Published online Sep 18, 2016. doi: 10.5312/wjo.v7.i9.584
Peer-review started: March 30, 2016
First decision: May 13, 2016
Revised: May 28, 2016
Accepted: June 27, 2016
Article in press: June 29, 2016
Published online: September 18, 2016
Processing time: 168 Days and 21.9 Hours
To review and report functional outcomes, complications, and survivorship associated with total knee arthroplasty (TKA) in the treatment of post-traumatic arthritis (PTA).
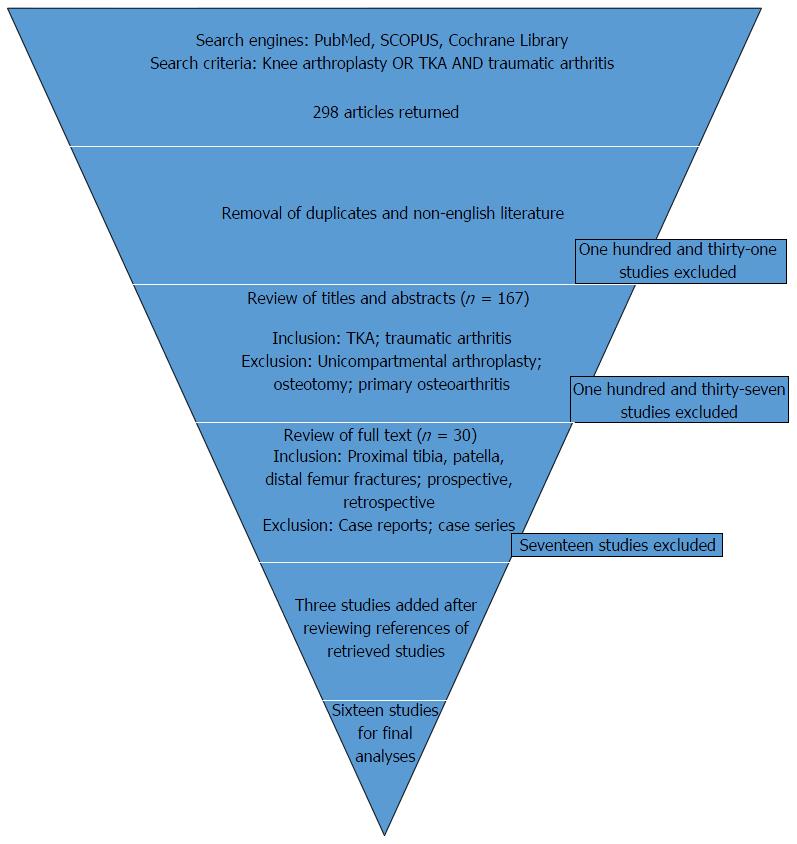
We conducted a systematic review according to the PRISMA guidelines. We searched PubMed, Cochrane Library, and SCOPUS in December 2015 for English-language clinical research studies, both prospective and retrospective, examining the use of TKA for the treatment of PTA. All relevant articles were accessed in full. The manual search included references of retrieved articles. We extracted data on patients’ demographics and clinical outcomes, including preoperative diagnosis and pre- and post-operative functional scores. We summarized the data and reported the results in tables and text.
Sixteen studies, four prospective and ten retrospective, examined patients who underwent TKA for PTA due to fractures of the proximal tibia, patella, and/or distal femur. Eleven studies utilized the Knee Society Scores criteria to assess functional outcomes. All studies utilizing these criteria reported an improvement in functional and knee scores of patients following TKA. Further, studies reported an increased range of motion (ROM) and reduction of pain following surgery. The most commonly reported complications with TKA included infection, stiffness, wound complications, intraoperative rupture of tendons, and osteolysis/polyethylene wear. The overwhelming majority of these complications occurred within the first two years following surgery. Six studies examined the survivorship of TKA with subsequent revision for any reason as an endpoint. Compared to patients with osteoarthritis, patients with PTA required more revisions, the majority for polyethylene wear.
Although associated with higher complication rates, TKA is an effective treatment for PTA, as it improves ROM, pain and functional outcomes.
Core tip: There is a paucity in the literature regarding the effectiveness of total knee arthroplasty (TKA) for the treatment of post-traumatic arthritis (PTA). The goal of this systematic review is to summarize the functional outcomes, complications, and survivorship of TKA performed for the treatment of PTA. Majority of studies reported improvements in functional outcomes, increased range of motion, and decreased pain following TKA. There is a significant complication rate, including infection, stiffness, and wound complications. Revisions were performed most commonly for polyethylene wear. Although associated with higher complication rates, TKA is an effective treatment for PTA, as it improves range of motion, pain and functional outcomes.
- Citation: Saleh H, Yu S, Vigdorchik J, Schwarzkopf R. Total knee arthroplasty for treatment of post-traumatic arthritis: Systematic review. World J Orthop 2016; 7(9): 584-591
- URL: https://www.wjgnet.com/2218-5836/full/v7/i9/584.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i9.584
Post-traumatic arthritis (PTA) refers to structural damage following an injury to an articulating joint[1]. It commonly affects younger, more active individuals as they are more likely to participate in such activities that may cause injury (i.e., sports, blunt trauma, motor vehicle accidents, etc.)[1]. Although any joint in the body may be involved, PTA is often more notable in weight-bearing joints[1]. It is estimated that 12% of all symptomatic osteoarthritis (OA) of the hip, knee, and ankle are due to PTA[2]. With a varied prevalence of 21%-44% reported in the literature, PTA of the knee occurs following intra- or extra-articular fractures of the proximal tibia, patella, and distal femur[3-5]. A combination of factors most likely contributes to the development of PTA following injury to the knee. First, mechanical imbalance may be due to ligamentous laxity, meniscal tears and malalignment[1]. Second, the release of pro-inflammatory cytokines into local tissue leads to imperfect remodeling of the cartilage. Lastly, non-unions and malunions following fractures may lead to PTA[4].
The treatment of PTA can be divided into non-operative and operative management. Activity modification, anti-inflammatory medications, ambulatory assist devices, and physical therapy are the mainstay of non-operative treatment[1]. After these are exhausted, surgical options range from arthroscopic debridement to arthrodesis[6]. Total knee arthroplasty (TKA) is an option for the treatment of end-stage PTA[7].
There is a paucity in the literature regarding TKA for the treatment of PTA. Compared to TKA for patients with primary OA, TKA performed for PTA is often more technically challenging due to previous surgeries and scarring, uses more hospital resources, and incurs a higher cost[8]. There are conflicting reports in the literature regarding the short and long term outcomes of these surgeries, as well as associated perioperative complications[8-10]. The goal of this systematic review is to summarize the functional outcomes, complications, and survivorship of TKA performed for the treatment of PTA.
This systematic review was conducted according to the PRISMA guidelines. A comprehensive search of PubMed, Cochrane Library, and SCOPUS was performed for prospective and retrospective studies examining the use of TKA for the treatment of PTA. The initial search utilized the following key terms: Knee arthroplasty, TKA and traumatic arthritis. English-language studies that examined the short and/or long-term outcomes of TKA performed for traumatic arthritis were included. References from retrieved studies were further reviewed to identify additional articles of interest.
First, inclusion and exclusion criteria were applied to study titles and abstracts independently by two reviewers (Saleh H, Yu S) to identify potentially eligible studies; disagreements were settled and final selections made by a third reviewer (Schwarzkopf R). Studies discussing TKA and traumatic arthritis were included. Studies which focused on unicompartmental knee arthroplasty, osteotomy, and/or patients with primary OA were excluded. Those studies considered potentially eligible were retrieved in full for review. Again, two reviewers independently applied inclusion and exclusion criteria. Studies examining fractures of the proximal tibia, patella, and/or distal femur were included. All study methods, including case-control, cohort, randomized-controlled studies- prospective or retrospective- were included. Case reports, case series, and biomechanics studies were excluded (Figure 1). Included studies were systematically reviewed for methodology (i.e., year of publication, sample size, study type, inclusion/exclusion criteria), demographics (i.e., age, gender), and clinical outcomes (i.e., follow-up period, preoperative diagnosis, implant selection criteria, pain, functional outcomes).
The main clinical outcomes studied regarding TKA following PTA included patient reported function, knee range of motion, and post-operative pain. Different studies utilized various criteria to assess these outcomes. Hospital for Special Surgery (HSS) Scores, International Knee Scores (IKS), Knee Osteoarthritis Outcomes Scores (KOOS), Oxford Knee Scores, and Knee Society Scores (KSS) were utilized by various studies to analyze the functional outcomes and pain following TKA. KSS was the most commonly utilized, however. The KSS is a 200-point scoring system which ascribes a maximum of 100 points each for function score (ability to walk, climb stairs, and need for assistive devices) and knee score (pain, range of motion, alignment, stability).
All studies examined complications following TKA for the treatment of PTA. The rate of complications was noted, as well as the specific complications observed. Six studies assessed the survivorship of TKA, with the endpoint defined as any subsequent surgery on the same knee. Studies followed patients for different averages of length of time, ranging from 3 to 15 years.
Sixteen articles met the inclusion criteria. Ten studies were retrospective, four were prospective (two with the same study cohort), and two were prospective matched cohorts. All studies examined patients with PTA due to fractures of the proximal tibia, patella, and/or distal femur, including nonunions or malunions in three studies. Four studies compared patients with TKA to those with primary OA. The average length of follow-up ranged from 3 to 15 years (Table 1).
| Ref. | Type of study | Total patients | Males (%) | Mean age | Fracture types | Mean follow-up time | Outcome criteria scoring |
| Abdel et al[14] | Prospective | 62 | 36 | 63 | Tibia | 15 | KSS |
| Bala et al[9] | Retrospective | PTA: 3509 | PTA: 43 | N/A | Tibia/femur | N/A | CCI; Elixhauser |
| Cont: 257, 611 | Cont: 35 | ||||||
| Benazzo et al[24] | Prospective | 43 | 47 | 64 | Tibia/femur/patella | 6 | KSS |
| Civinini et al[25] | Retrospective | 25 | 36 | 57 | Tibia | 8 | KSS |
| Deschamps et al[23] | Retrospective | 78 | 42 | 63 | Tibia/femur (includes malunions) | 4 | SOO |
| Lizaur-Utrilla et al[11] | Prospective matched cohort | PTA: 29 Cont: 58 | 35 | PTA: 57.3 Cont: 59.2 | Tibia | 7 | KSS, SF-12, WOMAC |
| Lonner et al[17] | Prospective | 30 | 50 | 60 | Tibia/femur | 4 | KSS |
| Lunebourg et al[8] | Retrospective | PTA: 33 | PTA: 55 | PTA: 69 | Tibia/femur | 11 | KSS, KOOS |
| Cont: 407 | Cont: 32 | Cont: 72 | |||||
| Massin et al[13] | Retrospective | 40 | 10 | 59 | Tibia/femur | 5 | IKS |
| Papadopoulos et al[22] | Retrospective | 47 | 21 | 65 | Femur (includes malunions) | 6 | KSS |
| Parratte et al[19] | Retrospective | 74 | 46 | 63 | Tibia/femur/patella (includes malunion) | 4 | KSS |
| Saleh et al[6] | Retrospective | 15 | 27 | 56 | Tibia | 6 | HSS, SF-36 |
| Scott et al[16] | Prospective matched cohort | PTA: 31 Cont: 93 | 26 | 66 | Tibia | 7 | Oxford knee, SF-12 |
| Shearer et al[10] | Retrospective | 47 | 62 | 48 | Tibia/femur | 4 | KSS |
| Weiss et al[12] | Prospective | 62 | 36 | 63 | Tibia | 5 | KSS |
| Wu et al[26] | Retrospective | 15 | 80 | 58 | Tibia/femur | 3 | KSS |
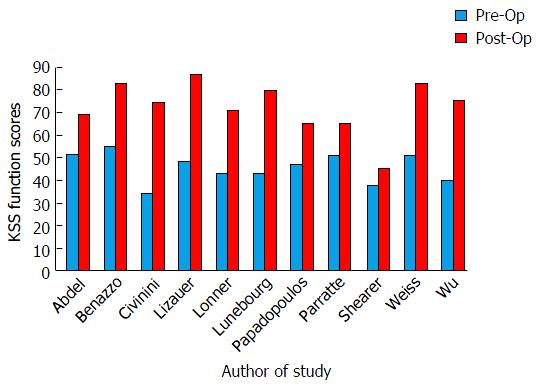
Fifteen studies assessed the functional outcomes of TKA for PTA, using different scoring systems such as HSS, IKS, KOOS and KSS. All eleven studies utilizing the KSS criterion showed trends towards or significant improvement between pre- and post- operative function scores (Figure 2). Lizaur-Utrilla et al[11] reported no difference in the post-operative functional scores of patients with PTA vs primary OA. Lunebourg et al[8], utilizing the KOOS criteria, reported significantly lower post-operative scores for patients with PTA, compared to primary OA, in all five categories - pain, symptoms, activities of daily living, sports activity, and quality of life.
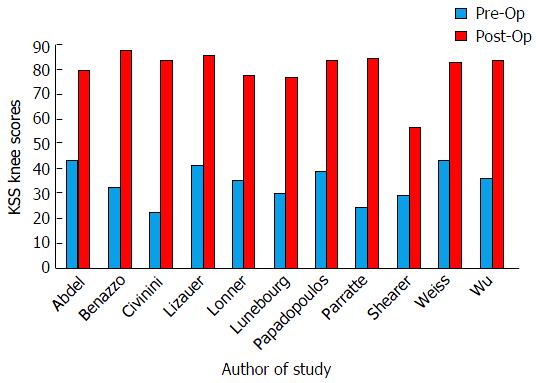
With regards to knee and pain scores, all studies utilizing the KSS criteria showed trends towards or significant improvement in pre- and post-operative scores (Figure 3). Lizaur-Utrilla et al[11] reported no significant difference in post-operative scores between patients with PTA vs primary OA. They also found no significant difference in WOMAC pain scores between the two groups[11]. Further, Weiss et al[12] examined patient-reported pain. Whereas all patients reported at least mild pain prior to the PTA, 83.9% denied having any pain after the surgery.
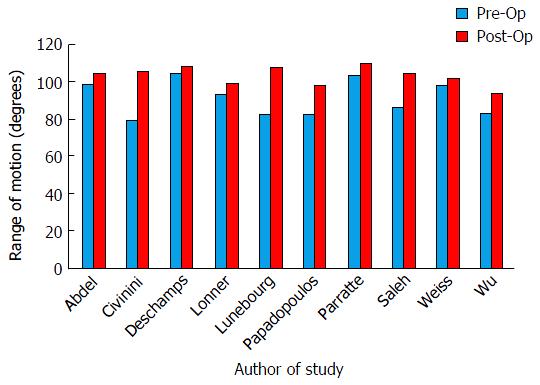
Ten studies examined the effect of TKA on the range of motion (ROM). All studies found an improvement in the mean arc of motion (Figure 4). Arthroplasty provided a substantial gain in flexion[13]. Some studies further compared the ROM between patients with PTA and primary OA. Lunebourg et al[8] observed that while the degree of improvement in ROM was greater in patients who underwent TKA for PTA, the final results were still significantly lower than those with primary OA. However, Lizaur-Utrilla et al[11] reported no significant difference in the final ROM of patients who underwent TKA for PTA vs primary OA.
Nine studies examined complications from TKA. The total complication rate at the time of longest follow-up ranged from 14% to 67%. Lizaur-Utrilla et al[11] reported that the complication rate was significantly higher in patients with PTA vs primary OA. The most commonly reported complications included superficial infections, deep infections, stiffness, manipulation under anesthesia (MUA), rupture of tendons, wound complications, osteolysis/polyethylene wear, instability, and aseptic loosening (Table 2). Bala et al[9] further reported that compared to patients with primary OA, patients with PTA had significantly higher complication rates of cellulitis, closed fractures, and wound complications. However, there was no difference between the groups in the rates of bleeding, broken prostheses, mechanical complications, MUA, osteolysis/polyethylene wear, or rupture of tendons[9]. In addition, nine studies analyzed the rate of revisions. This ranged from 3% to 18%.
| Ref. | Total | S Infxn | D Infxn | STIFF | MUA | ROT | WC | O/P | INST | AL | REVR |
| Abdel et al[14] | 34 | 3 | 5 | 10 | 1 | 1 | 5 | 8 | 3 | 6 | 18 |
| Bala et al[9] | 54 | 15 | 1 | 1 | 2 | 1 | 5 | 0 | 1 | 1 | 5 |
| Benazzo et al[24] | 21 | 1 | 2 | 5 | 1 | 1 | 1 | 1 | 1 | 2 | 7 |
| Civinini et al[25] | 32 | 4 | 4 | 8 | 1 | 4 | 4 | 1 | 1 | 4 | 1 |
| Deschamps et al[23] | 18 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 13 |
| Lizaur-Utrilla et al[11] | 14 | 3 | 1 | 1 | 3 | 3 | 3 | 1 | 1 | 3 | 3 |
| Lonner et al[17] | 57 | 1 | 10 | 1 | 1 | 3 | 6 | 1 | 1 | 1 | 1 |
| Lunebourg et al[8] | 21 | 1 | 6 | 6 | 1 | 1 | 1 | 1 | 1 | 3 | 9 |
| Massin et al[13] | 28 | 5 | 5 | 1 | 1 | 8 | 1 | 1 | 1 | 3 | 5 |
| Papadopoulous et al[22] | 19 | 1 | 6 | 1 | 1 | 2 | 4 | 1 | 2 | 1 | 13 |
| Parratte et al[19] | 26 | 3 | 3 | 8 | 1 | 4 | 1 | 1 | 1 | 1 | 1 |
| Saleh et al[6] | 67 | 1 | 15 | 1 | 20 | 1 | 1 | 7 | 7 | 1 | 1 |
| Scott et al[16] | 35 | 13 | 3 | 9 | 1 | 6 | 1 | 1 | 0 | 1 | 1 |
| Shearer et al[10] | 21 | 1 | 4 | 1 | 1 | 1 | 1 | 1 | 6 | 2 | 1 |
| Weiss et al[12] | 26 | 3 | 3 | 10 | 8 | 8 | 5 | 1 | 2 | 2 | 8 |
| Wu et al[26] | 47 | 13 | 1 | 1 | 27 | 13 | 1 | 1 | 7 | 1 | 1 |
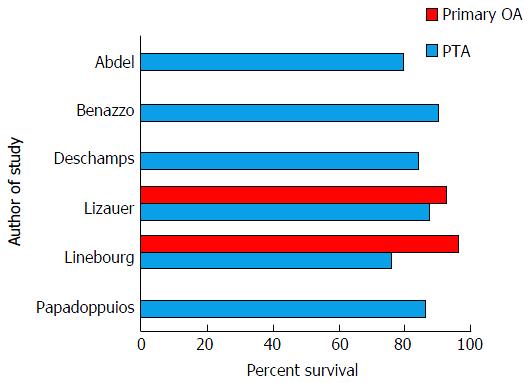
Six studies assessed the survivorship from any revision following TKA. Endpoints were defined as any surgery on the operated knee after the index TKA. Lizaur-Utrilla et al[11], after a mean follow-up of 7 years reported 90% survival, with no significant difference from those with primary OA. After a mean follow-up of 11 years, Lunebourg et al[8] reported a survivorship of 79%, significantly lower than patients with primary OA. Abdel et al[14], after a follow-up of 15 years, reported 82% survival (Figure 5).
There is a paucity in the literature regarding the outcome of TKA performed for the treatment of PTA. This systematic review aimed to examine the current English literature to investigate the clinical outcomes, perioperative complications, and survivorship of TKA for PTA.
Several studies utilized different scoring systems to judge the functional outcomes of TKA in PTA patients. Most of the studies utilized the KSS criteria, which is composed of a functional and knee score. The functional score includes a patient assessment of walking distance, ability to climb stairs, and need for assistive devices; the knee score incorporates patient reported pain, ROM, alignment, and stability[10]. The overwhelming majority of these studies reported an improvement in the functional and knee scores of patients following TKA for PTA. Lizaur-Utrilla et al[11] further reported that there were no significant differences in knee or WOMAC pain scores of patients treated with TKA for PTA vs primary OA. Lunebourg et al[8], while reporting significant improvement in scores, noted lower post-operative scores for patients with PTA vs primary OA.
These results indicate that TKA is an effective treatment for patients with PTA. It results in functional improvement, as well as increased range of motion and reduction in pain. With regards to the lower post-operative scores noted above, despite significant improvement, it is reasonable to infer that this difference compared to patients undergoing TKA for primary OA may be due to differences in the pre-operative status of the patients[8]. Thus, the post-operative difference observed in patients with PTA vs primary OA, is not due to the intrinsic success of the procedure itself, but rather the poorer pre-operative status of patients with PTA[8].
Six studies examined the survivorship of TKA with revision for any reason as an end point. Lizaur-Utrilla et al[11] found no significant difference in survivorship between patients with PTA vs primary OA, whereas Lunebourg did observe a difference[8]. Perhaps this disparity is due to differences in the lengths of follow-up. With increased length of follow-up, there seems to be a significant difference, in that TKA performed for PTA required more revisions and thus had decreased survivorship, compared to TKA performed for primary OA. Abdel et al[14] reported that the majority of the TKA revisions were for polyethylene wear. Given that patients with PTA tend to present at a younger age than primary OA, it is reasonable to at least partially attribute the decreased survivorship of TKA in patients with PTA to increased use and wear due to the younger age of this patient group[12]. Again, the difference in survivorship of TKA may be due to the patient population, and not the intrinsic success of the surgery. For example, Stiehl et al[15] reported higher risk-adjusted rates of failure in females and younger patients. Further long-term studies are needed to better characterize the factors that affect the survivorship of TKA for PTA.
All sixteen studies reported complications with TKA, including infection, stiffness, wound complications, intraoperative rupture of tendons, and osteolysis/ polyethylene wear. Scott et al[16] observed no significant difference in the overall rate of complications between patients who underwent TKA for PTA and primary OA. However, the type of complication differed between the two groups; wound complications and stiffness were observed more frequently in patients with TKA[16]. Abdel et al[14], even with the longest follow-up time of 15 years, reported that 90% of their complications occurred within the first two years of surgery. This data suggests that perioperative complications are more of a concern than long-term complications of TKA[14]. Despite the high rate of complications, most did not affect functional outcomes nor require further surgeries[11].
Many factors likely contribute to this observed rate of complications. First, patients with PTA have an inherent health challenge, in that PTA causes severe joint deformity as it is often accompanied by arthrofibrosis and malunion/nonunion of the fracture[9]. Second, patients with PTA often have had previous operations, which may compromise the soft-tissue surrounding the knee and thus predispose these patients to infections and wound complications[12]. Prior fracture surgeries are associated with increased infection rates after TKA[17]. Piedade et al[18] reported that prior knee surgery predisposes to higher post-operative complication rates in primary TKA. Third, scarring of the tissue, including fibrosis, may complicate exposure during surgery and positioning of the implant during surgery[12,19]. Malpositioning has been shown to have a negative effect on the long-term survival of TKA[20]. Efforts to preserve skin and soft-tissue vascularity, restore limb alignment, and ensure proper positioning may help prevent these complications[21,22]. Osteotomies may be utilized to correct rotational deformities of the knee[23]. Regardless, majority of studies reported improvement with total knee arthroplasty, with only few observed complications[24-26].
There are several limitations to this systematic review. First, there was inconsistency among studies regarding the criteria utilized to assess functional outcomes of TKA. However, this only slightly limited inter-study comparison, as majority of studies did utilize the KSS scoring systems. Second, tibial, patellar, and/or femoral fractures were examined in studies, but the results were grouped in this review. Third, there was a wide range in the average length of follow-up among the studies, from 3 to 15 years. However, this revealed not only short-term but also long-term outcomes. Despite these limitations, this review compiled the available research regarding the efficacy of TKA for the treatment of PTA.
In conclusion, despite the paucity in the literature regarding total knee arthroplasty in the treatment of post-traumatic arthritis, several conclusions may be drawn. TKA is an effective treatment for PTA, as it improves functional outcomes, range of motion, and pain. The accelerated nature of PTA and thus poorer pre-operative status of patients may explain the observed differences in the results of TKA following PTA vs primary OA. There is a significant rate of complications associated with this surgery, majority of which occur in the perioperative period. Scarring from the initial trauma and prior surgeries, as well as the inherent technical difficulty of the operation, likely contribute to this complication rate.
With a prevalence of 21%-44% reported in the literature, post-traumatic arthritis (PTA) of the knee occurs following intra- or extra-articular fractures of the proximal tibia, patella, and/or distal femur. After non-operative treatment is exhausted, total knee arthroplasty (TKA) is one of the surgical options. Compared to TKA performed for patients with primary osteoarthritis, TKA performed for PTA is often more technically challenging due to previous surgeries and scarring. There is a paucity in the literature regarding TKA for the treatment of PTA. The goal of this systematic review is to summarize the functional outcomes, complications, and survivorship of TKA performed for the treatment of PTA.
Several factors contribute to PTA following injury to the knee. These include mechanical imbalance, release of pro-inflammatory cytokines, and nonunions and malunions following fractures. TKA following PTA is often challenging, utilizes more hospital resources, and incurs higher costs.
The number of total knee arthroplasties performed in the United States has been increasing over the years. Newer implants have had great success, improving outcomes while decreasing the need for revisions. However, majority of these studies focus on patients with primary OA, not PTA.
PTA is prevalent in symptomatic arthritis, mainly in weight-bearing joints such as hips, knees and ankles. These patients have usually had prior surgeries and subsequent scarring, making total knee arthroplasties in this population technically more challenging. Understanding the functional outcomes and complications associated with total knee arthroplasties performed following PTA will help the orthopaedic surgeon in providing appropriate quality of care to this challenging subset of patients.
The manuscript is well written and interesting.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Anand A, Jiao C, Willis-Owen CA S- Editor: Gong XM L- Editor: A E- Editor: Li D
| 1. | Pickering RD. Posttraumatic arthritis. Can Fam Physician. 1984;30:1511-1513. [PubMed] |
| 2. | Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA. Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006;20:739-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 608] [Cited by in RCA: 682] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 3. | Larson AN, Hanssen AD, Cass JR. Does prior infection alter the outcome of TKA after tibial plateau fracture? Clin Orthop Relat Res. 2009;467:1793-1799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Furman BD, Mangiapani DS, Zeitler E, Bailey KN, Horne PH, Huebner JL, Kraus VB, Guilak F, Olson SA. Targeting pro-inflammatory cytokines following joint injury: acute intra-articular inhibition of interleukin-1 following knee injury prevents post-traumatic arthritis. Arthritis Res Ther. 2014;16:R134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 135] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 5. | Anderson DD, Marsh JL, Brown TD. The pathomechanical etiology of post-traumatic osteoarthritis following intraarticular fractures. Iowa Orthop J. 2011;31:1-20. [PubMed] |
| 6. | Saleh KJ, Sherman P, Katkin P, Windsor R, Haas S, Laskin R, Sculco T. Total knee arthroplasty after open reduction and internal fixation of fractures of the tibial plateau: a minimum five-year follow-up study. J Bone Joint Surg Am. 2001;83-A:1144-1148. [PubMed] |
| 7. | Schenker ML, Mauck RL, Ahn J, Mehta S. Pathogenesis and prevention of posttraumatic osteoarthritis after intra-articular fracture. J Am Acad Orthop Surg. 2014;22:20-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 96] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 8. | Lunebourg A, Parratte S, Gay A, Ollivier M, Garcia-Parra K, Argenson JN. Lower function, quality of life, and survival rate after total knee arthroplasty for posttraumatic arthritis than for primary arthritis. Acta Orthop. 2015;86:189-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Bala A, Penrose CT, Seyler TM, Mather RC, Wellman SS, Bolognesi MP. Outcomes after Total Knee Arthroplasty for post-traumatic arthritis. Knee. 2015;22:630-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Shearer DW, Chow V, Bozic KJ, Liu J, Ries MD. The predictors of outcome in total knee arthroplasty for post-traumatic arthritis. Knee. 2013;20:432-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Lizaur-Utrilla A, Collados-Maestre I, Miralles-Muñoz FA, Lopez-Prats FA. Total Knee Arthroplasty for Osteoarthritis Secondary to Fracture of the Tibial Plateau. A Prospective Matched Cohort Study. J Arthroplasty. 2015;30:1328-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 12. | Weiss NG, Parvizi J, Hanssen AD, Trousdale RT, Lewallen DG. Total knee arthroplasty in post-traumatic arthrosis of the knee. J Arthroplasty. 2003;18:23-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 70] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Massin P, Bonnin M, Paratte S, Vargas R, Piriou P, Deschamps G. Total knee replacement in post-traumatic arthritic knees with limitation of flexion. Orthop Traumatol Surg Res. 2011;97:28-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Abdel MP, von Roth P, Cross WW, Berry DJ, Trousdale RT, Lewallen DG. Total Knee Arthroplasty in Patients With a Prior Tibial Plateau Fracture: A Long-Term Report at 15 Years. J Arthroplasty. 2015;30:2170-2172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 15. | Stiehl JB, Hamelynck KJ, Voorhorst PE. International multi-centre survivorship analysis of mobile bearing total knee arthroplasty. Int Orthop. 2006;30:190-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Scott CE, Davidson E, MacDonald DJ, White TO, Keating JF. Total knee arthroplasty following tibial plateau fracture: a matched cohort study. Bone Joint J. 2015;97-B:532-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 71] [Article Influence: 7.1] [Reference Citation Analysis (1)] |
| 17. | Lonner JH, Pedlow FX, Siliski JM. Total knee arthroplasty for post-traumatic arthrosis. J Arthroplasty. 1999;14:969-975. [PubMed] |
| 18. | Piedade SR, Pinaroli A, Servien E, Neyret P. TKA outcomes after prior bone and soft tissue knee surgery. Knee Surg Sports Traumatol Arthrosc. 2013;21:2737-2743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Parratte S, Boyer P, Piriou P, Argenson JN, Deschamps G, Massin P. Total knee replacement following intra-articular malunion. Orthop Traumatol Surg Res. 2011;97:S118-S123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Suzuki G, Saito S, Ishii T, Motojima S, Tokuhashi Y, Ryu J. Previous fracture surgery is a major risk factor of infection after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:2040-2044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59:77-79. [PubMed] |
| 22. | Papadopoulos EC, Parvizi J, Lai CH, Lewallen DG. Total knee arthroplasty following prior distal femoral fracture. Knee. 2002;9:267-274. [PubMed] |
| 23. | Deschamps G, Khiami F, Catonné Y, Chol C, Bussière C, Massin P. Total knee arthroplasty for osteoarthritis secondary to extra-articular malunions. Orthop Traumatol Surg Res. 2010;96:849-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Benazzo F, Rossi SM, Ghiara M, Zanardi A, Perticarini L, Combi A. Total knee replacement in acute and chronic traumatic events. Injury. 2014;45 Suppl 6:S98-S104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Civinini R, Carulli C, Matassi F, Villano M, Innocenti M. Total knee arthroplasty after complex tibial plateau fractures. Chir Organi Mov. 2009;93:143-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Wu LD, Xiong Y, Yan SG, Yang QS. Total knee replacement for posttraumatic degenerative arthritis of the knee. Chin J Traumatol. 2005;8:195-199. [PubMed] |