Published online Dec 18, 2017. doi: 10.5312/wjo.v8.i12.895
Peer-review started: August 16, 2017
First decision: October 9, 2017
Revised: October 11, 2017
Accepted: November 22, 2017
Article in press: November 22, 2017
Published online: December 18, 2017
Processing time: 124 Days and 15 Hours
To research the influence of season of the year on periprosthetic joint infections.
We conducted a retrospective review of the entire Medicare files from 2005 to 2014. Seasons were classified as spring, summer, fall or winter. Regional variations were accounted for by dividing patients into four geographic regions as per the United States Census Bureau (Northeast, Midwest, West and South). Acute postoperative infection and deep periprosthetic infections within 90 d after surgery were tracked.
In all regions, winter had the highest incidence of periprosthetic infections (mean 0.98%, SD 0.1%) and was significantly higher than other seasons in the Midwest, South and West (P < 0.05 for all) but not the Northeast (P = 0.358). Acute postoperative infection rates were more frequent in the summer and were significantly affected by season of the year in the West.
Season of the year is a risk factor for periprosthetic joint infection following total hip arthroplasty (THA). Understanding the influence of season on outcomes following THA is essential when risk-stratifying patients to optimize outcomes and reduce episode of care costs.
Core tip: Season of the year when a total hip arthroplasty is performed may affect 90-d post-operative outcomes in certain regions of the United States. Furthermore, there appears to be a difference of the effect of seasonal variation on the outcomes as superficial infections have different patterns compared to deep peri-prosthetic joint infection.
- Citation: Rosas S, Ong AC, Buller LT, Sabeh KG, Law TY, Roche MW, Hernandez VH. Season of the year influences infection rates following total hip arthroplasty. World J Orthop 2017; 8(12): 895-901
- URL: https://www.wjgnet.com/2218-5836/full/v8/i12/895.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i12.895
Total hip arthroplasty is one of the most common orthopaedic procedures in the United States, with over 600000 performed annually[1,2]. Though this procedure has societal and personal benefits for patients, it is not without risks[3]. Complications following THA range from increased length of stay to circulatory collapse and death. While minor and major complications are infrequent[4,5] their impact on readmissions and postdischarge care represents a significant portion of the episode payment[6]. Factors increasing the likelihood of complications are of great interest, as risk minimization strategies have been shown to reduce overall cost in THA[7]. Hospital type, surgeon volume, comorbidities and other modifiable risk factors have recently been studied in great detail[4,8-13]. However, non-modifiable risk factors have also been elucidated as important for pre-operative risk stratification[14-17].
Recently, the influence of seasonality on outcomes in various surgical subspecialties has been investigated[14,18-21]. How season or climate impacts outcomes following THA remains unknown, with the only evidence originating from a single institution, retrospective study by Kane et al[22] who demonstrated an association between summer and infection. In the United States, seasonality affects aspects of life in a variety of manners[23]. Winter months encourage a sedentary lifestyle, changes eating patterns and results in fewer follow up visits[24-27]. In contrast, the increased temperatures and humidity of summer months improves microbe survivorship, increases vitamin D levels, encourages being outdoors and overall activity levels[28]. Given the impact of seasonality on such diverse aspects of life, this study sought to elucidate the influence of season of the year and geographic location on outcomes following THA at a national level. To improve the relevance of this study, we chose to compare differences in the incidence of postoperative infections within the 90-d period, simulating an episode of care period as put forth by the Comprehensive Care for Joint Replacement (CJR) Model.
We conducted a retrospective case-control, level of evidence III study, evaluating the effects of season of the year on two types of infections following THA. This was achieved by analysis of the Medicare patient database. The query was performed through the Pearldiver Supercomputer (Warsaw, IN, United States). The supercomputer allows identification of patient records through international classification of disease (ICD) ninth revision codes. Patients were then stratified by season of surgery. The seasons were defined as follows: Spring (March, April and May), summer: (June, July and August), fall (September, October and November), winter (December, January and February). Demographical data including age, gender and region of the United States were the surgery was performed was gathered at baseline. Geographical region was classified according to the United States Census Bureau as follows: Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin. Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island and Vermont. South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington and Wyoming.
Patients and outcomes were tracked for 90 d. Using previously described methodology; ICD-9 codes were used to identify complications[9-11,29,30]. The following outcomes were tracked: acute post-operative infection (998.5), osteomyelitis (730) and infection of orthopaedic device (996.66). Infections were then subdivided into acute postoperative infection (ICD-998.5) and deep infection (ICD-996.66 and 730). This methodology of separating infections has also been previously described[9-11,29,30]. The incidence of complications was compared through Chi-squares with Yates corrections given the large sample size of the study. Statistical analysis was conducted through SPSS version 20 (IBM, Armonk, NY, United States). An alpha value less than 0.05 was deemed statistically significant.
A cohort representative of 1311672 patients who underwent THA between 2005 and 2014 was identified. The seasonal distribution of procedures was similar: 25% in the spring, 26.9% in the summer, 25% in the fall and 24% in the winter. Regional volume varied significantly (P < 0.001) with the south performing the majority of surgeries (35%) followed by the mid-west (28%), the northeast (19%) and the west (18%) (Table 1).
| NE | MW | WE | SO | |
| Female | 61.60% | 61.10% | 60.60% | 61.40% |
| Male | 38.40% | 38.90% | 39.40% | 38.60% |
| Age (yr) | 9% | 9% | 9% | 12% |
| ≤ 64 | 9% | 9% | 9% | 12% |
| 65-69 | 23% | 24% | 26% | 24% |
| 70-74 | 22% | 22% | 23% | 22% |
| 75-79 | 21% | 21% | 20% | 20% |
| 80-84 | 16% | 15% | 14% | 14% |
| ≥ 85 | 10% | 9% | 9% | 8% |
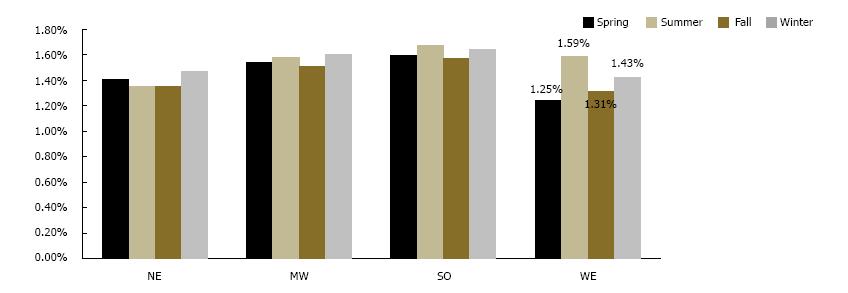
There was a significant difference in the incidence of acute postoperative infections by season in the West (Table 2). The greatest incidence in the West was following surgeries performed in the summer (1.59%), which was significantly greater than all other seasons (P < 0.001 for all) (Figure 1). There was no difference in acute postoperative infections when stratified by season in the other regions.
| Location | Spring | Summer | Fall | Winter | χ2 |
| North East | 1.41% | 1.35% | 1.35% | 1.47% | 0.281 |
| Mid West | 1.54% | 1.59% | 1.51% | 1.60% | 0.39 |
| South | 1.60% | 1.68% | 1.58% | 1.64% | 0.277 |
| West | 1.25% | 1.59% | 1.31% | 1.43% | < 0.001 |
| Mean | 1.45% | 1.55% | 1.44% | 1.54% | |
| SD | 0.16% | 0.14% | 0.13% | 0.10% |
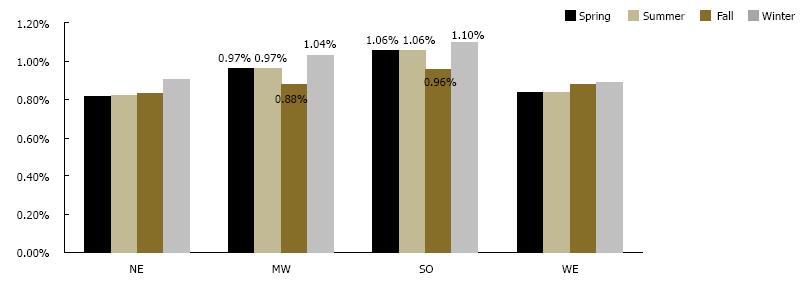
Our analysis demonstrated that season of the year had a significant effect on periprosthetic joint infections in two out of the four regions, Midwest and South (Table 3). The mean incidence in the Northeast and West was 0.85% (range 0.82% to 0.91%, P = 0.358) and 0.86% (range 0.84% to 0.89%, P = 0.680), respectively. The Midwest region had the highest incidence of periprosthetic infections in the winter 1.04%, which was significantly higher than the fall (0.88%, P = 0.001) but not higher than other seasons (P = 0.175 vs the summer and P = 0.155 vs the spring). There were no significant differences when comparing the remaining seasons. In the South, the highest incidence of periprosthetic infections was also seen in the winter (1.1%), which was significantly higher than the fall 0.96% (P < 0.001) but not than the summer or spring, both 1.06% (P = 0.377 and 0.344 respectively). In the South, the fall had a lower incidence, 0.96%, compared to the spring (P = 0.018) and to the summer (P = 0.005) (Figure 2).
| Location | Spring | Summer | Fall | Winter | χ2 |
| North East | 0.82% | 0.83% | 0.84% | 0.91% | 0.358 |
| Mid West | 0.97% | 0.97% | 0.88% | 1.04% | 0.013 |
| South | 1.06% | 1.06% | 0.96% | 1.10% | 0.007 |
| West | 0.84% | 0.84% | 0.88% | 0.89% | 0.68 |
| Mean | 0.92% | 0.92% | 0.89% | 0.98% | |
| SD | 0.11% | 0.11% | 0.05% | 0.10% |
This study sought to determine the effect of season of the year, a non-modifiable risk factor, on infections following THA. This was achieved by scrutinizing the entire Medicare population from 2005 to 2014 for the outcomes of interest during the 90-d post-operative period. Our analysis of over 1 million patients demonstrated that acute postoperative infections are significantly affected by season in certain geographical regions. These results are similar to the work of Kane et al[22], who reported infection rates during summer of 4.7%, fall 2.4%, winter 1.5% and spring 0.5%. Although the authors did not differentiate between deep and superficial infections, they highlight that humidity; colonization and the implementation of new house staff (“July effect”) might be responsible for the reported findings. Similarly, various studies have demonstrated a seasonal variation in the rates of surgical site infections from Staphylococcus aureus, which is the main cause of superficial infections among orthopaedic patients[14,19,31,32]. The seasonal influence of the microbes in conjunction with increased sweat gland output, skin hydration, and elevated temperatures may all contribute to the seasonal variation observed here[20,28,32]. Conversely, the relative consistency of the weather in the South, with warmer year-round temperatures, may account for the lack of statistically significant variation in this region. Previous studies have found differences in infection rates are more pronounced in particular regions of the United States, which was also reported in the present study[32].
The overall incidence of periprosthetic joint infections reported in this study (0.89%-0.98%) is similar to epidemiological studies by Kurtz et al[33] who reported an overall incidence of 2% with variation by training center from 0.61% in rural hospitals to 0.73% at urban-teaching hospitals to 1.18% in Urban-non-teaching hospitals[34]. This study also found a significant variation in the total number of procedures performed when stratified by geographic region, with the South performing the highest volume of cases. Thakore et al[35] reported similar results with the number of average discharges billed to Medicare at each hospital highest in the Midwest, followed by the South, Northeast and West. Similarly, this study demonstrated a seasonal variation in the incidence of infection in certain regions of the United States. The Midwest and the South were found to have higher rates of infection in the winter (1.04% and 1.1%, respectively). Previous studies in spine surgery have found a greater incidence of infectious complications in the summer (4.1%) followed by the fall (3.9%)[31]. However, these authors did not differentiate between superficial and deep infections and classified patients based on the surgical site infection classification. Similar findings were also reported by Kestle et al[36], who concluded that there is an increased risk of infections attributable to the “July effect,” based on data from 737 patients treated in Canada. Nonetheless, these articles did not analyse a national sample stratified by region and potential reasons for the higher periprosthetic infection rate seen in the winter include longer length of stay because of travel/discharge difficulties, decreased patient compliance with post-operative care or difficulty making follow up appointments. The “July” effect which refers to incoming house staff lack of experience has been suggested as a cause of increased infections following surgical management of certain entities, but this has not held true in the arthroplasty literature[31]. Although our study did not stratify by hospital type (teaching vs non-teaching), demonstration that periprosthetic joint infections are more common in the winter suggests incoming residents may not be at fault[14,18].
Although our study demonstrates certain differences in infection rates by season of the year and by region, we demonstrated that “superficial infections” have different variations that “deep infections” which although controversial, may be due to various reasons: first, the increased risk of superficial infections in the summer may be related to the increased in temperature as has been postulated by Anthony et al[37] in their large population-based study of the National Inpatient Sample. The authors conducted a comprehensive examination of the NIS and accounted for patient factors, hospital factors and weather variations with their models. Furthermore, the authors state that bacteria can colonize different skin areas at different concentration as temperature varies. Unfortunately, less is known about the seasonality of deep infections. Some authors have demonstrated a seasonal variation in bacteraemia in hospitalized patients, but bacteraemia does not always cause a joint infection and as such limited information can be extracted from this[38]. Thus, with such little evidence available no definite conclusion can be made of why such variation exists.
This study is not without its limitations. Being a retrospective review, there is potential for selection bias due to the way patients were stratified. This bias was minimized, as the number of THAs in each group was similar. As a large database study, another source of selection bias might have been the coding of the procedures and/or the outcomes, which is beyond the author’s control. Although we relied on previously published literature regarding the identification of the outcomes, it is possible that coding errors may have influenced our results. However, the importance of coding on reimbursements, decreases this likelihood. Time-lead bias may also play a part in the significance of our results as the outcomes are tracked for 90 d following the procedures that occurred within a 3-mo period and thus we cannot account for whether a procedure was performed at the beginning or end of that 3-mo period that comprised a season of the year.
In conclusion, season of the year, which is a non-modifiable risk factor, influences the rate of postoperative infections following THA in some regions of the United States. Superficial, acute post-operative infections are more commonly seen after THAs performed in the summer and periprosthetic joint infections more frequently occur in THAs performed in the winter. Understanding that seasonality is a risk factor for periprosthetic joint infection following THA is essential when risk stratifying patients that are a part of a bundled payment reimbursement model.
Limited information is available in regard to the correlation between season of the year when a surgery is performed to the outcomes of the surgery. Weather variations may account for different bacterial patterns that may lead to infection. Thus, we studied the effects of season of the year on the infectious outcomes after total hip arthroplasty in the United States Medicare patient population.
Due to the large effect on morbidity, mortality and cost that infections can cause, it is important to study modifiable and non-modifiable risk factors for adverse outcomes after surgery. By identifying a seasonal variation in post-operative outcomes, one may ultimately use this information to delay elective surgery.
The purpose of this study was to determine if season of the year when a total hip arthroplasty is performed had an effect on 90-d post-operative superficial and deep infections among Medicare beneficiaries in the United States. The study identified certain seasonal differences that should promote research on this subject through prospective studies.
The authors conducted a retrospective review of the entire Medicare files and stratified patients by region and season when the surgery was performed. The authors evaluated the 90-d post-operative period after the procedure to determine the incidence of these complications. The authors analyzed the entire Medicare records from 2005 to 2014. Comparative statistical analysis was used to compare the 90-d incidences reported by international classification of disease 9th edition code tracked in the patient file.
There was a significant difference in the incidence of acute postoperative infections by season in the West. The greatest incidence in this region (West) was following surgeries performed in the summer (1.59%), which was significantly greater than all other seasons (P < 0.001 for all). Our analysis demonstrated that season of the year had a significant effect on periprosthetic joint infections in two out of the four regions, Midwest and South. These results help demonstrate that variation exists in certain regions of the United States by season of the year and that more research is needed on this non-modifiable risk factor.
There were no previous articles in the literature describing seasonal variation of outcomes after lower extremity arthroplasty. The new findings of this study is: Season of the year may influence post-operative outcomes after total hip arthroplasty. This study proposes the new theories that seasonal variation of these outcomes varies and that the seasonal variability between superficial infection and peri-prosthetic infection exists. This study offered the original insights into the current knowledge by providing evidence that there is regional and seasonal variation in outcomes. This study proposed the new hypotheses that temperature and weather variations may lead to different infectious complications after hip arthroplasty. The authos proposed the new methods that prospective trials to investigate the effect of not only season of the year when the surgery is performed affect the outcomes but also weather. We found the new phenomena that certain regions of the United States have different post-operative complication rates of infectious outcomes after THA when stratified by season of the year when the surgery was performed. Through experiments in this study, the authors confirmed the hypotheses that seasonal variation exists in infectious outcomes after THA in certain regions of the United States. In the future, non-modifiable risk factors may play a role in the outcome of THA such as season of the year when the surgery is performed.
Season of the year when surgery is performed may have an effect on complication rates after THA. Future studies should create models that account for weather and seasonal variations in the study of outcomes after arthroplasty procedures.
We would like to acknowledge Daniel Bracey, MD, PhD for his help with the audio tip recording.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cui QT, Lepetsos P S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Singh JA. Epidemiology of knee and hip arthroplasty: a systematic review. Open Orthop J. 2011;5:80-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 213] [Cited by in RCA: 242] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 2. | Kowalik TD, DeHart M, Gehling H, Gehling P, Schabel K, Duwelius P, Mirza A. The Epidemiology of Primary and Revision Total Hip Arthroplasty in Teaching and Nonteaching Hospitals in the United States. J Am Acad Orthop Surg. 2016;24:393-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275:858-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 304] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 4. | Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2003;85-A:27-32. [PubMed] |
| 5. | Gundtoft PH, Pedersen AB, Varnum C, Overgaard S. Increased Mortality After Prosthetic Joint Infection in Primary THA. Clin Orthop Relat Res. 2017;475:2623-2631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 159] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 6. | Bozic KJ, Ward L, Vail TP, Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clin Orthop Relat Res. 2014;472:188-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 357] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 7. | Navathe AS, Troxel AB, Liao JM, Nan N, Zhu J, Zhong W, Emanuel EJ. Cost of Joint Replacement Using Bundled Payment Models. JAMA Intern Med. 2017;177:214-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 250] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 8. | Johnsen SP, Sørensen HT, Lucht U, Søballe K, Overgaard S, Pedersen AB. Patient-related predictors of implant failure after primary total hip replacement in the initial, short- and long-terms. A nationwide Danish follow-up study including 36,984 patients. J Bone Joint Surg Br. 2006;88:1303-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 112] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 9. | Best MJ, Buller LT, Gosthe RG, Klika AK, Barsoum WK. Alcohol Misuse is an Independent Risk Factor for Poorer Postoperative Outcomes Following Primary Total Hip and Total Knee Arthroplasty. J Arthroplasty. 2015;30:1293-1298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Best MJ, Buller LT, Klika AK, Barsoum WK. Increase in perioperative complications following primary total hip and knee arthroplasty in patients with hepatitis C without cirrhosis. J Arthroplasty. 2015;30:663-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Best MJ, Buller LT, Klika AK, Barsoum WK. Outcomes Following Primary Total Hip or Knee Arthroplasty in Substance Misusers. J Arthroplasty. 2015;30:1137-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 12. | Tischler EH, Matsen Ko L, Chen AF, Maltenfort MG, Schroeder J, Austin MS. Smoking Increases the Rate of Reoperation for Infection within 90 Days After Primary Total Joint Arthroplasty. J Bone Joint Surg Am. 2017;99:295-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 63] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 13. | Wagner ER, Kamath AF, Fruth KM, Harmsen WS, Berry DJ. Effect of Body Mass Index on Complications and Reoperations After Total Hip Arthroplasty. J Bone Joint Surg Am. 2016;98:169-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 153] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 14. | Durkin MJ, Dicks KV, Baker AW, Moehring RW, Chen LF, Sexton DJ, Lewis SS, Anderson DJ. Postoperative infection in spine surgery: does the month matter? J Neurosurg Spine. 2015;23:128-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 15. | O’Neal RM, Cryer KA, Edwards PK, Barnes CL, Mears SC. Narcotic Use: A Modifiable Risk Factor for Hip and Knee Arthroplasty. J Surg Orthop Adv. 2016;25:227-233. [PubMed] |
| 16. | Bass AR, McHugh K, Fields K, Goto R, Parks ML, Goodman SM. Higher Total Knee Arthroplasty Revision Rates Among United States Blacks Than Whites: A Systematic Literature Review and Meta-Analysis. J Bone Joint Surg Am. 2016;98:2103-2108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 17. | Martsolf GR, Barrett ML, Weiss AJ, Kandrack R, Washington R, Steiner CA, Mehrotra A, SooHoo NF, Coffey R. Impact of Race/Ethnicity and Socioeconomic Status on Risk-Adjusted Hospital Readmission Rates Following Hip and Knee Arthroplasty. J Bone Joint Surg Am. 2016;98:1385-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 18. | Banco SP, Vaccaro AR, Blam O, Eck JC, Cotler JM, Hilibrand AS, Albert TJ, Murphey S. Spine infections: variations in incidence during the academic year. Spine (Phila Pa 1976). 2002;27:962-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Isgren CM, Salem SE, Archer DC, Worsman FC, Townsend NB. Risk factors for surgical site infection following laparotomy: Effect of season and perioperative variables and reporting of bacterial isolates in 287 horses. Equine Vet J. 2017;49:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Kao HK, Chen MC, Lee WC, Yang WE, Chang CH. Seasonal Temperature and Pin Site Care Regimen Affect the Incidence of Pin Site Infection in Pediatric Supracondylar Humeral Fractures. Biomed Res Int. 2015;2015:838913. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Odén A, Kanis JA, McCloskey EV, Johansson H. The effect of latitude on the risk and seasonal variation in hip fracture in Sweden. J Bone Miner Res. 2014;29:2217-2223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Kane P, Chen C, Post Z, Radcliff K, Orozco F, Ong A. Seasonality of infection rates after total joint arthroplasty. Orthopedics. 2014;37:e182-e186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 23. | Mirchandani S, Aharonoff GB, Hiebert R, Capla EL, Zuckerman JD, Koval KJ. The effects of weather and seasonality on hip fracture incidence in older adults. Orthopedics. 2005;28:149-155. [PubMed] |
| 24. | Alvarez-Nebreda ML, Jiménez AB, Rodríguez P, Serra JA. Epidemiology of hip fracture in the elderly in Spain. Bone. 2008;42:278-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 151] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 25. | Grønskag AB, Forsmo S, Romundstad P, Langhammer A, Schei B. Incidence and seasonal variation in hip fracture incidence among elderly women in Norway. The HUNT Study. Bone. 2010;46:1294-1298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Solbakken SM, Magnus JH, Meyer HE, Emaus N, Tell GS, Holvik K, Grimnes G, Forsmo S, Schei B, Søgaard AJ. Impact of comorbidity, age, and gender on seasonal variation in hip fracture incidence. A NOREPOS study. Arch Osteoporos. 2014;9:191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 27. | Koren L, Barak A, Norman D, Sachs O, Peled E. Effect of seasonality, weather and holidays on the incidence of proximal hip fracture. Isr Med Assoc J. 2014;16:299-302. [PubMed] |
| 28. | Leekha S, Diekema DJ, Perencevich EN. Seasonality of staphylococcal infections. Clin Microbiol Infect. 2012;18:927-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 105] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 29. | Buller LT, Best MJ, Klika AK, Barsoum WK. The influence of psychiatric comorbidity on perioperative outcomes following primary total hip and knee arthroplasty; a 17-year analysis of the National Hospital Discharge Survey database. J Arthroplasty. 2015;30:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 117] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 30. | Roche MW, Law TY, Triplet JJ, Hubbard ZS, Kurowicki J, Rosas S. Effect of Hypoglycemia on the Incidence of Revision in Total Knee Arthroplasty. J Arthroplasty. 2017;32:499-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Gruskay J, Smith J, Kepler CK, Radcliff K, Harrop J, Albert T, Vaccaro A. The seasonality of postoperative infection in spine surgery. J Neurosurg Spine. 2013;18:57-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 32. | Klein EY, Sun L, Smith DL, Laxminarayan R. The changing epidemiology of methicillin-resistant Staphylococcus aureus in the United States: a national observational study. Am J Epidemiol. 2013;177:666-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 121] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 33. | Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27:61-5.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1101] [Cited by in RCA: 1218] [Article Influence: 93.7] [Reference Citation Analysis (0)] |
| 34. | Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008;23:984-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 708] [Cited by in RCA: 762] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 35. | Thakore RV, Greenberg SE, Bulka CM, Ehrenfeld JM, Obremskey WT, Sethi MK. Geographic variations in hospital charges and Medicare payments for major joint arthroplasty. J Arthroplasty. 2015;30:728-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Kestle JR, Cochrane DD, Drake JM. Shunt insertion in the summer: is it safe? JNS. 2006;105 Suppl 3:165-168. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 37. | Anthony CA, Peterson RA, Polgreen LA, Sewell DK, Polgreen PM. The Seasonal Variability in Surgical Site Infections and the Association With Warmer Weather: A Population-Based Investigation. Infect Control Hosp Epidemiol. 2017;38:809-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 38. | Eber MR, Shardell M, Schweizer ML, Laxminarayan R, Perencevich EN. Seasonal and temperature-associated increases in gram-negative bacterial bloodstream infections among hospitalized patients. PLoS One. 2011;6:e25298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 123] [Article Influence: 8.8] [Reference Citation Analysis (0)] |