Published online Sep 18, 2016. doi: 10.5312/wjo.v7.i9.553
Peer-review started: March 23, 2016
First decision: May 16, 2016
Revised: July 19, 2016
Accepted: July 29, 2016
Article in press: August 1, 2016
Published online: September 18, 2016
Processing time: 174 Days and 8.5 Hours
To compare the posterior vs anterior approaches for fusion of Lenke 5 adolescent idiopathic scoliosis curves, matched for curve magnitude and for the distal level of fixation (dLOF) standardized to the third lumbar vertebrae (L3).
A prospectively collected multicenter database was used for this retrospective comparative study. Our dependent variables included sagittal and coronal radiographic measurements, number of fused vertebrae, estimated blood loss, length of hospitalization and SRS total and individual domain scores at the two-year follow-up. Subject demographics were similar for all group comparisons. Independent t-test was used to compare groups for all analyses at P < 0.01.
For all matched cases of Lenke 5 curves, a selective approach was used only 50% of the time in cases undergoing a posterior fusion. When comparing a posterior selective approach to an anterior selective approach, surgeons utilizing a posterior approach fused significantly more levels than surgeons using an anterior approach with no other significant differences in radiographic or SRS outcomes (Ant = 4.8 ± 1.0 levels vs post = 6.1 ± 1.0 levels, P < 0.0001). When the dLOF was standardized to L3, the anterior approached provided significantly greater lumbar Cobb percent correction than the posterior approach (Ant = 69.1% ± 12.6% vs post = 54.6% ± 16.4%, P = 0.004), with no other significant radiographic or SRS score differences between approaches.
Surgeons treating Lenke 5c curves with a posterior instrumentation and fusion vs an anterior approach include more motion segments, even with a selective fusion. When controlled for the distal level of fixation, the anterior approach provides greater correction of the thoracolumbar curve.
Core tip: A multicenter database was analyzed to determine the frequency that surgeons performed a selective fusion of the thoracolumbar (TL)/lumbar curve in adolescent idiopathic scoliosis patients with Lenke 5c curves. We found that surgeons treating Lenke 5c curves will include more motion segments when employing a posterior approach. When controlled for the distal level of fixation, the anterior approach provides greater correction of the TL curve.
- Citation: Abel MF, Singla A, Feger MA, Sauer LD, Novicoff W. Surgical treatment of Lenke 5 adolescent idiopathic scoliosis: Comparison of anterior vs posterior approach. World J Orthop 2016; 7(9): 553-560
- URL: https://www.wjgnet.com/2218-5836/full/v7/i9/553.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i9.553
Lenke 5 curves are the third most common adolescent idiopathic scoliosis (AIS) curve type[1]. These curves are characterized by a single structural curve in lumbar/thoracolumbar region with non-structural curves (defined as bending to a Cobb angle of less than 25°) in thoracic and low lumbar (lumbosacral) regions of the spine. Common surgical treatment of Lenke 5c curves involves selective fusion (where the proximal level of fixation is distal to the thoracic apex) of the thoracolumbar curve[1] with the expectation that the non-structural thoracic curve will spontaneously correct[1-4]. There appears to be good literature support for selective fusion of thoracolumbar curves[2,4-6]. Ilgenfritz et al[4] studied 21 patients undergoing selective fusion of Lenke 5 curves and identified a spontaneous correction of the uninstrumented thoracic curves of 42% at 1 year. Thirty percent was the correction maintained at five years follow-up[4]. These authors and others felt that extension of fusion to include thoracic spine provided no significant advantages[7]. However, there appears to be a state of equipoise in the literature as to whether an anterior or posterior surgical approach is best suited for the selective fusion of Lenke 5 curves.
The anterior approach was initially popularized by Allen Dwyer et al[8] and became increasingly popular with advancements in anterior instrumentation[9-11]. The anterior thoracoabdominal approach was reported to be highly efficacious at improving clinical and radiographic measurements of trunk rotation[10,12]. One important potential advantage of anterior approach was the possibility that surgeons could obtain equal or better correction with shorter fusion constructs and consequently preserve more spinal motion[12-17].
The posterior approach, however, is more familiar to spine surgeons and the growing popularity of pedicle screws constructs for posterior spinal segmental instrumentation provided a very viable alternate to anterior approach[18]. Additionally, widespread use of osteotomies[3] has resulted in better coronal and axial correction[19-25]. Geck et al[23] compared Lenke 5 AIS correction in 31 patients with posterior pedicle screw instrumented fusion to an equal number of patients undergoing anterior instrumented fusion. The authors[23] reported significantly better curve correction, less loss of correction over time, and shorter hospital stays with the posterior approach. However, this data represented an AIS cohort that underwent an anterior instrumented fusion from a single institution in comparison to an AIS cohort that underwent a posterior pedicle screw instrumented fusion from a different institution, which makes it difficult to know if differences in blood loss, length of hospitalization, and magnitude of correction are due to differences in surgeon skill or management protocols. Bennett et al[20] reported maintenance of correction with posterior spinal fusion at five years follow-up for a heterogeneous group of Lenke 3c, 5c, and 6c curve types. However, these results cannot be generalized to Lenke 5 curves, as a systematic review by Helenius[26] suggests that the most appropriate use of the anterior approach is for Lenke 5 curves with a distal level of fixation (dLOF) at third lumbar vertebrae (L3). Evidence suggests that dLOF is significantly correlated with 2-year correction and balance after spinal fusion for Lenke 5 curves[27], however, previous studies have note matched anterior vs posterior cases by dLOF.
To effectively compare these two different approaches in regards to the magnitude of correction, the preservation of motion segments, and patient oriented outcomes for Lenke 5 AIS curves, data is required from multiple surgeons (multi-centered study) with careful regard to match cases according to curve magnitude while standardizing the dLOF at L3. Therefore, our purpose was to compare the posterior vs anterior approaches for the instrumentation and fusion of Lenke 5 AIS curve types for cases that were matched by curve magnitude, to compare cases where surgeons used a selective posterior approach (where the proximal level of fixation was distal to the thoracic apex) vs anterior cases and to compare selective posterior cases to anterior cases where the dLOF was standardized to the L3. We hypothesized that the anterior approach would result in fewer vertebrae fused and would provide better or comparable correction of radiographic curve parameters when the dLOF was standardized to L3.
A prospectively collected multicenter database was used for this cohort study and was queried for all surgically treated Lenke 5c patients. Institutional review board approval for the study was obtained locally from each contributing center and consent was obtained from each patient prior to data collection.
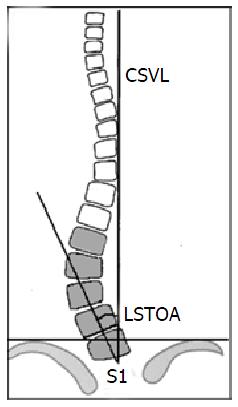
Radiographic and clinical measurements were recorded pre-operatively and at 2 years after surgery. Our dependent variables were thoracic and lumbar Cobb percent correction, lumbosacral take-off angle (LSTOA) (Figure 1), percent correction, absolute change in thoracolumbar (Th-L) apical translation, change in disc angulation below dLOF, change in proximal junctional kyphosis, change in kyphosis (from T5-T12 and from T10-L2), change in lumbar lordosis (T12 to top of the sacrum), number of fused vertebrae, estimated blood loss, length of hospitalization and SRS total and individual domain scores.
Patients with Lenke type 5c deformity were included in the analysis if their curve was corrected by either anterior or posterior spinal fusion. Eighty cases (40 anterior and 40 posterior) were identified and matched according to curve magnitude (Table 1). The surgical approach (anterior vs posterior), as well as the surgical levels fused, were decided by the operating surgeon.
| All cases | Selective fusions only | Selective fusions where dLOF = L3 | |||||||
| Mean (SD) | Mean (SD) | Mean (SD) | |||||||
| Ant (n = 40) | Post (n = 40) | P-value | Ant (n = 39) | Post (n = 20) | P-value | Ant (n = 25) | Post (n = 14) | P-value | |
| Thoracic Cobb | 28.7 (7.2) | 29.2 (8.0) | 0.759 | 28.3 (6.7) | 26.8 (5.7) | 0.395 | 27.6 (5.9) | 25.6 (5.5) | 0.313 |
| Lumbar Cobb | 46.9 (6.7) | 47.1 (6.6) | 0.880 | 46.8 (6.7) | 48.0 (6.8) | 0.0527 | 47.5 (7.1) | 46.6 (6.8) | 0.687 |
| LSTOA | 15.8 (4.7) | 17.0 (5.7) | 0.342 | 15.7 (4.8) | 18.3 (6.3) | 0.086 | 15.8 (4.8) | 16.3 (4.8) | 0.762 |
| Thoracolumbar apical translation (centimeters) | 5.0 (1.6) | 5.4 (1.5) | 0.241 | 5.0 (1.6) | 5.6 (1.7) | 0.214 | 5.2 (1.7) | 5.5 (1.3) | 0.521 |
| Disc angulation below dLOF (degrees) | 0.7 (6.2) | 1.9 (5.4) | 0.351 | 0.8 (6.2) | 2.3 (5.4) | 0.372 | 2.8 (6.3) | 0.4 (4.5) | 0.220 |
| Proximal junctional kyphosis (degrees) | 4.1 (5.7) | 4.7 (4.6) | 0.607 | 4.0 (5.8) | 3.2 (2.6) | 0.522 | 4.2 (6.4) | 3.2 (2.7) | 0.573 |
| Kyphosis from T5-T12 (degrees) | 25.7 (10.4) | 24.8 (10.0) | 0.719 | 25.7 (10.5) | 24.9 (10.2) | 0.756 | 24.4 (10.9) | 25.6 (11.1) | 0.743 |
| Kyphosis from T10-L2 (degrees) | 5.6 (11.3) | 3.8 (8.7) | 0.437 | 6.1 (11.0) | 7.5 (7.5) | 0.622 | 8.0 (11.7) | 5.9 (7.2) | 0.547 |
| Lordosis from T12-top of Sacrum (degrees) | 60.0 (12.2) | 57.4 (10.8) | 0.324 | 60.1 (12.3) | 55.7 (11.5) | 0.196 | 57.8 (12.9) | 58.9 (8.0) | 0.791 |
| SRS (total) | 3.9 (0.5) | 4.0 (0.3) | 0.463 | 3.9 (0.5) | 4.1 (0.3) | 0.371 | 3.9 (0.4) | 4.1 (0.3) | 0.305 |
| SRS (self) | 3.8 (0.7) | 3.7 (0.6) | 0.367 | 3.8 (0.7) | 3.5 (0.6) | 0.335 | 3.8 (0.5) | 3.5 (0.6) | 0.282 |
| SRS (pain) | 3.7 (0.7) | 3.9 (0.6) | 0.269 | 3.6 (0.7) | 4.0 (0.4) | 0.139 | 3.6 (0.6) | 4.0 (0.4) | 0.087 |
| SRS (function) | 4.0 (0.6) | 4.1 (0.4) | 0.469 | 4.1 (0.6) | 4.2 (0.5) | 0.392 | 4.2 (0.4) | 4.2 (0.5) | 0.691 |
| SRS (activity) | 4.5 (0.7) | 4.6 (0.5) | 0.576 | 4.5 (0.7) | 4.6 (0.6) | 0.572 | 4.5 (0.5) | 4.6 (0.6) | 0.496 |
To compare anterior vs posterior surgical approaches, three separate analyses were performed. The first analysis was to compare all matched cases of anterior vs posterior approaches (anterior n = 40, posterior n = 40). The second analysis compared cases where surgeons used a selective posterior approach (meaning the proximal point of fixation was below the apical vertebra of the thoracic cure) vs selective anterior approaches (anterior selective n = 39, posterior selective n = 20). The third analysis was to compare selective posterior cases to selective anterior cases where the dLOF was standardized to the L3 (anterior L3 n = 25, posterior L3 n = 14) (Figure 1).
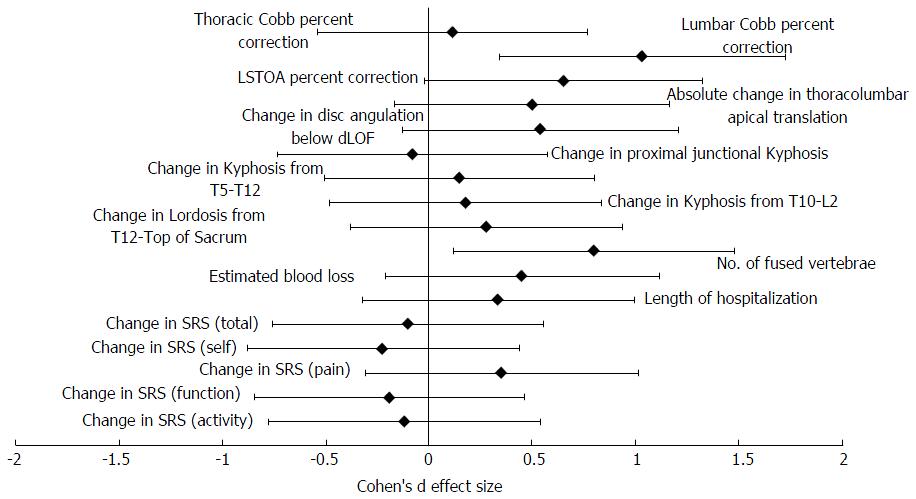
Independent t-tests were used to compare anterior and posterior cases for all outcome measures. Our alpha level was conservatively set a priori at 0.01 to control for multiple comparisons. Cohen’s d effect sizes and associated 95%CIs were calculated for our third analysis (dLOF = L3) to estimate the magnitude and precision of the group differences. Clinical interpretation of effect sizes was performed as > 0.80 was a large effect, 0.50 to 0.79 was a moderate effect, 0.20 to 0.49 was a small effect, and < 0.20 was a trivial effect. Data was analyzed using Statistical Package for Social Sciences (SPSS) Version 20.0 (SPSS, Inc, Chicago, IL).
The angulation of the low lumbar segments (L4 and L5) from the sacrum on the standing film was felt to be an important determinant of coronal plane balance[28]. Thus the LSTOA[29], defined from the standing spinal radiograph as the angle between the best-fit line between the spinous processes of L4, L5 and S1 and the vertical, was a radiographic measure developed to assess the influence of instrumentation and fusion on the coronal balance (Figure 2). Four raters of varying experience levels measured pre-operative and 2-year post-operative radiographs for 10 patients on two occasions. Pre-operative and post-operative measurements were separated by at least 24 h and raters were blinded to the first set of measurements during the second measurement occasion. All raters used the same software and all were blinded to one another’s measurements until data collection was complete. The reliability of the LSTOA measurement was considered “good” with an intraclass correlation coefficient of 0.829 and Cronbach’s alpha value of 0.975.
There were no differences in patient demographics for age, height, mass and sex distribution (Ant = 15.1 ± 2.0 years, 163.3 ± 9.6 cm, 56.9 ± 12.1 kg, 8M:32F vs post = 15.4 ± 2.0 years, 159.6 ± 20.2 cm, 59.5 ± 14.1 kg, 6M:34F, P > 0.01 for all analyses). There were no significant differences between anterior and posterior cohorts for all cases (anterior n = 40, posterior n = 40, P > 0.01 for all analyses), selective fusions (anterior selective n = 39, posterior selective n = 20, P > 0.01 for all analyses), or selective fusions where dLOF was standardized to L3 (anterior L3 n = 25, posterior L3 n = 14, P > 0.01 for all analyses, Table 1).
The anterior approach resulted in a significantly less number of fused vertebrae (Ant = 4.9 ± 1.1 vs post = 9.0 ± 3.3, P < 0.0001). At 2 years follow-up the radiographic correction, estimated blood loss, length of hospitalization and patient reported SRS scores were noted to be similar for both surgical approaches (P > 0.01 for all analyses) (Tables 2 and 3).
| All cases | Selective fusions only | Selective fusions where dLOF = L3 | |||||||
| Mean (SD) | Mean (SD) | Mean (SD) | |||||||
| Ant (n = 40) | Post (n = 40) | P-value | Ant (n = 39) | Post (n = 20) | P-value | Ant (n = 25) | Post (n = 14) | P-value | |
| Thoracic Cobb percent correction | 36.7 (23.2) | 48.1 (24.3) | 0.036 | 35.9 (22.9) | 35 (20.2) | 0.890 | 40.5 (24.6) | 37.9 (17.7) | 0.732 |
| Lumbar Cobb percent correction | 64.5 (14.7) | 63.4 (17.0) | 0.764 | 64.7 (14.9) | 58.2 (17.1) | 0.135 | 69.1 (12.6) | 54.6 (16.4) | 0.0041 |
| LSTOA percent correction | 46.6 (17.0) | 44.9 (21.6) | 0.688 | 46.9 (17.2) | 46.2 (21.7) | 0.900 | 48.8 (15.6) | 37.7 (19.4) | 0.058 |
| Absolute change in thoracolumbar apical translation (centimeters) | 3.6 (1.4) | 3.2 (1.6) | 0.293 | 3.6 (1.4) | 3.5 (1.7) | 0.669 | 3.9 (1.4) | 3.2 (1.4) | 0.157 |
| Change in disc angulation below dLOF (degrees) | 5.2 (9.5) | 5.8 (5.0) | 0.702 | 5.1 (9.6) | 6.0 (5.7) | 0.685 | 9.0 (7.9) | 5.1 (5.7) | 0.116 |
| Change in proximal junctional Kyphosis (degrees) | 3 (5.2) | 4.4 (6.1) | 0.253 | 2.7 (5.0) | 2.7 (3.8) | 0.989 | 2.7 (5.7) | 3.1 (3.7) | 0.806 |
| Change in Kyphosis from T5-T12 (degrees) | -2.4 (9.7) | 0.2 (10.3) | 0.253 | -2.3 (9.8) | -4.4 (8.4) | 0.424 | -3.5 (10.9) | -5.0 (8.2) | 0.652 |
| Change in Kyphosis from T10-L2 (degrees) | 24.2 (158.1) | 9.6 (8.2) | 0.562 | 25.1 (160.1) | 12.4 (8.0) | 0.725 | 39.8 (199.7) | 11.2 (8.0) | 0.597 |
| Change in Lordosis from T12-Top of sacrum (degrees) | 25.0 (148.6) | -1.8 (11.6) | 0.261 | 25.9 (150.5) | -6.0 (10.8) | 0.350 | 39.1 (187.9) | -3.3 (11.0) | 0.407 |
| No. of fused vertebrae | 4.9 (1.1) | 9.0 (3.3) | < 0.0011 | 4.8 (1.0) | 6.1 (1.0) | < 0.0011 | 5.1 (0.8) | 5.8 (1.0) | 0.025 |
| Estimated blood loss (mL) | 463 (327) | 985 (1046) | 0.0031 | 457 (329) | 396 (166) | 0.441 | 526 (381) | 380 (168) | 0.185 |
| Length of hospitalization (d) | 5.8 (1.5) | 6.0 (1.4) | 0.593 | 5.7 (1.4) | 5.8 (1.0) | 0.926 | 6.0 (1.2) | 5.6 (1.2) | 0.378 |
| All cases | Selective fusions only | Selective fusions where dLOF = L3 | |||||||
| Mean (SD) | Mean (SD) | Mean (SD) | |||||||
| Ant (n = 40) | Post (n = 40) | P-value | Ant (n = 39) | Post (n = 20) | P-value | Ant (n = 25) | Post (n = 14) | P-value | |
| Change in SRS (total) | 0.15 (0.54) | 0.12 (0.53) | 0.848 | 0.19 (0.52) | 0.21 (0.31) | 0.931 | 0.14 (0.44) | 0.18 (0.32) | 0.811 |
| Change in SRS (self) | -0.54 (0.87) | -0.25 (0.93) | 0.262 | -0.47 (0.83) | -0.14 (0.81) | 0.258 | -0.40 (0.37) | -0.27 (0.84) | 0.632 |
| Change in SRS (pain) | 0.49 (0.70) | 0.45 (0.83) | 0.860 | 0.55 (0.66) | 0.38 (0.56) | 0.456 | 0.48 (0.71) | 0.25 (0.53) | 0.399 |
| Change in SRS (function) | 0.12 (0.66) | -0.09 (0.65) | 0.259 | 0.11 (0.67) | 0.05 (0.37) | 0.747 | -0.03 (0.50) | 0.06 (0.42) | 0.653 |
| Change in SRS (activity) | 0.14 (0.50) | 0.06 (0.58) | 0.640 | 0.14 (0.51) | 0.17 (0.61) | 0.904 | 0.14 (0.56) | 0.21 (0.64) | 0.774 |
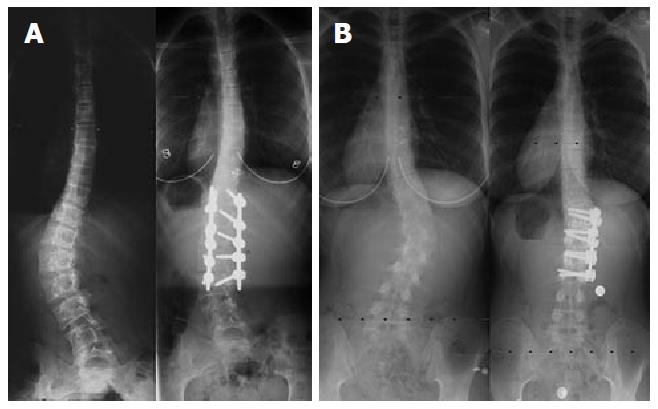
There were significantly fewer vertebrae included in the fusion construct when surgeons utilized an anterior approach (Ant = 4.8 ± 1.0 vs post = 6.1 ± 1.0, P < 0.0001). No significant differences were noted between anterior and posterior approaches for measures of radiographic curve parameters, estimated blood loss, length of hospitalization, or SRS scores (P > 0.01 for all analyses) (Tables 2 and 3). Representative examples for selective anterior and posterior approaches are presented in Figure 1.
The anterior approach resulted in a significantly greater lumbar Cobb percent correction (Ant = 69.1% ± 12.6% vs post 54.6% ± 16.4%, P = 0.004). No significant differences were noted between anterior and posterior approaches for number of fused vertebrae, radiographic curve parameters, estimated blood loss, length of hospitalization, or SRS scores (P > 0.01 for all analyses) (Tables 2 and 3). We identified large effect sizes in favor of the anterior approach for number of fused vertebrae and lumbar Cobb percent correction. We also identified moderate effect sizes in favor of the anterior approach for LSTOA percent correction, absolute change in Th-L apical translation, and change in disc angulation below the dLOF (L3). All other effect sizes were trivial or small with 95% confidence intervals that were centered around zero, suggesting no meaningful treatment effects for those outcome measures (Figure 3).
A primary goal of spinal fusion for idiopathic scoliosis is to maximize correction, while preserving as many motion segments as possible[4]. Lenke 5 curves are unique in having a thoracolumbar or lumbar curve as the dominant curve in association with a flexible, non-structural thoracic curve, which is expected to spontaneously correct with a selective fusion. We have now provided evidence that for matched Lenke 5 cases and for cases where a selective fusion is performed with similar baseline curve parameters, surgeons performing a posterior approach will include more motion segments in the fusion construct when compared to those performing an anterior approach. In our analyses, including more motion segments did not improve radiographic or patient oriented outcomes[30]. These findings are particularly important in the context of current evidence highlighting significant reductions in sagittal, coronal, and transverse planes of motion following instrumented spinal fusion[31]. Furthermore, their results suggest that the more distal the fusion construct goes, the greater reductions in forward flexion post-operatively[31,32], which underscores the importance of standardizing to the dLOF. Surgeons should continue to rigorously evaluate surgical approaches in clearly defined cohorts to elucidate potential options for maximizing curve correction while maintaining spinal mobility. To our knowledge, this is the first study to compare selective instrumentation and fusion of matched Lenke 5c curves using either a posterior approach vs an anterior approach with the dLOF standardized (as recommended)[26] to the third lumbar level.
In our first analysis, we found that surgeons using a posterior approach to the Lenke 5c deformity included more levels in the instrumentation for comparable curves. This is not a surprising finding given that extension of the posterior exposure and instrumentation is technically easier since the anterior extension requires retraction of the lung, incision of the parietal pleura and control of the segmental vessels proximally or control and mobilization of iliac vessels distally. It should be acknowledged, however, that the relative benefit of complete correction of deformity vs the functional loss from fusing more segments has not been fully elucidated. The tendency to fuse more vertebrae with the posterior approach was also demonstrated in our second analysis of selective posterior vs selective anterior cases, yet there was no evidence of superior correction with the posterior approach. Interestingly, half (20 of 40 cases) of our original matched posterior cases were not selective spinal fusions, whereas only 1 of the matched anterior cases had a fusion construct that encompassed the thoracic apex. This finding further illustrates the likelihood of surgeons utilizing a posterior approach to include proximal segments that may or may not be required to improve spinal alignment of the thoracic spine. However, we did identify that surgeons that elected to use a selective posterior fusion fused 5-6 fewer levels than those that utilized a non-selective posterior approach. Finally, when the dLOF was standardized in both groups to L3, the anterior approach provides about a 15% greater correction of the lumbar curve. We also identified moderate to large effect sizes in favor of the anterior approach for outcome measures including number of fused vertebrae, lumbar Cobb percent correction, LSTOA percent correction, absolute change in Th-L apical translation, and change in disc angulation below the dLOF (L3). While the clinical importance of differences of this magnitude is not clearly documented, our results illustrate the potential to maximize post-operative spinal motion with equal or greater radiographic correction with an anterior spinal fusion.
Historically, the anterior approach was considered the preferred approach because of its ability to provide excellent coronal curve correction with significant spine derotation and shorter fusion constructs[5-9]. Tao et al[14] reported superiority of anterior solid rod-screw instrumentation with shorter fusion segments, better sagittal alignment and quality of life measures (SRS scores) than posterior pedicle screw instrumentation. However, trunk scarring, spine pseudoarthrosis, negative impacts on pulmonary function and reduction of lumbar lordosis were reported to be major disadvantages of the anterior approach[24]. More recent studies with newer techniques and implant designs have reported no significant post-operative kyphosis[12] or pulmonary function changes[33] with the anterior thoracoabdominal approach. Our results are consistent with the recent studies in that there were no differences in patient oriented outcomes as reported on the SRS questionnaires or in EBL or length of hospitalization between anterior or posterior approaches for any of our three analyses.
This study has several limitations. Matching was based on radiographic measures but surgeons may have chosen the surgical approach based on the clinical appearance, extending the fusion to include the thoracic vertebra in cases with a more pronounce right scapular prominence. The sagittal plane alignment of either the lumbar and thoracic curves can also influence the decision on the surgical approach. For instance, increased lumbar kyphosis, excessive thoracic kyphosis or thoracic hyper-lordosis, may prompt the surgeon to use a posterior approach for instrumentation to affect sagittal plane correction and this was not analyzed. An argument could also be made that the magnitude of difference between these two approaches is not meaningful to the patient, as we did not identify significant differences in our SRS outcomes or length of hospitalization between approaches. The relative benefits of complete correction of deformity vs the functional lose from fusing more segments has not been objectively studied. However, until we have more objective data on the functional implications of longer fusions or the rate of adjacent level degeneration, we cannot strongly advise an anterior TL approach for the Lenke 5C curve. Given the above considerations, our results do suggest that an anterior approach may be advantageous for severe or rigid deformity where the desired dLOF is the third lumbar level (Figure 1), as it can provide better correction for same levels of fusion with no deleterious effects on patient reported outcomes.
In conclusion, surgeons treating Lenke 5c curves will include more motion segments when employing a posterior approach; when controlled for the dLOF, the anterior approach provides greater correction of the TL curve.
Lenke 5 scoliosis can be surgically corrected by either anterior or posterior approach. The purpose of this study purpose was to compare the posterior vs anterior approaches for fusion of Lenke 5 adolescent idiopathic scoliosis curves.
Posterior approach is more popular nowadays because of its ease and universal application. Anterior approach is generating interest again because of its ability to provide excellent coronal curve correction and significant spine derotation with relatively shorter fusion constructs. The current research is also focused on saving fusion levels, which may prove to be an important factor in the long term.
To our knowledge, this is the first study to compare selective instrumentation and fusion of matched Lenke 5c curves with the distal level of fixation (dLOF) standardized to the third lumbar level, in addition to overall surgical outcome of anterior vs posterior approaches.
This study suggests a tendency to fuse more levels with posterior approach for treating Lenke 5c curves and that the anterior approach provides greater correction for similar distal level of fusion. These findings may provide important guidelines with regards to surgical approach if surgeon prefers shorter fusion levels for deformity correction.
Distal level of fixation - dLOF.
Interesting paper that compares two different approaches for surgical correction of Lenke 5c scolisois by selective fusion.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Elgafy H, Korovessis P S- Editor: Qiu S L- Editor: A E- Editor: Li D
| 1. | Lenke LG, Betz RR, Clements D, Merola A, Haher T, Lowe T, Newton P, Bridwell KH, Blanke K. Curve prevalence of a new classification of operative adolescent idiopathic scoliosis: does classification correlate with treatment? Spine (Phila Pa 1976). 2002;27:604-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 128] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Senkoylu A, Luk KD, Wong YW, Cheung KM. Prognosis of spontaneous thoracic curve correction after the selective anterior fusion of thoracolumbar/lumbar (Lenke 5C) curves in idiopathic scoliosis. Spine J. 2014;14:1117-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Huitema GC, Jansen RC, van Ooij A, Punt IM, van Rhijn LW. Predictability of spontaneous thoracic curve correction after anterior thoracolumbar correction and fusion in adolescent idiopathic scoliosis. A retrospective study on a consecutive series of 29 patients with a minimum follow-up of 2 years. Spine J. 2015;15:966-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Ilgenfritz RM, Yaszay B, Bastrom TP, Newton PO. Lenke 1C and 5C spinal deformities fused selectively: 5-year outcomes of the uninstrumented compensatory curves. Spine (Phila Pa 1976). 2013;38:650-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Huitema GC, Jansen RC, Dompeling E, Willems P, Punt I, van Rhijn LW. Pulmonary function after less invasive anterior instrumentation and fusion for idiopathic thoracic scoliosis. Scoliosis. 2013;8:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Min K, Hahn F, Ziebarth K. Short anterior correction of the thoracolumbar/lumbar curve in King 1 idiopathic scoliosis: the behaviour of the instrumented and non-instrumented curves and the trunk balance. Eur Spine J. 2007;16:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Lark RK, Yaszay B, Bastrom TP, Newton PO. Adding thoracic fusion levels in Lenke 5 curves: risks and benefits. Spine (Phila Pa 1976). 2013;38:195-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Dwyer AF, Newton NC, Sherwood AA. An anterior approach to scoliosis. A preliminary report. Clin Orthop Relat Res. 1969;62:192-202. [PubMed] |
| 9. | Halm H, Richter A, Thomsen B, Köszegvary M, Ahrens M, Quante M. [Anterior scoliosis surgery. State of the art and a comparison with posterior techniques]. Orthopade. 2009;38:131-134, 136-140, 142-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Kaneda K, Shono Y, Satoh S, Abumi K. New anterior instrumentation for the management of thoracolumbar and lumbar scoliosis. Application of the Kaneda two-rod system. Spine (Phila Pa 1976). 1996;21:1250-1261; discussion 1261-1262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 122] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Hall JE. Dwyer Instrumentation in anterior fusion of the spine. J Bone Joint Surg Am. 1981;63:1188-1190. [PubMed] |
| 12. | Verma K, Auerbach JD, Kean KE, Chamas F, Vorsanger M, Lonner BS. Anterior spinal fusion for thoracolumbar scoliosis: comprehensive assessment of radiographic, clinical, and pulmonary outcomes on 2-years follow-up. J Pediatr Orthop. 2010;30:664-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Wang T, Zeng B, Xu J, Chen H, Zhang T, Zhou W, Kong W, Fu Y. Radiographic evaluation of selective anterior thoracolumbar or lumbar fusion for adolescent idiopathic scoliosis. Eur Spine J. 2008;17:1012-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Tao F, Wang Z, Li M, Pan F, Shi Z, Zhang Y, Wu Y, Xie Y. A comparison of anterior and posterior instrumentation for restoring and retaining sagittal balance in patients with idiopathic adolescent scoliosis. J Spinal Disord Tech. 2012;25:303-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Lu WC, Zhang JG, Qiu GX, Sadik I, Wang YP, Yu B, Zhao H, Zhao Y, Weng XS. [Selective anterior thoracolumbar or lumbar fusion for adolescent idiopathic scoliosis]. Zhonghua Waike Zazhi. 2009;47:758-761. [PubMed] |
| 16. | Liu Y, Li M, Zhu XD, Zhou XH, Chen HJ, Wang XW, Shi P, Yuan W. Retrospective analysis of anterior correction and fusion for adolescent idiopathic thoracolumbar/lumbar scoliosis: the relationship between preserving mobile segments and trunk balance. Int Orthop. 2009;33:191-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Lowe TG, Betz R, Lenke L, Clements D, Harms J, Newton P, Haher T, Merola A, Wenger D. Anterior single-rod instrumentation of the thoracic and lumbar spine: saving levels. Spine (Phila Pa 1976). 2003;28:S208-S216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke Type I adolescent idiopathic scoliosis curves. Spine (Phila Pa 1976). 2005;30:1859-1866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 109] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 19. | Gu SX, Li M, Zhu XD, Wang CF, Wu DJ, Zhao YC. Posterior pedicle screws combined with shortening and release techniques for lumbar and thoracolumbar adolescent idiopathic scoliosis. Orthop Surg. 2009;1:6-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Bennett JT, Hoashi JS, Ames RJ, Kimball JS, Pahys JM, Samdani AF. The posterior pedicle screw construct: 5-year results for thoracolumbar and lumbar curves. J Neurosurg Spine. 2013;19:658-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Huang Z, Wang Q, Yang J, Yang J, Li F. Vertebral Derotation by Vertebral Column Manipulator Improves Postoperative Radiographs Outcomes of Lenke 5C Patients for Follow-up of Minimum 2 Years. Clin Spine Surg. 2016;29:E157-E161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Hwang SW, Dubaz OM, Ames R, Rothkrug A, Kimball JS, Samdani AF. The impact of direct vertebral body derotation on the lumbar prominence in Lenke Type 5C curves. J Neurosurg Spine. 2012;17:308-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Geck MJ, Rinella A, Hawthorne D, Macagno A, Koester L, Sides B, Bridwell K, Lenke L, Shufflebarger H. Comparison of surgical treatment in Lenke 5C adolescent idiopathic scoliosis: anterior dual rod versus posterior pedicle fixation surgery: a comparison of two practices. Spine (Phila Pa 1976). 2009;34:1942-1951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 86] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 24. | Shufflebarger HL, Geck MJ, Clark CE. The posterior approach for lumbar and thoracolumbar adolescent idiopathic scoliosis: posterior shortening and pedicle screws. Spine (Phila Pa 1976). 2004;29:269-276; discussion 276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 108] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 25. | Okada E, Watanabe K, Pang L, Ogura Y, Takahashi Y, Hosogane N, Toyama Y, Matsumoto M. Posterior correction and fusion surgery using pedicle-screw constructs for Lenke type 5C adolescent idiopathic scoliosis: a preliminary report. Spine (Phila Pa 1976). 2015;40:25-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 26. | Helenius I. Anterior surgery for adolescent idiopathic scoliosis. J Child Orthop. 2013;7:63-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Wang Y, Bünger CE, Zhang Y, Wu C, Li H, Dahl B, Hansen ES. Lowest instrumented vertebra selection for Lenke 5C scoliosis: a minimum 2-year radiographical follow-up. Spine (Phila Pa 1976). 2013;38:E894-E900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 28. | Mehta SS, Modi HN, Srinivasalu S, Chen T, Suh SW, Yang JH, Song HR. Interobserver and intraobserver reliability of Cobb angle measurement: endplate versus pedicle as bony landmarks for measurement: a statistical analysis. J Pediatr Orthop. 2009;29:749-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Abel MF, Herndon SK, Sauer LD, Novicoff WM, Smith JS, Shaffrey CI. Selective versus nonselective fusion for idiopathic scoliosis: does lumbosacral takeoff angle change? Spine (Phila Pa 1976). 2011;36:1103-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 30. | Singla A, Bennett JT, Sponseller PD, Pahys JM, Marks MC, Lonner BS, Newton PO, Miyanji F, Betz RR, Cahill PJ. Results of selective thoracic versus nonselective fusion in Lenke type 3 curves. Spine (Phila Pa 1976). 2014;39:2034-2041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 31. | Udoekwere UI, Krzak JJ, Graf A, Hassani S, Tarima S, Riordan M, Sturm PF, Hammerberg KW, Gupta P, Anissipour AK. Effect of Lowest Instrumented Vertebra on Trunk Mobility in Patients With Adolescent Idiopathic Scoliosis Undergoing a Posterior Spinal Fusion. Spine Deformity. 2014;2:291-300. [RCA] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Sun X, Qiu Y, Liu Z, Ma WW, Wang B, Zhu ZZ, Yu Y, Qian BP, Zhu F. Interbody cage support improves reconstruction of sagittal balance after anterior selective fusion in Lenke type 5 idiopathic scoliosis patients. Orthop Surg. 2009;1:285-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Kim YJ, Lenke LG, Bridwell KH, Cheh G, Sides B, Whorton J. Prospective pulmonary function comparison of anterior spinal fusion in adolescent idiopathic scoliosis: thoracotomy versus thoracoabdominal approach. Spine (Phila Pa 1976). 2008;33:1055-1060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |