Published online Jul 18, 2016. doi: 10.5312/wjo.v7.i7.458
Peer-review started: January 22, 2016
First decision: March 24, 2016
Revised: April 4, 2016
Accepted: May 31, 2016
Article in press: June 2, 2016
Published online: July 18, 2016
Processing time: 172 Days and 2.7 Hours
We describe a case of a 19-year-old young man with oligoarthritis type of juvenile idiopathic arthritis, who presented with several month duration of lower neck pain and progressive muscular weakness of all four limbs. X-rays of the cervical spine demonstrated spontaneous apophyseal joint fusion from the occipital condyle to C6 and from C7 to Th2 with marked instability between C6 and C7. Surgical intervention began with anterolateral approach to the cervical spine performing decompression, insertion of cage and anterior vertebral plate and screws, followed by posterior approach and fixation. Care was taken to restore sagittal balance. The condition was successfully operatively managed with multisegmental, both column fixation and fusion, resulting in pain cessation and resolution of myelopathy. Postoperatively, minor swallowing difficulties were noted, which ceased after three days. Patient was able to move around in a wheelchair on the sixth postoperative day. Stiff neck collar was advised for three months postoperatively with neck pain slowly decreasing in the course of first postoperative month. On the follow-up visit six months after the surgery patient exhibited no signs of spastic tetraparesis, X-rays of the cervical spine revealed solid bony fusion at single mobile segment C6-C7. He was able to gaze horizontally while sitting in a wheelchair. Signs of myelopathy with stiff neck and single movable segment raised concerns about intubation, but were successfully managed using awake fiber-optic intubation. Avoidance of tracheostomy enabled us to perform an anterolateral approach without increasing the risk of wound infection. Regarding surgical procedure, the same principles are obeyed as in management of fracture in ankylosing spondylitis or Mb. Forestrier.
Core tip: The spontaneous cervical apophyseal joint fusion is rare and only seen in juvenile type rheumatoid arthritis, where spontaneous fusions of more than three cervical segments are extremely uncommon. We present a patient with fusion of all but C6-C7 level. The single mobile segment became highly unstable, producing mechanical pain with symptoms of myelopathy. Prior to the surgery, awake fiber-optic intubation was used. Surgical intervention began with the anterolateral approach to the cervical spine performing decompression, insertion of cage and anterior vertebral plate and screws, followed by posterior approach and fixation. Care was taken to restore sagittal balance.
- Citation: Suhodolčan L, Mihelak M, Brecelj J, Vengust R. Operative stabilization of the remaining mobile segment in ankylosed cervical spine in systemic onset - juvenile idiopathic arthritis: A case report. World J Orthop 2016; 7(7): 458-462
- URL: https://www.wjgnet.com/2218-5836/full/v7/i7/458.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i7.458
Juvenile idiopathic arthritis (JIA) is an exclusion diagnosis that applies to any arthritis of unknown origin, persisting for more than 6 wk and with the onset before the age of 16 years[1]. Patients who belong to oligoarthritis type of JIA are characterized by an asymmetric arthritis affecting mainly large joints of an early onset (before 6 years of age), a female predilection, a high frequency of positive antinuclear antibodies, a high risk for developing chronic iridocyclitis and consistent HLA associations, which is typical of children and is not seen in adults[2,3].
Recent advances in medical treatment enable more favorable prognosis, but rapid progressing cases may result in severe complications such as joint deformities, joint ankylosis, osteoporosis and decreased bone mass. The common clinical manifestation of spinal involvement is the instability of upper cervical spine. The spontaneous cervical apophyseal joint fusion is rare and only seen in juvenile type rheumatoid arthritis, where one-or two level fusions occur in up to 41 percents of cases[4]. On the other hand, spontaneous fusions of more than three cervical segments are reported to be extremely rare (Table 1)[5].
| Patient characteristics |
| 27-yr-old female |
| JIA for 10 yr |
| Symptoms |
| Posterior neck pain |
| Progressive weakness |
| Paresthesia and dysesthesia below the C7 dermatome |
| Imaging |
| Spontaneus apophyseal joint fusion from the occipital condyle to C6 |
| Instability at C6/C7 level - only mobile segment |
| Problems during procedure |
| Contracture of temporo-mandibular joint |
| Endotracheal intubation not feasible due to stiff neck |
| Tracheostomy needed |
| Severe osteoporosis noted |
| Approach/type of fixation |
| Posterior approach |
| Decompressive subtotal laminectomy |
| Interspinous process wiring with titanium-braded cable and addition of integrated bone graft at C6/7 level |
| Results |
| Pathologic reflexes disappeared |
| Well established bone graft incorporation 6 mo post-op |
| Conclusion |
| First-reported case of long-segment cervical fusion, may be related with rapid progression of the disease |
We report a case of spontaneous cervical ankylosis from the occiput to C6 and from C7 to Th2 with subjacent instability at C6-C7 level and neurological deficit in patient with JIA, which has been operatively stabilized.
A 19-year-old young man with oligoarthritis type of JIA presented with several month duration of lower neck pain and progressive muscular weakness of all four limbs. He had been treated previously for major contractures of the hip, knee and ankles. The valgus of the both knees was corrected with a temporary hemiepiphysiodesis at the age of 12. At the age of 15 an elongation of Achilles tendon and the knee flexors were performed. Total hip replacement was performed at the age of 15 on the left side and a year later on the right side. He has been partly wheelchair-bound for 3 years before admission due to extensive contractures of hips, knees and ankles. But he was able to walk short distances with the help of crutches. At the age of 12, pain in the cervical spine occurred for the first time, followed by occasional mild pain episodes. The patient had been treated with methotrexate, steroids and antihypertensive therapy.
Clinical examination revealed markedly limited mobility of cervical spine with rotations being completely blocked. Flexion and extension resulted in significant pain in lower cervical spine. Patient was unable to walk independently, with signs of spastic tetraparesis.
Loss of lordosis and sclerotic changes of the facet joints in cervical plain X-rays had been present 7 years before admission (Figure 1). X-rays of the cervical spine on the day of the admission demonstrated spontaneous apophyseal joint fusion from the occipital condyle to C6 and from C7 to Th2. Bending films showed marked instability between C6 and C7 (Figure 2). There were no rentgenographic abnormalities of thoracolumbar spine. Computerized tomography/angiography confirmed apophyseal fusion of the entire cervical spine except for the C6-C7 level, where the left vertebral artery was dominant. Spinal canal was narrowed at C6-C7 due to posteriorly protruding spondylophites. MRI revealed C6-C7 disc degeneration with spinal canal stenosis but no signal changes in spinal cord.
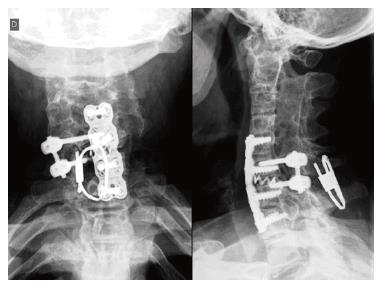
The patient underwent surgical intervention because of progredient spastic tetraparesis. Surgery was started after awake fiberoptic intubation. We began the procedure using anterolateral approach to the spine, where discectomy and osteophyte removal was performed, followed by the insertion of cage filled with bone substitute at the C6-C7 level. Vertebral bodies C5, C6 were fixed to C7, Th1 using anterior vertebral plate and screws (Figure 3).
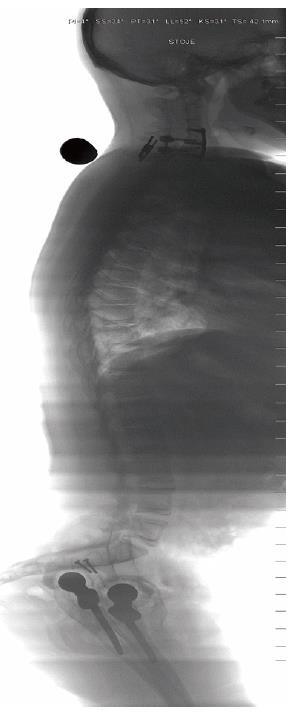
Later on, the patient was turned prone, and cervical spine was accessed using the posterior approach. Posterior fixation was obtained using unilateral pedicular screws combined with an interspinous wire. Pedicular screws were inserted on the right side only, due to very small caliber vertebral artery ipsilaterally. Bone substitute was placed to the decorticated C6-C7 apophyseal joints. Care was taken to fix the spine in a position, which would enable the patient to gaze horizontally in a sitting position (Figure 4).
After the surgery patient had mild swallowing difficulties, which ceased after three days. He was able to move around in a wheelchair on the sixth postoperative day. Stiff neck collar was advised for three months postoperatively with neck pain slowly decreasing in the course of the first postoperative month. On the follow-up visit six months after the surgery the patient exhibited no signs of myelopathy, X-rays of the cervical spine revealed solid bony fusion at C6-C7 level. He was able to gaze horizontally while sitting in a wheelchair.
JIA of the spine was once believed to be a benign disease process. Many studies have shown, however, that the spectrum of joint erosion, deformity, ensuing neurological deficit, and underlying pathologic mechanisms warrant concern, especially in cervical spine[6-8]. The most common pathologic condition is a spontaneous posterior cervical fusion seen in the late stage of the disease. Fusion usually occurs in one or two segments without clinical consequences[5]. Apart from this, our patient presented with fusion of all but one level of cervical spine. The single mobile segment became highly unstable over time and produced mechanical pain, which along with symptoms of myelopathy forced the patient to consult a physician. The clinical course of progressive stiffness with escalating localized pain is unique in childhood and only resembles the pseudoarthrosis in ankylosing spondylitis in adults[9,10].
Regarding surgical procedure the same principles were obeyed as in management of fracture in ankylosing spondylitis or Mb. Forestier[11,12]. Multilevel both column fixation was performed employing combined anterolateral and posterior approach. Signs of myelopathy with stiff neck and single movable segment raised concerns about intubation, but were successfully managed using awake fiber-optic intubation. Avoidance of tracheostomy enabled us to perform the anterolateral approach without increasing the risk of wound infection.
To the best of our knowledge, this is the first-reported case of multisegmental cervical ankylosis in JIA, operatively managed with combined anterior and posterior spinal interbody fusion.
As with other cases of stiff cervical spine, special care has to be taken to achieve proper sagittal alignment[13]. With careful preoperative planning fixation should be achieved, which suits patient best in terms of optimal gaze.
We present a JIA patient with a multisegmental spontaneous fusion of cervical spine. The one segment remaining mobile became overtly instable causing mechanical neck pain and progressive spastic tetraparesis. The condition was operatively managed with multisegmental, both column fixation and fusion, resulting in pain cessation and resolution of myelopathy symptoms six months postoperatively.
A 19-year-old young man with oligoarthritis type of juvenile idiopathic arthritis presented with several month duration of lower neck pain and progressive muscular weakness of all four limbs.
Clinical examination revealed markedly limited mobility of cervical spine with rotations being completely blocked. Flexion and extension resulted in significant pain in lower cervical spine. Patient was unable to walk independently, with signs of spastic tetraparesis.
Ankylosing spondylitis, Mb. Forestier, Diffuse idiopathic skeletal hyperostosis.
All labs were within normal limits.
X-rays of the cervical spine on the day of the admission demonstrated spontaneous apophyseal joint fusion from the occipital condyle to C6 and from C7 to Th2. Flexion and extension X-rays showed wide apophyseal joint space between C6 and C7, suggesting instability and excessive mobility. Computerized tomography confirmed ankylosis at the C0-C1 level.
Juvenile idiopathic arthritis.
Surgical intervention with the anterolateral approach to the cervical spine, performing decompression, insertion of cage and anterior vertebral plate and screws, followed by posterior approach and fixation.
Rapid progressing cases of juvenile idiopathic arthritis may result in severe complications such as joint deformities, joint ankylosis, osteoporosis and decreased bone mass. The common clinical manifestation of spinal involvement is the instability of upper cervical spine. The spontaneous cervical apophyseal joint fusion is rare and only seen in juvenile type rheumatoid arthritis, where one-or two level fusions occur in up to 41 percents of cases. Spontaneous fusions of more than three cervical segments are reported to be extremely rare.
Juvenile idiopathic arthritis (JIA) is an exclusion diagnosis that applies to any arthritis of unknown origin, persisting for more than 6 wk and with the onset before the age of 16 years.
The single mobile segment of multisegmental cervical ankylosis in JIA that produces mechanical pain and neurologic deficit should be operatively managed. Awake fiber-optic intubation can be used prior to the surgery to overcome concerns of stiff neck. Avoidance of tracheostomy enables combined anterior and posterior spinal interbody fusion without increasing the risk of wound infection. Care should be taken to restore sagittal balance.
It is a very good paper.
Manuscript source: Invited manuscript
P- Reviewer: Firstenberg MS, Jiang B, Kettering K, Najafi M, Peteiro J, Ueda H S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | Prakken B, Albani S, Martini A. Juvenile idiopathic arthritis. Lancet. 2011;377:2138-2149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 528] [Cited by in RCA: 587] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 2. | Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, He X, Maldonado-Cocco J, Orozco-Alcala J, Prieur AM. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31:390-392. [PubMed] |
| 3. | Martini A, Lovell DJ. Juvenile idiopathic arthritis: state of the art and future perspectives. Ann Rheum Dis. 2010;69:1260-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 82] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Laiho K, Savolainen A, Kautiainen H, Kekki P, Kauppi M. The cervical spine in juvenile chronic arthritis. Spine J. 2002;2:89-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Kim H, Yang DH, Kim SH, Shin YS, Ahn YH, Yoon SH, Cho KG, Cho H. Long-segment Spontaneous Cervical Arthrodesis in Juvenile Rheumatoid Arthritis. Kor J Spine. 2007;4:157-160. |
| 6. | Cabot A, Becker A. The cervical spine in rheumatoid arthritis. Clin Orthop Relat Res. 1978;130-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 7. | Hensinger RN, DeVito PD, Ragsdale CG. Changes in the cervical spine in juvenile rheumatoid arthritis. J Bone Joint Surg Am. 1986;68:189-198. [PubMed] |
| 8. | Shen FH, Samartzis D, Jenis LG, An HS. Rheumatoid arthritis: evaluation and surgical management of the cervical spine. Spine J. 2004;4:689-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 48] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Peh WC, Luk KD. Pseudoarthrosis in ankylosing spondylitis. Ann Rheum Dis. 1994;53:206-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Kanefield DG, Mullins BP, Freehafer AA, Furey JG, Horenstein S, Chamberlin WB. Destructive lesions of the spine in rheumatoid ankylosing spondylitis. J Bone Joint Surg Am. 1969;51:1369-1375. [PubMed] |
| 11. | Olerud C, Frost A, Bring J. Spinal fractures in patients with ankylosing spondylitis. Eur Spine J. 1996;5:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 105] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 12. | Chaudhary SB, Hullinger H, Vives MJ. Management of acute spinal fractures in ankylosing spondylitis. ISRN Rheumatol. 2011;2011:150484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Kim DH, Betz RR, Huhn SI, Newton PO. Surgery of the pediatric spine. Thieme medical publishers. 2008;375-379. [DOI] [Full Text] |