intervention by acellular dermal extracellular matrix and bone graft.
Other reports in the literature have mentioned decreased range of motion associated with the injury. The lack of decreased range of motion does not exclude the injury.
Scapular fracture healed in non-union are not a common result of non-operative treatment.
The use of the extracellular dermal matrix with bone graft was successful at preventing herniation of the subscapularis and alleviating the patient’s symptoms.
It is a well-written case.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Shrestha BM, Sun ZR, Yu BQ S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Dimitroulias A, Molinero KG, Krenk DE, Muffly MT, Altman DT, Altman GT. Outcomes of nonoperatively treated displaced scapular body fractures. Clin Orthop Relat Res. 2011;469:1459-1465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Jones CB, Sietsema DL. Analysis of operative versus nonoperative treatment of displaced scapular fractures. Clin Orthop Relat Res. 2011;469:3379-3389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | McGahan JP, Rab GT, Dublin A. Fractures of the scapula. J Trauma. 1980;20:880-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 131] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Ferraz IC, Papadimitriou NG, Sotereanos DG. Scapular body nonunion: a case report. J Shoulder Elbow Surg. 2002;11:98-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Gupta R, Sher J, Williams GR, Iannotti JP. Non-union of the scapular body. A case report. J Bone Joint Surg Am. 1998;80:428-430. [PubMed] |