Published online Dec 18, 2017. doi: 10.5312/wjo.v8.i12.902
Peer-review started: July 14, 2017
First decision: September 4, 2017
Revised: October 30, 2017
Accepted: November 28, 2017
Article in press: November 28, 2017
Published online: December 18, 2017
Processing time: 160 Days and 3 Hours
To determine morbidity and mortality in hip fracture patients and also to assess for any independent associations between Do-Not-Resuscitate (DNR) status and increased post-operative morbidity and mortality in patients undergoing surgical repair of hip fractures.
We conducted a propensity score matched retrospective analysis using de-identified data from the American College of Surgeons’ National Surgical Quality Improvement Project (ACS NSQIP) for all patients undergoing hip fracture surgery over a 7 year period in hospitals across the United States enrolled in the ACS NSQIP with and without DNR status. We measured patient demographics including DNR status, co-morbidities, frailty and functional baseline, surgical and anaesthetic procedure data, post-operative morbidity/complications, length of stay, discharge destination and mortality.
Of 9218 patients meeting the inclusion criteria, 13.6% had a DNR status, 86.4% did not. Mortality was higher in the DNR compared to the non-DNR group, at 15.3% vs 8.1% and propensity score matched multivariable analysis demonstrated that DNR status was independently associated with mortality (OR = 2.04, 95%CI: 1.46-2.86, P < 0.001). Additionally, analysis of the propensity score matched cohort demonstrated that DNR status was associated with a significant, but very small increased likelihood of post-operative complications (0.53 vs 0.43 complications per episode; OR = 1.21; 95%CI: 1.04-1.41, P = 0.004). Cardiopulmonary resuscitation and unplanned reintubation were significantly less likely in patients with DNR status.
While DNR status patients had higher rates of post-operative complications and mortality, DNR status itself was not otherwise associated with increased morbidity. DNR status appears to increase 30-d mortality via ceilings of care in keeping with a DNR status, including withholding reintubation and cardiopulmonary resuscitation.
Core tip: We present a large, multi-institution retrospective cohort study which examines the independent association of Do-Not-Resuscitate (DNR) status with perioperative outcomes during hip fracture surgery. We find that DNR status independently predicts overall rates of complications and mortality at 30 d without other clear sources of morbidity. Our conclusions place this work in the context of other literature on the outcomes for patients with DNR status during the perioperative period, exploring the data among other surgical populations and hypotheses for this effect.
- Citation: Brovman EY, Pisansky AJ, Beverly A, Bader AM, Urman RD. Do-Not-Resuscitate status as an independent risk factor for patients undergoing surgery for hip fracture. World J Orthop 2017; 8(12): 902-912
- URL: https://www.wjgnet.com/2218-5836/full/v8/i12/902.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i12.902
Do-Not-Resuscitate (DNR) status documents that a decision has been made to withhold certain resuscitative measures in the event of cardiorespiratory arrest. This typically includes withholding chest compressions and endotracheal intubation. DNR status documents a patient’s advance refusal of resuscitative procedures, due to expressed wishes or beliefs, or where cardiopulmonary resuscitation would fail to restore a quality of life compatible with the patient’s goals of care[1-3]. DNR status is most common when patients have multiple, severe co-morbidities, extreme frailty, or end-stage diseases[4-6].
DNR status does not prevent surgery, despite the potential need for endotracheal intubation or inotropic support during anesthesia. The American Society of Anaesthesiologists’ Ethics Committee guidance of 2013 states: “an essential element of preoperative preparation and perioperative care for patients with DNR orders …is communication among involved parties. …The status of these directives should be clarified or modified based on the preferences of the patient”[7]. Patients with DNR status can undergo a range of emergency, urgent or elective surgical procedures to prolong life or improve quality of life. However, as DNR status frequently coincides with narrowed goals of care, procedures tend to be life sustaining or palliative, rather than elective.
The true incidence and composition of surgery in patients with DNR status is unknown. One recent analysis identified 22% of all surgeries in patients with DNR status were lower limb orthopedic procedures[8]. Hip fracture fixation is the most common indication for hip surgery at the older extreme of age, and orthogeriatric patient outcomes have been the focus of recent national quality improvement initiatives[9-12]. However, outcomes after hip fracture surgery specifically in the DNR status population are unknown.
It is also unclear whether DNR status itself independently and negatively impacts major outcomes such as morbidity and length of stay[13-16]. DNR status only directs actions in the event of cardiopulmonary arrest. The “failure to treat” hypothesis, describing inadequate (non-resuscitative) treatment of patients because of DNR status, has been suggested but with inconclusive evidence[17]. The aim of this study is to describe the incidence and distribution of DNR status in patients undergoing hip fracture surgery and to determine whether DNR status is an independent risk factor for worse outcomes on 30 d follow up.
The American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) is a data registry of cases reported from approximately 400 participating sites. ACS-NSQIP is a well-validated database and incorporates data from patients’ medical charts, with data entry overseen by a designated Surgical Clinical Reviewer (SCR) at each site. Institutional Review Board (Brigham and Women’s Hospital, Boston, MA, United States) approval was obtained for analysis of the data and was exempted from the consent requirement due to the de-identified nature of the data.
The 2007-2013 NSQIP was compiled into a single data file containing 306 variables across 2.8 million surgical cases. All cases recording patients under age 18, trauma cases, transplant surgeries, cases where the patient is American Society of Anesthesiologists (ASA) physical status class 6, representing a brain-dead organ donor are excluded from NSQIP (Table 1). We isolated all admissions for hip fracture surgery using all listed ICD codes (Appendix 1) and Current Procedural Terminology (CPT) codes (included in Table 2 with case mix data). All cases failing to report the “do not resuscitate” variable or CPT code were excluded from the analysis. Patient demographic data were collected for age, ASA physical status (PS) class, sex, race, ethnicity, height, weight, and body mass index. Preoperative comorbidity data were collected for functional status prior to surgery, defined as ability to perform activities of daily living (ADL), baseline dyspnea, diabetes mellitus (insulin and non-insulin dependent); smoking status within one year prior to admission; presence of chronic obstructive pulmonary disease, congestive heart failure, coronary artery disease (defined as a composite of a history of angina, myocardial infarction, percutaneous coronary interventions or previous cardiac surgery), hypertension, chronic kidney disease, cerebrovascular accidents, pre-operative weight loss of greater than 10% in the 6 mo prior to surgery, sepsis physiology and a previous operation within the past 30 d. Additional pre-operative laboratories, including the creatinine, albumin, hematocrit, platelet count and international normalized ratio (INR) were collected.
| Category | DNR | Not DNR | OR (95%CI) | P values | ||||
| Num | Denom | % | Num | Denom | % | |||
| Age, mean (SD) | 85.1 | 6.7 | 77.55 | 12.3 | 1.098 (1.088-1.109) | < 0.001 | ||
| < 65 | 26 | 1256 | 2.1 | 1188 | 7962 | 14.9 | Reference | < 0.001 |
| 65-80 | 169 | 1256 | 13.5 | 2384 | 7962 | 29.9 | 3.239 (2.131-4.923) | |
| > 80 | 1061 | 1256 | 84.5 | 4390 | 7962 | 55.1 | 11.043 (7.445-16.381) | |
| Sex | ||||||||
| Male | 313 | 1254 | 25.0 | 2395 | 7950 | 30.1 | Reference | < 0.001 |
| Female | 941 | 1254 | 75.0 | 5555 | 7950 | 69.9 | 1.296 (1.131-1.486) | |
| Demographics | ||||||||
| White | 781 | 1215 | 64.3 | 6008 | 7544 | 79.6 | Reference | < 0.001 |
| Black | 11 | 1215 | 0.9 | 371 | 7544 | 4.9 | 0.228 (0.125-0.417) | |
| Asian | 3 | 1215 | 0.2 | 94 | 7544 | 1.2 | 0.246 (0.078-0.777) | |
| Other | 4 | 1215 | 0.3 | 31 | 7544 | 0.4 | 0.993 (0.349-2.819) | |
| Not reported | 416 | 1215 | 34.2 | 1040 | 7544 | 13.8 | 3.077 (2.686-3.525) | |
| Hispanic | 18 | 824 | 2.2 | 314 | 6677 | 4.7 | 0.453 (0.28-0.732) | 0.001 |
| BMI | ||||||||
| Mean (SD) | 24.1 | 5.5 | 25.3 | 6.5 | 0.966 (0.953-0.978) | < 0.001 | ||
| < 18.5 | 110 | 913 | 12.0 | 630 | 7076 | 8.9 | 1.261 (1.007-1.579) | < 0.001 |
| 18.5-25 | 454 | 913 | 49.7 | 3279 | 7076 | 46.3 | Reference | |
| 25-30 | 244 | 913 | 26.7 | 1976 | 7076 | 27.9 | 0.892 (0.756-1.052) | |
| > 30 | 105 | 913 | 11.5 | 1191 | 7076 | 16.8 | 0.637 (0.51-0.795) | |
| Functional status | ||||||||
| No dyspnea | 1098 | 1256 | 87.4 | 7136 | 7961 | 89.6 | Reference | 0.015 |
| Dyspnea with moderate exertion | 116 | 1256 | 9.2 | 652 | 7961 | 8.2 | 1.156 (0.94-1.423) | |
| Dyspnea at rest | 42 | 1256 | 3.3 | 173 | 7961 | 2.2 | 1.578 (1.12-2.224) | |
| Independent | 491 | 1251 | 39.2 | 4726 | 7917 | 59.7 | Reference | < 0.001 |
| Partially dependent | 579 | 1251 | 46.3 | 2583 | 7917 | 32.6 | 2.158 (1.896-2.456) | |
| Totally dependent | 181 | 1251 | 14.5 | 608 | 7917 | 7.7 | 2.865 (2.369-3.466) | |
| ASA class | ||||||||
| 1 or 2 | 108 | 1256 | 8.6 | 1739 | 7951 | 21.9 | 0.388 (0.315-0.478) | < 0.001 |
| 3 | 779 | 1256 | 62.0 | 4866 | 7951 | 61.2 | Reference | |
| 4 or 5 | 369 | 1256 | 29.4 | 1346 | 7951 | 16.9 | 1.712 (1.492-1.965) | |
| Comorbidities | ||||||||
| Hypertension | 908 | 1256 | 72.3 | 5413 | 7962 | 68.0 | 1.229 (1.076-1.402) | 0.002 |
| Diabetes | 184 | 1256 | 14.7 | 1468 | 7962 | 18.4 | 0.759 (0.643-0.897) | 0.001 |
| COPD | 181 | 1256 | 14.4 | 899 | 7962 | 11.3 | 1.323 (1.114-1.571) | 0.001 |
| CHF | 55 | 1256 | 4.4 | 234 | 7962 | 2.9 | 1.512 (1.12-2.041) | 0.006 |
| CAD | 212 | 1256 | 16.9 | 1340 | 7962 | 16.8 | 1.004 (0.856-1.176) | 0.966 |
| PVD | 25 | 1256 | 2.0 | 235 | 7962 | 3.0 | 0.668 (0.44-1.013) | 0.056 |
| CKD | 29 | 1256 | 2.3 | 214 | 7962 | 2.7 | 0.856 (0.578-1.267) | 0.436 |
| Stroke | 229 | 1256 | 18.2 | 1023 | 7962 | 12.8 | 1.512 (1.292-1.771) | < 0.001 |
| Weight loss | 31 | 1256 | 2.5 | 119 | 7962 | 1.5 | 1.668 (1.118-2.488) | 0.011 |
| Sepsis | 204 | 1249 | 16.3 | 931 | 7892 | 11.8 | 1.46 (1.238-1.721) | < 0.001 |
| Recent surgery | 12 | 1256 | 1.0 | 114 | 7962 | 1.4 | 0.664 (0.365-1.207) | 0.177 |
| Labs | ||||||||
| Creatinine | 1.09 | 0.8 | 1.08 | 0.9 | 1.015 (0.946-1.088) | 0.664 | ||
| Hematocrit | 30.7 | 30.1 | 1.01 (0.986-1.034) | 0.394 | ||||
| Platelets | 212 | 208 | 1.04 (0.977-1.107) | 0.196 | ||||
| Surgical urgency | ||||||||
| Emergent | 428 | 1256 | 34.1 | 2194 | 7962 | 27.6 | 1.359 (1.197-1.542) | < 0.001 |
| Surgical complexity | ||||||||
| Work RVU | 17.45 | 2.0 | 17.46 | 2.7 | 0.998 (0.975-1.021) | 0.841 | ||
| Anesthesia | ||||||||
| General | 796 | 1255 | 63.4 | 6028 | 7959 | 75.7 | NA | < 0.001 |
| Neuraxial/regional | 446 | 1255 | 35.5 | 1876 | 7959 | 23.6 | 1.8 (1.586-2.044) | |
| Other | 13 | 1255 | 1.0 | 55 | 7959 | 0.7 | 1.79 (0.974-3.291) | |
| Anesthesia time | 117.9 | 48.1 | 128.8 | 58.5 | 0.996 (0.995-0.997) | < 0.001 | ||
| Operation time | 61.4 | 43.8 | 70.2 | 43.5 | 0.994 (0.992-0.996) | < 0.001 | ||
| Modified Charlson score | 2.44 | 1.4 | 2.03 | 1.5 | 1.207 (1.16-1.255) | < 0.001 | ||
We calculated a frailty score for each patient undergoing hip fracture surgery to assess for presence of any baseline differences in pre-morbid status between the DNR and non-DNR status groups. We used a variation of the well-known Charlson Comorbidity Index[18-21]. The Canadian Study of Health and Ageing (CSHA)[22] Clinical Frailty Scale is a 7 point index, modified from the Charlson Comorbidity Index. It has been validated previously using NSQIP data, and has been modified for use with data collected within the NSQIP dataset[23].
Data collection for the surgical procedure included the primary surgical CPT code, surgical wound classification, total anesthesia and surgical time and anesthesia type. To assess for independent association between preoperative patient demographic, co-morbidity and frailty variables and DNR status, we conducted univariable and multivariable regression analysis. For the logistic regression, odds ratios (OR) were reported with their associated 95% CI. OR not including 1.00 in their 95%CI were considered statistically significant and were included in the multivariable regression analysis.
We collected binary outcomes data for the following postoperative events up to 30 d after surgery: Death, return to the operating room, superficial and deep space surgical site infections, post-operative pneumonia, unplanned intubation, failure to wean from the ventilator, progressive renal insufficiency and acute renal failure requiring dialysis, urinary tract infections, cerebrovascular accidents, myocardial infarction, post-operative bleeding requiring transfusion of packed red blood cells, deep venous thrombosis requiring therapy, pulmonary embolism and post-operative sepsis. Additional data on discharge destination (Home, Skilled Care, or Rehabilitation facility) and total length of stay were also collected. All outcomes were reported as percentages, with the numerator defined as the absolute count reporting a given outcome and the denominator defined as the total number of cases reporting any outcome for that variable. To assess for the associations between DNR status and post-operative outcomes, we developed a propensity score matched cohort in which patients were matched by propensity for DNR status. We performed univariable and multivariable regression analysis on the matched cohort and OR not including 1.00 in their 95%CI were considered statistically significant.
R Project for Statistical Computing (R version 3.2.3) was used to perform all statistical analysis. Differences between cohorts were assessed using the Pearson chi squared test for categorical variables and using the Student’s t-test for continuous variables due to assessment of normality. However, for the variable length of stay, assessment of the distribution of data was non-normal; thus a Wilcoxon rank sum test was performed on this variable. For all demographic, comorbidity, and operative characteristics, a univariable logistic regression model was fitted to assess the association of each variable with DNR status. Of note, the database does not report any postoperative outcomes (including death) occurring more than 30 d after surgery. Additionally, for variables with a large continuous range, the following assumptions were made; platelet count assumes a change of 100000, while the morbidity and mortality risk scores assume a change of 10%. For anesthesia and surgical operating time, the regression model assumes a time interval change of 10 min.
For our primary analysis, we applied a propensity score matched logistic regression model accounting for propensity for DNR status. The matched cohort was developed using a propensity scoring method in which we incorporated statistically significant variables from the unmatched model into a propensity score model. A 1:1 greedy, nearest neighbor matching strategy was employed utilizing the MatchIt library, producing successful matching of 725 patients who were DNR to 725 patients who were not DNR. Success of the matching process was evaluated using Student’s t-test for continuous variables and Pearson’s χ2 test for categorical variables. We found only one statistically significant difference between the cohorts after matching, which suggested that the matched groups may have hematocrit values that differed by approximately 1.3% (OR = 0.87; P = 0.017; see Table 3).
| CPT code | Translation | DNR | Not DNR | P value | ||||
| num | denom | % | num | denom | % | |||
| 27236 | Open treatment of femoral fracture, proximal end, neck, internal fixation or prosthetic replacement | 210 | 725 | 28.966 | 223 | 725 | 30.759 | 0.994 |
| 27245 | Treatment of intertrochanteric, per-trochanteric, or sub-trochanteric femoral fracture; with intramedullary implant | 173 | 725 | 23.862 | 171 | 725 | 23.586 | |
| 27125 | Hemiarthroplasty, hip, partial (e.g., femoral stem prosthesis, bipolar arthroplasty) | 111 | 725 | 15.31 | 104 | 725 | 14.345 | |
| 27244 | Treatment of intertrochanteric, per-trochanteric, or sub-trochanteric femoral fracture; with plate/screw type implant, with or without cerclage | 91 | 725 | 12.552 | 99 | 725 | 13.655 | |
| 27235 | Percutaneous skeletal fixation of femoral fracture, proximal end, neck | 48 | 725 | 6.621 | 44 | 725 | 6.069 | |
| 27130 | Arthroplasty, acetabular and proximal femoral prosthetic replacement (total hip arthroplasty) | 20 | 725 | 2.759 | 19 | 725 | 2.621 | |
| 27248 | Open treatment of greater trochanteric fracture, with or without internal or external fixation | 9 | 725 | 1.241 | 5 | 725 | 0.69 | |
| 27506 | Open treatment of femoral shaft fracture, with or without external fixation, with insertion of intramedullary implant, with or without cerclage and/or locking screws | 8 | 725 | 1.103 | 12 | 725 | 1.655 | |
| 27187 | Prophylactic treatment (nailing, pinning, plating or wiring) with or without methylmethacrylate, femoral neck and proximal femur | 6 | 725 | 0.828 | 4 | 725 | 0.552 | |
| 27454 | Osteotomy, multiple, with realignment on intramedullary rod, femoral shaft (e.g., Sofield type procedure) | 5 | 725 | 0.69 | 4 | 725 | 0.552 | |
| 27507 | Open treatment of femoral shaft fracture with plate/screws, with or without cerclage | 5 | 725 | 0.69 | 8 | 725 | 1.103 | |
| 27511 | Open treatment of femoral supracondylar or trans-condylar fracture without intercondylar extension, with or without internal or external fixation | 5 | 725 | 0.69 | 6 | 725 | 0.828 | |
| 27228 | Open treatment of acetabular fracture(s) involving anterior and posterior (two) columns, includes T-fracture and both column fracture with complete articular detachment, or single column or transverse fracture with associated acetabular wall fracture, with internal fixation | 3 | 725 | 0.414 | 4 | 725 | 0.552 | |
| 27513 | Open treatment of femoral supracondylar or trans-condylar fracture with intercondylar extension, with or without internal or external fixation | 3 | 725 | 0.414 | 1 | 725 | 0.138 | |
| 27122 | Acetabuloplasty; resection, femoral head (e.g., Girdlestone procedure) | 2 | 725 | 0.276 | 2 | 725 | 0.276 | |
| 27138 | Revision of total hip arthroplasty | 2 | 725 | 0.276 | 2 | 725 | 0.276 | |
| 27165 | Osteotomy, intertrochanteric or sub-trochanteric, including internal or external fixation and/or cast | 2 | 725 | 0.276 | 0 | 725 | 0 | |
| 27509 | Percutaneous skeletal fixation of femoral fracture, distal end, medial or lateral condyle, or supracondylar or trans-condylar, with or without intercondylar extension, or distal femoral epiphyseal | 2 | 725 | 0.276 | 1 | 725 | 0.138 | |
| 27132 | Conversion of previous hip surgery to total hip arthroplasty | 1 | 725 | 0.138 | 1 | 725 | 0.138 | |
| 27134 | Revision of total hip arthroplasty | 1 | 725 | 0.138 | 0 | 725 | 0 | |
| 27254 | Open treatment of hip dislocation, traumatic, with acetabular wall and femoral head fracture, with or without internal or external fixation | 1 | 725 | 0.138 | 1 | 725 | 0.138 | |
| 27450 | Osteotomy, femur, shaft or supracondylar; with fixation | 1 | 725 | 0.138 | 3 | 725 | 0.414 | |
| 27514 | Open treatment of femoral fracture, distal end, medial or lateral condyle, with or without internal or external fixation | 1 | 725 | 0.138 | 1 | 725 | 0.138 | |
For the logistic regression on the matched cohorts, odds ratios (ORs) were reported with associated 95%CI. ORs not including 1.00 in the 95%CI were considered statistically significant. To assess the association specifically between length of stay and DNR status, a Cox proportional hazard model was fitted, incorporating the demographic and comorbidity co-variables as described above to generate a hazard ratio (HR). The model was right censored with death as a completing event.
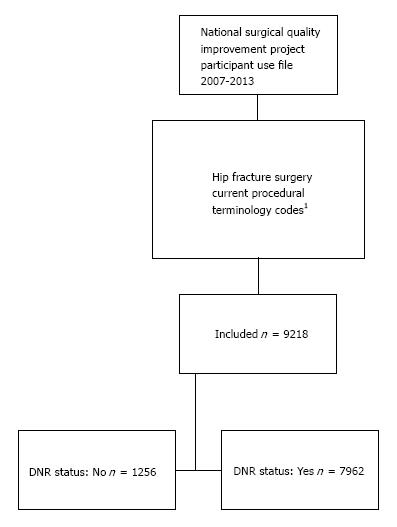
The ICD codes included in the analysis are shown in Appendix 1. A total of 9218 cases met inclusion criteria (Figure 1). Of these, 1256 (13.6%) were patients with DNR status, and 7962 (86.4%) were patients without DNR status. Unmatched univariable analysis demonstrated that patients undergoing hip fracture surgery with DNR status were more likely to be female, aged over > 80 years, unreported race/ethnicity, BMI < 18.5, dyspneic with moderate exertion or rest, ASA class III or IV, partially or totally dependent for activities of daily living or diagnosed with hypertension, diabetes, COPD, CHF, PVD, prior stroke, weight loss, or sepsis (Table 1). Comparison between the groups in the unmatched cohort also suggested that patients with DNR status were more likely to have surgery booked as emergent, to receive a neuraxial or regional anesthetic, have a shorter anesthetic and operative time, and a higher modified Charlson score. These factors were used to construct the propensity score matched cohort as described above.
Using the ACS-NSQIP calculator, the average pre-operative risk prediction within the DNR status group was a mortality of 10% [Standard deviation (S.D) 10%] and morbidity of 15% (S.D 7%). In the non-DNR status group, using the ACS-NSQIP risk prediction calculator the average predicted mortality was 4% (S.D 6%) and morbidity was 11% (S.D 6%).
Table 2 shows the most common 23 CPT codes encountered for hip fracture surgery in the matched cohorts. Ninety-seven point six percent of all DNR patients and 95% of all non-DNR patients had hip fracture surgery classed by one of these CPT codes. The remaining minority (2.4% of DNR and 5% of non-DNR) had other hip fracture surgery CPT codes not listed. These patients were included in the analysis. Table 3 demonstrates the propensity score matched case mix of procedures and the distribution within DNR and non-DNR status groups. The numbers of patients per CPT code were too small to conduct regression analysis. However, ranking CPT codes by frequency demonstrated very similar surgical case mixes in terms of CPT codes between the DNR and non-DNR groups, with the same 10 CPT codes accounting for over 95% of cases and occurring in the same order of frequency, with several low volume exceptions. This suggests there were minimal differences and a high correlation between the surgical case mixes encountered across the two groups, however the degree or significance of differences beyond this were not analysed further. CPT codes were not included in multivariable regression modelling.
| Do-Not-Resuscitate | Not Do-Not-Resuscitate | OR (95%CI) | P-values | |||||
| Category | Num | Denom | % | Num | Denom | % | ||
| Age, mean (SD) | 85.1 | NA | 6.7 | 85.0 | NA | 6.5 | 1.001 (0.985-1.016) | 0.946 |
| < 65 | 17 | 725 | 2.3 | 18 | 725 | 2.5 | Reference | 0.982 |
| 65-80 | 92 | 725 | 12.7 | 93 | 725 | 12.8 | 1.047 (0.508-2.158) | |
| > 80 | 616 | 725 | 85.0 | 614 | 725 | 84.7 | 1.062 (0.542-2.081) | |
| Sex | ||||||||
| Male | 177 | 725 | 24.4 | 165 | 725 | 22.8 | Reference | 0.458 |
| Female | 548 | 725 | 75.6 | 560 | 725 | 77.2 | 0.912 (0.716-1.163) | |
| Demographics | ||||||||
| White | 692 | 725 | 95.4 | 689 | 725 | 95.0 | Reference | 0.462 |
| Black | 6 | 725 | 0.8 | 4 | 725 | 0.6 | 1.493 (0.42-5.316) | |
| Asian | 3 | 725 | 0.4 | 9 | 725 | 1.2 | 0.332 (0.089-1.231) | |
| Other | 3 | 725 | 0.4 | 2 | 725 | 0.3 | 1.493 (0.249-8.966) | |
| Not Reported | 21 | 725 | 2.9 | 21 | 725 | 2.9 | 0.996 (0.539-1.84) | |
| Hispanic | 17 | 725 | 2.3 | 17 | 725 | 2.3 | 1 (0.506-1.974) | 1 |
| BMI | ||||||||
| Mean (SD) | 24.1 | NA | 5.6 | 24.3 | NA | 5.4 | 0.996 (0.977-1.015) | 0.646 |
| < 18.5 | 90 | 725 | 12.4 | 88 | 725 | 12.1 | 0.999 (0.719-1.389) | 0.901 |
| 18.5-25 | 350 | 725 | 48.3 | 342 | 725 | 47.2 | Reference | |
| 25-30 | 198 | 725 | 27.3 | 211 | 725 | 29.1 | 0.917 (0.718-1.171) | |
| > 30 | 87 | 725 | 12.0 | 84 | 725 | 11.6 | 1.012 (0.724-1.415) | |
| Functional status | ||||||||
| No Dyspnea | 614 | 725 | 84.7 | 608 | 725 | 83.9 | Reference | 0.899 |
| Dyspnea with moderate exertion | 77 | 725 | 10.6 | 80 | 725 | 11.0 | 0.953 (0.684-1.329) | |
| Dyspnea at rest | 34 | 725 | 4.7 | 37 | 725 | 5.1 | 0.91 (0.564-1.469) | |
| Independent | 267 | 725 | 36.8 | 269 | 725 | 37.1 | Reference | 0.938 |
| Partially Dependent | 342 | 725 | 47.2 | 336 | 725 | 46.3 | 1.025 (0.818-1.286) | |
| Totally Dependent | 116 | 725 | 16.0 | 120 | 725 | 16.6 | 0.974 (0.717-1.323) | |
| ASA class | ||||||||
| 1 or 2 | 47 | 725 | 6.5 | 49 | 725 | 6.8 | 0.955 (0.627-1.455) | 0.977 |
| 3 | 444 | 725 | 61.2 | 442 | 725 | 61.0 | Reference | |
| 4 or 5 | 234 | 725 | 32.3 | 234 | 725 | 32.3 | 0.995 (0.796-1.245) | |
| Comorbidities | ||||||||
| Hypertension | 547 | 725 | 75.4 | 555 | 725 | 76.6 | 0.941 (0.74-1.198) | 0.623 |
| Diabetes | 120 | 725 | 16.6 | 113 | 725 | 15.6 | 1.074 (0.812-1.422) | 0.617 |
| COPD | 112 | 725 | 15.4 | 117 | 725 | 16.1 | 0.949 (0.716-1.259) | 0.719 |
| CHF | 36 | 725 | 5.0 | 40 | 725 | 5.5 | 0.895 (0.563-1.421) | 0.637 |
| CAD | 147 | 725 | 20.3 | 159 | 725 | 21.9 | 0.905 (0.703-1.165) | 0.44 |
| PVD | 17 | 725 | 2.3 | 23 | 725 | 3.2 | 0.733 (0.388-1.384) | 0.336 |
| CKD | 16 | 725 | 2.2 | 12 | 725 | 1.7 | 1.341 (0.63-2.855) | 0.445 |
| Stroke | 137 | 725 | 18.9 | 139 | 725 | 19.2 | 0.982 (0.756-1.277) | 0.894 |
| Weight loss | 21 | 725 | 2.9 | 20 | 725 | 2.8 | 1.051 (0.565-1.957) | 0.874 |
| Sepsis | 148 | 725 | 20.4 | 152 | 725 | 21.0 | 0.967 (0.75-1.247) | 0.795 |
| Recent surgery | 5 | 725 | 0.7 | 6 | 725 | 0.8 | 0.832 (0.253-2.739) | 0.762 |
| Labs | ||||||||
| Creatinine | 1.13 | 0.8 | 1.11 | 0.7 | 1.034 (0.897-1.192) | 0.646 | ||
| Hematocrit | 33.3 | 34.6 | 0.868 (0.765-0.985) | 0.017 | ||||
| Platelet count | 210 | 206 | 1.067 (0.94-1.211) | 0.313 | ||||
| Surgical urgency | ||||||||
| Emergent | 181 | 725 | 25.0 | 175 | 725 | 24.1 | 1.046 (0.823-1.328) | 0.714 |
| Surgical complexity | ||||||||
| Work RVU | 17.4 | 2.2 | 17.5 | 2.1 | 0.988 (0.942-1.036) | 0.622 | ||
| Anesthesia | ||||||||
| General | 562 | 725 | 77.5 | 557 | 725 | 76.8 | Reference | 0.568 |
| Neuraxial/Regional | 162 | 725 | 22.3 | 168 | 725 | 23.2 | 0.956 (0.748-1.222) | |
| Other | 1 | 725 | 0.1 | 0 | 725 | 0.0 | 1 (-∞-∞) | |
| Anesthesia Time | 122.0 | NA | 49.4 | 123.6 | NA | 49.7 | 0.999 (0.997-1.001) | 0.55 |
| Operation Time | 63.9 | NA | 34.0 | 64.7 | NA | 36.1 | 0.999 (0.996-1.002) | 0.645 |
| Modified Charlson Score | 2.6 | NA | 1.4 | 2.59 | NA | 1.4 | 1.007 (0.936-1.084) | 0.852 |
Table 3 demonstrates various surgical and anaesthetic factors between the matched groups. Post propensity matching univariable regression demonstrated no increased likelihood for patients with DNR status to have a hip fracture surgery as an emergency procedure. DNR status was not independently associated with shorter surgical time (OR = 0.99, CI 0.99-1.00) or anesthetic time (OR = 0.99, 95%CI: 0.99-1.00). DNR status also did not appear to impact anesthesia modality: Compared to general anaesthesia, spinal anesthesia was not more likely in the DNR patient group compared to the non-DNR patient group in the propensity score matched analysis (OR = 0.96, 95%CI: 0.75-1.22).
Table 4 presents outcomes up to 30 d postoperatively between the propensity matched cohorts. Mortality was higher in DNR status patients than in non-DNR status patients undergoing hip fracture surgery, at 15.3% vs 8.1% of patients. Multivariable regression demonstrated DNR status was independently associated with mortality (OR = 2.04, 95%CI: 1.46-2.85, P < 0.001). DNR status was not associated with return to the operating room on multivariable regression.
| Outcomes | DNR | Not DNR | OR (95%CI) | P values | ||||
| Num | Denom | % | Num | Denom | % | |||
| Death | 111 | 725 | 15.3 | 59 | 725 | 8.1 | 2.04 (1.459-2.851) | < 0.001 |
| Reoperation/return to OR | 22 | 725 | 3.0 | 17 | 725 | 2.3 | 1.309 (0.689-2.487) | 0.417 |
| Failure to wean from ventilator | 4 | 725 | 0.6 | 7 | 725 | 1.0 | 0.558 (0.161-1.934) | 0.364 |
| Reintubation | 5 | 725 | 0.7 | 19 | 725 | 2.6 | 0.253 (0.093-0.688) | 0.004 |
| Superficial SSI | 10 | 725 | 1.4 | 0 | 725 | 0.0 | 21.294 (1.245-364.078) | 0.002 |
| Deep incisional SSI | 3 | 725 | 0.4 | 2 | 725 | 0.3 | 1.466 (0.242-8.901) | 0.654 |
| Organ/space SSI | 2 | 725 | 0.3 | 2 | 725 | 0.3 | 1.011 (0.142-7.196) | 1 |
| Wound Dehiscence | 1 | 725 | 0.1 | 0 | 725 | 0.0 | 3.00 (0.122-73.870) | 0.317 |
| Pneumonia | 25 | 725 | 3.4 | 34 | 725 | 4.7 | 0.725 (0.428-1.23) | 0.232 |
| Acute kidney injury | 3 | 725 | 0.4 | 4 | 725 | 0.6 | 0.754 (0.168-3.383) | 0.705 |
| Renal failure requiring dialysis | 3 | 725 | 0.4 | 2 | 725 | 0.3 | 1.5 (0.249-9.034) | 0.654 |
| CVA | 4 | 725 | 0.6 | 5 | 725 | 0.7 | 0.798 (0.213-2.994) | 0.738 |
| Cardiac arrest with CPR | 2 | 725 | 0.3 | 16 | 725 | 2.2 | 0.115 (0.025-0.523) | 0.001 |
| Acute MI | 16 | 725 | 2.2 | 13 | 725 | 1.8 | 1.245 (0.594-2.608) | 0.574 |
| Transfusion | 169 | 725 | 23.3 | 139 | 725 | 19.2 | 1.243 (0.964-1.603) | 0.054 |
| Venous thromboembolism | 9 | 725 | 1.2 | 14 | 725 | 1.9 | 0.621 (0.265-1.457) | 0.293 |
| UTI | 45 | 725 | 6.2 | 41 | 725 | 5.7 | 1.061 (0.683-1.649) | 0.657 |
| Sepsis | 14 | 725 | 1.9 | 23 | 725 | 3.2 | 0.595 (0.303-1.17) | 0.134 |
| Number of complications | Mean | SD | Mean | SD | OR (95%CI) | P-values | ||
| 0.53 | 0.65 | 0.43 | 0.61 | 1.213 (1.043-1.409) | 0.004 | |||
| Length of hospital stay | Mean | SD | Mean | SD | HR (95%CI) | P-values | ||
| 6.4 | 5.0 | 6.74 | 5.3 | 2.133 (0.469-0.871) | 0.219 | |||
Our analysis of the propensity score matched cohort found one difference with respect to post operative morbidity. Patients with DNR status had a slightly higher average number of complications per hospitalization (0.53 vs 0.43; OR = 1.213, 95%CI: 1.04-1.41). Although DNR patients appeared more likely to experience superficial surgical site infections (OR = 21.3; 95%CI: 1.25-364), this was likely an artifact of no events for the non-DNR patients and was no difference was seen with deep surgical site infections or dehiscence rates. DNR patients were less likely to experience reintubation (OR = 0.253; 95%CI: 0.09-0.69), or cardiac arrest with CPR (OR = 0.115; 95%CI: 0.03-0.52). Mean length of stay in the DNR group was no different between the propensity score matched groups.
Our study aimed to examine post-operative mortality and morbidity in patients with DNR status undergoing hip fracture surgery. We also aimed to determine whether DNR status was independently associated with increased morbidity or whether DNR status purely decreased utilisation of CPR and reintubation, without affecting other postoperative outcomes. We found that mortality was over two times greater in the DNR status group, with DNR status independently predicting mortality after patient groups were matched for other underlying comorbidities using propensity scoring methods. However, relatively few sources of morbidity were independently associated with DNR status. Although overall complication rates were slightly higher, rates of reintubation and cardiac arrest with CPR were much lower among patients with a DNR order in place. This raises the question of how we reconcile the increased rate of mortality observed among the DNR cohort in the setting of an isolated, modest overall rate of complications but no clear source of morbidity.
Historically, some surgeons and anesthesiologists have considered perioperative DNR status controversial, given the interventional procedures and unique physiologic changes that occur during anesthesia and the way clinicians manage these events. In light of this, both the American College of Surgeons[24] and American Society of Anesthesiologists[7] have produced consensus statements to guide perioperative management of DNR status. These emphasize communication and individualized management plans, including suspending, then reinstating DNR status post-operatively, if in accordance with a patient’s wishes.
The impact of DNR status on surgical outcomes has been examined previously in the wider surgical cohort and in specific specialty groups such as patients undergoing vascular surgery[25,26]. Kazaure et al[25] demonstrated similar patient associations with having DNR status (white, female, > 85) and also demonstrated high mortality (nearly 1 in 4) in surgical patients with DNR status. However, in contrast to our findings, they demonstrated significantly higher morbidity rates in DNR vs non DNR patients. These higher rates of morbidity were not replicated in our hip fracture specific study, and therefore may imply that in our orthopedic cohort a DNR status did not negatively impact outcomes or morbidity to the degree described in the predominantly general surgery (63%) cohort which they analysed. Aziz et al[26] investigated outcomes of patients undergoing vascular surgery with DNR status and also demonstrated higher mortality in DNR patients, but found similarity in rates of complications between the two groups, except for graft failure, a procedure specific complication. This demonstrates the importance of procedure specific information in discussing risk with patients.
Other emerging literature supports our findings of relatively high mortality among patients with DNR orders who undergo surgery. A recent study by our group[8] examined outcomes among DNR patients undergoing a variety of the most common procedures done for this patient population using NSQIP data. The most common procedures among DNR patients focused on symptom relief but were also associated with higher rates of 30 d mortality (but not morbidity) when compared to non-DNR matched controls[8]. In another analysis focused on DNR patients undergoing hip surgery, the urgency of the procedure (emergent vs non-emergent) was found to cause no independent increase in 30-d morbidity, while DNR status itself again demonstrated high 30-d mortality rates in excess of those predicted by the NSQIP risk calculator[27].
Patients undergoing hip fracture surgery comprise a diverse patient group, making risk stratification important[28,29]. High quality perioperative care and subsequent recovery particularly in the most elderly and medically complex patients presents a growing challenge for an ageing population[10-12]. Ours is among the emerging literature to measure hip fracture surgery outcomes in the presence of a DNR status and quantify the impact of this important risk factor in this common condition. Our analysis demonstrates that at present, 13.6% of all patients undergoing hip fracture surgery have DNR status. This incidence was previously unknown, despite the growing awareness of the higher risk orthogeriatric population. The burden of mortality and morbidity in this population therefore may present a sizeable and specific opportunity for quality improvement[30]. It may also identify a skills gap or systems gap in broaching discussions about end of life wishes in a pre-emptive, comprehensive, acceptable and sensitive fashion. Shared surgical decision making is an emerging topic in the literature, and there have been research and policy agendas proposed for improved perioperative code status discussion between providers involved in perioperative care and patients as well as their families[31].
We report that patients with DNR status undergoing hip fracture surgery were more likely to be female, aged over > 80 years, dyspneic with moderate exertion or rest, ASA class III or IV, partially or totally dependent for activities of daily living or diagnosed with hypertension, diabetes, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), peripheral vascular disease (PVD), prior stroke, weight loss, or sepsis and this is in keeping with patterns described elsewhere[4,25,32,33]. Similar to previous reports on DNR status, we also found patients with DNR status were less likely to report their race/ethnicity and more likely to be underweight (BMI < 18.5)[33-35]. This could also reflect physician inconsistency in discussing end of life and resuscitation status as well as ethnic variations in fragility fractures or even of life expectancy[36,37].
Concern has been expressed previously that DNR status may carry inadvertent care provider bias, or the so-called “failure to rescue” hypothesis. This could lead to inadequate or insufficient care, extending beyond withholding CPR or intubation and ventilation[14]. Our study was not designed to evaluate this specifically, however propensity score matching and regression analysis created a model to compare outcomes in patients with and without DNR status, controlling for age, gender, race, ethnicity, ASA class, functional status, albumin levels and presence of multiple independently significant comorbidities. Additionally, our model matched patients using a frailty index, which may have further eliminated differences between the matched groups based on physical status alone.
Our study found that patients with DNR status had slightly shorter mean anesthesia and surgery times in the unmatched analyses. This may reflect an effort to reduce operative or anesthetic time for higher risk patients, by selecting more senior or experienced staff, or less complex operative procedures[38]. We found the rates of spinal anesthesia were higher for patients who were DNR. This may reflect ongoing debate as to whether spinal anesthesia out-performs general anesthesia in specific patient groups[39,40]. Potential benefits from regional anesthesia, such as reduced respiratory and neurological complications, and reduced opiate consumption and side effects may be more pronounced in high risk patients. This finding was despite the fact that some contraindications to spinal anesthesia, such as anticoagulation, may be more prevalent[39].
The primary limit to this study is fundamental to the retrospective data review design that we were obligated to by the dataset. We were not able to control selection of patients for the surgeries as a result, and therefore sought to address these limitations by our statistical methods, as described above.
The surgical case mix was similar for both groups, though due to a relatively small sample size this could not be analysed in detail. The 10 most common procedures appeared in approximately the same order for both groups, and no gross discrepancies were apparent to visual inspection of the relative proportions. Although our data was able to describe the case mix of procedures undertaken in this population, we were not able to discern sufficient level of detail to describe all aspects of the procedures performed. For instance, although we describe an approximately 15% incidence of total hip arthroplasty, the data set does not provide specific details on the techniques used to accomplish the surgery (e.g., use of cementing agent type, specific screw or prosthesis hardware type). This must be recognized as one of the specific limitations of the study in addition to the general limitations of retrospective administrative and clinical datasets.
Although the emerging literature in this area suggests that shared decision making is a crucial aspect of care for patients with DNR status, our data sources did not allow us to investigate the surgical decision making that preceded the operations among DNR patients in this cohort. Thus, we cannot comment on the specific decision making process that was used in deciding to undergo surgery for hip fracture among these patients. However, this would be a valuable area of future investigation.
However, the mortality and morbidity demonstrated in this study provides a useful reference point for specific discussions about risks of hip fracture surgery, for informed consent, end of life discussions, and for planning perioperative care in this high risk demographic. Importantly, while mortality was higher in DNR status patients, morbidity, defined by post-operative complications, either individually or overall, was generally not higher in the DNR status patients. Indeed, the reduced rate of CPR and unplanned intubation is both expected and consistent with findings in general and other surgical specialities[8]. It is unclear why a small number of patients with DNR status did undergo such resuscitative procedures, or what the events leading to this were. Taken together, it does not seem that an excess burden of post-operative adverse events cannot adequately explain the increased mortality and suggests the need for further research to understand what unmeasured variables account for these consistent differences in outcome. Our findings support the need for routine, systematic, perioperative discussion with hip fracture patients regarding their goals of care in the event of post-operative morbidity leading to cardiopulmonary arrest. Hip fracture surgery has high perioperative mortality, however this data suggests DNR status is effective in reducing specific interventions such as CPR and reintubation, without appearing to increase overall morbidity in the first 30 d after surgery.
Relatively little is known about the exact mechanism through which Do-Not-Resuscitate (DNR) status affects patient outcomes during the perioperative period. The approach of surgical and anesthesia societies has been to treat DNR status as a component of the decision to undergo surgery or as a means of framing surgical goals and expectations with patients and their families. Depending on patients’ goals, DNR status may even be reversed during the perioperative period. However, little is known about how preoperative DNR status affects morbidity and mortality during the perioperative period, if at all.
Patients in the orthogeriatric population who are undergoing hip fracture fixation surgery may be at increased risk for morbidity and/or mortality. Given that these patients have already made a premeditated decision to limit cardiopulmonary resuscitative aspects of their medical care, they may also benefit from additional counselling with regard to any additional risks that may apply to their surgical population.
This study seeks to describe the incidence and distribution of DNR status in patients undergoing hip fracture surgery and to determine whether DNR status is an independent risk factor for worse outcomes on 30-d follow up. The study’s objective was realized by analysis of propensity matched groups of patients in a large retrospective cohort. The study seeks to support an emerging field of literature which describes the unique perioperative outcomes among patients with preoperative DNR/DNI status.
A large, national, US-based retrospective cohort database was used to identify patients undergoing surgical fixation for hip fracture across a variety of geographic and hospital settings. Characteristics of this cohort were examined for unmatched groups of patients with and without DNR/DNI orders, as well as for groups of matched on their propensity for having a DNR/DNI order.
This study demonstrates that when comparing groups of patients that have been matched on propensity for DNR/DNI status, having a DNR/DNI order was independently associated with mortality (OR = 2.04, 95%CI: 1.46-2.86, P < 0.001). Additionally, DNR/DNI status was associated with a very slight increased risk of perioperative complications without otherwise showing significantly different incidences of morbidity between the matched groups.
New findings contributed by this study include insight in the role of DNR/DNI status as an independent predictor of perioperative mortality among patients undergoing hip fracture fixation surgeries. Notably, these matched groups did not demonstrate associations between DNR/DNI status and perioperative morbidity. Given that rates of CPR and reintubation were markedly lower in the DNR/DNI group, we demonstrate that there may be a “ceilings of care” effect in this context. The findings also raises a question as to whether a “failure to rescue” mechanism may be active among these patients in the perioperative period. Regardless, the results of this study raise questions for future research which will hopefully yield additional insight into the mechanisms driving increased mortality among patients with DNR/DNI status who are undergoing surgery for hip fracture. In the immediate term, these findings will assist clinicians in appropriately counselling patients who may have a DNR/DNI order and are undergoing surgery for hip fracture.
Future research will hopefully yield additional insight into the mechanisms driving increased mortality among patients with DNR/DNI status who are undergoing surgery for hip fracture.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cui Q, Lepetsos P, Malik H, Sun TS S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Burns JP, Edwards J, Johnson J, Cassem NH, Truog RD. Do-not-resuscitate order after 25 years. Crit Care Med. 2003;31:1543-1550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 108] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Loertscher L, Reed DA, Bannon MP, Mueller PS. Cardiopulmonary resuscitation and do-not-resuscitate orders: a guide for clinicians. Am J Med. 2010;123:4-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Morrell ED, Brown BP, Qi R, Drabiak K, Helft PR. The do-not-resuscitate order: associations with advance directives, physician specialty and documentation of discussion 15 years after the Patient Self-Determination Act. J Med Ethics. 2008;34:642-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Hakim RB, Teno JM, Harrell FE Jr, Knaus WA, Wenger N, Phillips RS, Layde P, Califf R, Connors AF Jr, Lynn J. Factors associated with do-not-resuscitate orders: patients’ preferences, prognoses, and physicians’ judgments. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Ann Intern Med. 1996;125:284-293. [PubMed] |
| 5. | Clemency MV, Thompson NJ. Do not resuscitate orders in the perioperative period: patient perspectives. Anesth Analg. 1997;84:859-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Cherniack EP. Increasing use of DNR orders in the elderly worldwide: whose choice is it? J Med Ethics. 2002;28:303-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 7. | American Society of Anesthesiologists. Ethical guidelines for the anesthesia care of patients with do-not-resuscitate orders or other directives that limit treatment. [last amended. 2013;Oct 16] Available from: http://www.asahq.org/~/media/Sites/ASAHQ/Files/Public/Resources/standards-guidelines/ethical-guidelines-for-the-anesthesia-care-of-patients.pdf. |
| 8. | Walsh EC, Brovman EY, Bader AM, Urman RD. Do-Not-Resuscitate Status Is Associated With Increased Mortality But Not Morbidity. Anesth Analg. 2017;125:1484-1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Berstock JR, Beswick AD, Lenguerrand E, Whitehouse MR, Blom AW. Mortality after total hip replacement surgery: A systematic review. Bone Joint Res. 2014;3:175-182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 128] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 10. | Le Manach Y, Collins G, Bhandari M, Bessissow A, Boddaert J, Khiami F, Chaudhry H, De Beer J, Riou B, Landais P. Outcomes After Hip Fracture Surgery Compared With Elective Total Hip Replacement. JAMA. 2015;314:1159-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 161] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 11. | Ooi LH, Wong TH, Toh CL, Wong HP. Hip fractures in nonagenarians--a study on operative and non-operative management. Injury. 2005;36:142-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Sathiyakumar V, Greenberg SE, Molina CS, Thakore RV, Obremskey WT, Sethi MK. Hip fractures are risky business: an analysis of the NSQIP data. Injury. 2015;46:703-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 13. | Saager L, Kurz A, Deogaonkar A, You J, Mascha EJ, Jahan A, Turner PL, Sessler DI, Turan A. Pre-existing do-not-resuscitate orders are not associated with increased postoperative morbidity at 30 days in surgical patients. Crit Care Med. 2011;39:1036-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Scarborough JE, Pappas TN, Bennett KM, Lagoo-Deenadayalan S. Failure-to-pursue rescue: explaining excess mortality in elderly emergency general surgical patients with preexisting “do-not-resuscitate” orders. Ann Surg. 2012;256:453-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 15. | Shepardson LB, Youngner SJ, Speroff T, Rosenthal GE. Increased risk of death in patients with do-not-resuscitate orders. Med Care. 1999;37:727-737. [PubMed] |
| 16. | Steinberg SM, Popa MR, Michalek JA, Bethel MJ, Ellison EC. Comparison of risk adjustment methodologies in surgical quality improvement. Surgery. 2008;144:662-667; discussion 662-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 122] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 17. | Yuen JK, Reid MC, Fetters MD. Hospital do-not-resuscitate orders: why they have failed and how to fix them. J Gen Intern Med. 2011;26:791-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 88] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Schmolders J, Friedrich MJ, Michel R, Strauss AC, Wimmer MD, Randau TM, Pennekamp PH, Wirtz DC, Gravius S. Validation of the Charlson comorbidity index in patients undergoing revision total hip arthroplasty. Int Orthop. 2015;39:1771-1777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Bannay A, Chaignot C, Blotière PO, Basson M, Weill A, Ricordeau P, Alla F. The Best Use of the Charlson Comorbidity Index With Electronic Health Care Database to Predict Mortality. Med Care. 2016;54:188-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 340] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 20. | Lakomkin N, Goz V, Lajam CM, Iorio R, Bosco JA 3rd. Higher Modified Charlson Index Scores Are Associated With Increased Incidence of Complications, Transfusion Events, and Length of Stay Following Revision Hip Arthroplasty. J Arthroplasty. 2017;32:1121-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 21. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32099] [Cited by in RCA: 38321] [Article Influence: 1008.4] [Reference Citation Analysis (0)] |
| 22. | Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4103] [Cited by in RCA: 5824] [Article Influence: 291.2] [Reference Citation Analysis (0)] |
| 23. | Velanovich V, Antoine H, Swartz A, Peters D, Rubinfeld I. Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res. 2013;183:104-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 413] [Cited by in RCA: 634] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 24. | American College of Surgeions. Statement on advance directives by patients: “do not resuscitate” in the operating room. Bull Am Coll Surg. 2014;99:42-43. [PubMed] |
| 25. | Kazaure H, Roman S, Sosa JA. High mortality in surgical patients with do-not-resuscitate orders: analysis of 8256 patients. Arch Surg. 2011;146:922-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 26. | Aziz H, Branco BC, Braun J, Hughes JD, Goshima KR, Trinidad-Hernandez M, Hunter G, Mills JL Sr. The influence of do-not-resuscitate status on the outcomes of patients undergoing emergency vascular operations. J Vasc Surg. 2015;61:1538-1542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Beverly A, Brovman EY, Urman RD. Comparison of Postoperative Outcomes in Elderly Patients With a Do-Not-Resuscitate Order Undergoing Elective and Nonelective Hip Surgery. Geriatr Orthop Surg Rehabil. 2017;8:78-86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 28. | Abad-Díez JM, Calderón-Larrañaga A, Poncel-Falcó A, Poblador-Plou B, Calderón-Meza JM, Sicras-Mainar A, Clerencia-Sierra M, Prados-Torres A. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. 2014;14:75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 155] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 29. | Mandels M. Microbial sources of cellulase. Biotechnol Bioeng Symp. 1975;81-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 386] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 30. | Dall TM, Gallo PD, Chakrabarti R, West T, Semilla AP, Storm MV. An aging population and growing disease burden will require a large and specialized health care workforce by 2025. Health Aff (Millwood). 2013;32:2013-2020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 333] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 31. | Hickey TR, Cooper Z, Urman RD, Hepner DL, Bader AM. An Agenda for Improving Perioperative Code Status Discussion. A A Case Rep. 2016;6:411-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 32. | Silvennoinen K, Meretoja A, Strbian D, Putaala J, Kaste M, Tatlisumak T. Do-not-resuscitate (DNR) orders in patients with intracerebral hemorrhage. Int J Stroke. 2014;9:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 33. | Wenger NS, Pearson ML, Desmond KA, Harrison ER, Rubenstein LV, Rogers WH, Kahn KL. Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med. 1995;155:2056-2062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 126] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 34. | Nakagawa K, Vento MA, Seto TB, Koenig MA, Asai SM, Chang CW, Hemphill JC 3rd. Sex differences in the use of early do-not-resuscitate orders after intracerebral hemorrhage. Stroke. 2013;44:3229-3231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 35. | Salottolo K, Offner PJ, Orlando A, Slone DS, Mains CW, Carrick M, Bar-Or D. The epidemiology of do-not-resuscitate orders in patients with trauma: a community level one trauma center observational experience. Scand J Trauma Resusc Emerg Med. 2015;23:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Curtis EM, van der Velde R, Moon RJ, van den Bergh JP, Geusens P, de Vries F, van Staa TP, Cooper C, Harvey NC. Epidemiology of fractures in the United Kingdom 1988-2012: Variation with age, sex, geography, ethnicity and socioeconomic status. Bone. 2016;87:19-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 301] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 37. | Cauley JA. Defining ethnic and racial differences in osteoporosis and fragility fractures. Clin Orthop Relat Res. 2011;469: 1891-1899. [RCA] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 168] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 38. | Raval MV, Wang X, Cohen ME, Ingraham AM, Bentrem DJ, Dimick JB, Flynn T, Hall BL, Ko CY. The influence of resident involvement on surgical outcomes. J Am Coll Surg. 2011;212:889-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 205] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 39. | Opperer M, Danninger T, Stundner O, Memtsoudis SG. Perioperative outcomes and type of anesthesia in hip surgical patients: An evidence based review. World J Orthop. 2014;5:336-343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 50] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 40. | Basques BA, Toy JO, Bohl DD, Golinvaux NS, Grauer JN. General compared with spinal anesthesia for total hip arthroplasty. J Bone Joint Surg Am. 2015;97:455-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 170] [Article Influence: 17.0] [Reference Citation Analysis (0)] |